|
SETMA believes that the key to the future of healthcare is an internalized ideal and a personal passion for excellence rather than reform which comes from external pressure. Transformation is self-sustaining, generative and creative. In this context, SETMA believes that efforts to transform healthcare may fail unless four strategies are employed, upon which SETMA depends in its transformative efforts:
- The methodology of healthcare must be electronic patient management.
- The content and standards of healthcare delivery must be evidenced-based medicine.
- The structure and organization of healthcare delivery must be patient-centered medical home.
- The payment methodology of healthcare delivery must be that of capitation with additional reimbursement for proved quality performance and cost savings.
At the core of these four principles is SETMA"s belief and practice that one or two quality metrics will have little impact upon the processes and outcomes of healthcare delivery and, they do little to reflect quality outcomes in healthcare delivery. In the Centers for Medicare and Medicaid Services (CMS) Physician Quality Reporting System (PQRS), healthcare providers are required to report on at least three quality metrics. This is a minimalist approach to providers quality reporting and is unlikely to change healthcare outcomes or quality. PQRS allows for the reporting of additional metrics and SETMA reports on 28 PQRS measures.
SETMA employs two definitions in our transformative approach to healthcare:
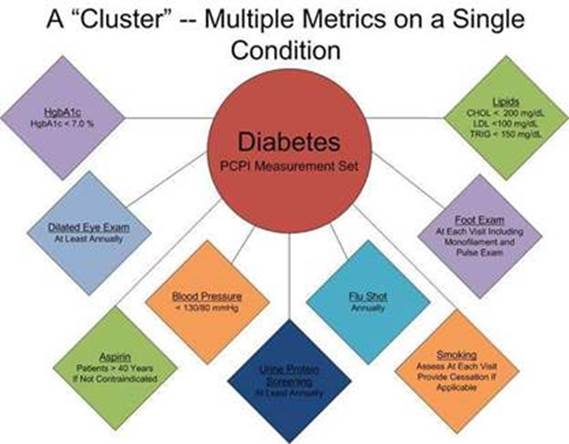
- A “cluster” is seven or more quality metrics for a single condition, i.e., diabetes, hypertension, etc.
- A “galaxy” is multiple clusters for the same patient, i.e., diabetes, hypertension, lipids, CHF, etc.
SETMA believes that fulfilling a single or a few quality metrics does not change outcomes, but fulfilling “clusters” and “galaxies” of metrics, which are measurable at the point-of-care, can and will change outcomes. The following illustrates the principle of a “cluster” of quality metrics. A single patient, at a single visit, for a single condition, will have eight or more quality metrics fulfilled for a condition, which WILL change the outcome of that patient’s treatment.
The following illustrates a “galaxy” of quality metrics. A single patient, at a single visit, may multiple “clusters” surrounding multiple chronic conditions thus having 60 or more quality metrics fulfilled in his/her care, which WILL change the quality of outcomes and will result in the improvement of the patient’s health. And, because of the improvement in care and health, the cost of that patient’s care will decrease as well.

SETMA"s model of care is based on these four principles and the concepts of “clusters” and “galaxies” of quality metrics. Foundational to this concept is that the fulfillment of quality metrics is incidental to excellent care rather than being the intention of that care.
Quality Metrics Philosophy
SETMA's approach to quality metrics and public reporting is driven by these assumptions:
- Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care.
- Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare “Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there.
- The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and patient- population data.
- There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- The collection of quality metrics should be incidental to the care patients are receiving and should not be the object of care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
The Limitations of Quality Metrics
The New York Times Magazine of May 2, 2010, published an article entitled, "The Data-Driven Life," which asked the question, "Technology has made it feasible not only to measure our most basic habits but also to evaluate them. Does measuring what we eat or how much we sleep or how often we do the dishes change how we think about ourselves?" Further, the article asked, "What happens when technology can calculate and analyze every quotidian thing that happened to you today?" Does this remind you of Einstein's admonition, "Not everything that can be counted counts, and not everything that counts can be counted?"
Technology must never blind us to the human. Bioethicist, Onora O'Neill, commented about our technological obsession with measuring things. In doing so, she echoes the Einstein dictum that not everything that is counted counts. She said, "In theory again the new culture of accountability and audit makes professionals and institutions more accountable for good performance. This is manifest in the rhetoric of improvement and rising standards, of efficiency gains and best practices, of respect for patients and pupils and employees. But beneath this admirable rhetoric the real focus is on performance indicators chosen for ease of measurement and control rather than because they measure accurately what the quality of performance is."
Technology Can Deal with Disease but Cannot Produce Health
In our quest for excellence, we must not be seduced by technology with its numbers and tables. This is particularly the case in healthcare. In the future of medicine, the tension - not a conflict but a dynamic balance - must be properly maintained between humanity and technology. Technology can contribute to the solving of many of our disease problems but ultimately cannot solve the "health problems" we face. The entire focus and energy of "health home" is to rediscover the trusting bond between patient and provider. In the "health home," technology becomes a tool to be used and not an end to be pursued. The outcomes of technology alone are not as satisfying as those where trust and technology are properly balanced in healthcare delivery.
Our grandchildren's generation will experience healthcare methods and possibilities which seem like science fiction to us today. Yet, that technology risks decreasing the value of our lives, if we do not in the midst of technology retain our humanity. As we celebrate science, we must not fail to embrace the minister, the ethicist, the humanist, the theologian, indeed the ones who remind us that being the bionic man or women will not make us more human, but it seriously risks causing us to being dehumanized. And in doing so, we may just find the right balance between technology and trust and thereby find the solution to the cost of healthcare.
It is in this context that SETMA whole-heartedly embraces technology and science, while retaining the sense of person in our daily responsibilities of caring for persons. Quality metrics have made us better healthcare providers. The public reporting of our performance of those metrics has made us better clinician/scientist. But what makes us better healthcare providers is our caring for people.
|