|
Index
- NCQA Accreditation: Benefits from SETMA’s View
- Healthcare Delivery before medical home and how it has changed since
- May 1, 1999, SETMA’s Statement about the future of healthcare
- May 1, 1999, Ten Principles enunciated for transforming practice & EHR
- Tell Us More about the SETMA Model of Care
- Noticeable Difference in SETMA before and After PC-MH
- Mistakes, Patient-Centric, Surprises about NCQA, What we know now
- Convenience is the new word for quality
- Activation, Engagement, Shared-decision making, Patient experience
- Why did you pursue NCQA Distinction in Patient Experience?
- SETMA’s CAPHS Survey Results Quarter 4, 2013
- Keeping Track of Patient Data
- Minority patient and treatment diversity
- Wall Street Journal Article Objecting to Quality metrics
- NEJM August 12, 2010 Article Poor Performance
- Treatment Inertia
- Quality Metrics General Principles
- How Can Quality Metrics Effect Quality Care?
- Precision Medicine
- SETMA’s Quality Metric Tracking, Auditing, Analyzing, Public Reporting
- Quality Metrics Philosophy
- The Limitations of Quality Metrics
- Technology Can Deal with Disease but Cannot Produce Health
- Team Approach to Healthcare Delivery
- Genesis of the Idea, May, 2013, The Automated Team
- Why Not Cheat?
- Maginot Line - Go Around Barriers
- Value Equals Quality Divided by Cost
- Complexity Demands Systemic Solutions
- How Many Tasks Can you get a provider to do?
- How can we change the future
- What advice do you have for other practices?
- It is the best known of all of the PC-MH reviewing organizations. NCQA recognition is widely recognized and is likely to continue to be dominant.
- NCQA is the publisher of the HEDIS measures which are the foundation of quality metrics of Medical Advantage STARS program and of the ACO quality metrics requirements.
- NCQA provides recognition for diabetes, heart/stroke quality and a distinction in Consumer Assessment of Healthcare Providers and Systems for Patient Centered Medical Home (AHPS PC-MH).
- Bridges to Excellence in most states provides payment for quality performance from multiple payers if practices have NCQA recognition. This will grow going forward.
- A Senior Fellow with MGMA has been commissioned by the Department of Health and Human Services’ Assistant Secretary for Planning and Evaluation (ASPE) to compare the PCMH programs. This is in preparation for CMS’s determination if one or more of the PCMH programs qualify to endorse practices to participate in the new payment system for Complex Chronic Condition Coordination payments. While others may be included, also, I think NCQA will be one of those selected, unless CMS decides to “go it alone.”
- SETMA is accredited by three of the four organizations involved in PC-MH recognition and by the end of March will be accredited by all four. While we will maintained all four for two or three, three-year cycles (we have completed NCQA Tier 3 for 2010-2013 and 2013-2016), we will certainly maintain NCQA recognition permanently.
When I started practicing medicine in 1975, primary care was high volume - which referred more to the number of patients seen, than to the number of tests and procedures ordered. At that time healthcare was paternalistic. Under the old model of care, which we might refer to as a paternalistic healthcare system, patients were very often told what to do and it was expected that they would follow the healthcare providers’ instructions without modification. The definition of “paternalism” helps understand the old model of care; it is: “A policy or practice of treating or governing people in a fatherly manner, especially by providing for their needs without giving them rights or responsibilities.”
The dynamic of the medical home redefines the relationship of healthcare provider and patient, and changes how they relate! Rather than the patient encounter being didactic (to lecture or teach, as one with knowledge instructions or informs those who do not) - where the healthcare provider tells the patient what to do, how to do it and when to do it - the patient/provider encounter becomes a dialogue (An exchange of ideas or opinions) - where the healthcare provider and the patient discuss a mutual concern and then together come to a mutual conclusion with a mutually agreed upon plan. This new relationship is somewhat like a partnership. (see more at Paternalism or Partnership: The Dynamic of the Patient-Centered Transformation)
In the mid-80s, laws changed so that primary care physicians could only charge for laboratory work which they actually performed in their offices. The sequence in which the changes were made, i.e., in July, 1984 or 85, physician fees were frozen and in August the laboratory regulations changed. For those who had not raised their fees in years and who did not over-utilize laboratory, this put tremendous financial pressure on primary care practices.
In the 1990s, managed care came to Southeast Texas and it challenged some of the fundamental assumptions we had made. In 1996, we began talking about electronic medical records, having no idea what we were talking about. In October, 1997, SETMA’s partners attended the MGMA meeting in Washington, D.C. and examined dozens of EHRs. March 30, 1998, SETMA bought the EHR which is still being used. I wrote a paper May 1, 1999, in part it stated:
“Doctors need to learn new technological ways of organizing and conducting the business of medicine. They need to allow the power of information systems to change the way they approach healthcare. They need to maintain personal contact; patients are people first and last, but doctors need to see CPR as a powerful tool and not simply as a new and expensive toy. If they do, they will begin the 21st Century with an ability to impact the delivery of healthcare in America.
“Healthcare providers must never lose sight of the fact that they are providing care for people, who are unique individuals. These individuals deserve our respect and our best. Healthcare providers must also know that the model of healthcare delivery, where the provider was the constable attempting to impose health upon an unwilling subject, has changed. Healthcare providers progressively are becoming counselors to their patients, empowering the patient to achieve the health the patient has determined to have. This is the healthcare model for the 21st Century and the computerized patient record is the tool, which makes that model possible.” (see the full text at More Than a Transcription Service: Revolutionizing the Practice of Medicine: And Meeting the Challenge of Managed Care With Electronic Medical Records (EMR) which Evolves into Electronic Patient Management)
SETMA’s evolution to a new model of care had already started in 1999. In the paper referenced above on “paternalism,” the following was included from a paper written in 1999. In speaking of transformation of our practice, we said:
“There are two aspects of this transformation. The first is structural; the second is dynamic. The structural change, being based on electronic patient records and electronic patient management of patients, is essential and in some ways it is easier than the required dynamic change. In 1999, ten years before we knew about medical home, SETMA defined both the structure and the dynamic of patient-centered medical home. We just did not know it.
“In May, 1999, SETMA defined the principles which would guide the structural changes Index four which would prepare us to become a medical home, at a time when we did not know the name or the concept. Those principles were:
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to bear upon every patient encounter what is known rather than what a particular provider knows.
- Make it easier to do it right than not to do it at all.
- Continually challenge providers to improve their performance.
- Infuse new knowledge and decision-making tools throughout an organization instantly.
- Establish and promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations of patients longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement Data Sets.
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
Remember, these principles were defined fifteen years ago. If reiterated today, they would be slightly changed but for our purposes, it is useful to see them as they were stated early in our development.”
February 16, 2009, five SETMA leaders attended our first lecture on PC-MH. It was not very helpful and did not answer our questions. The next day, I began reading and writing about medical home. Over the next sixteen weeks, I wrote an article a week about medical home. The following link is to SETMA’s website where these articles can be seen (Your Life Your Health - Medical-Home) In September, 2009, four SETMA leaders attended the NCQA PC-MH Conference in Washington where we continued to study and learn about Medical Home. Gradually, our vision and understanding of PC-MH ( a registered trademark of NCQA) deepened as we studied NCQA’s 2009 version of PC-MH standards and measures. In June of 2013, we would complete NCQA medical home recognition under the 2011 standards and received once again the Tier III Recognition.
While our use of EHR and the transformation which had already taken place in our practice enabled us to achieve Recognition, we were fully aware that we had not yet arrived. We still had a lot to learn and a lot to do. We had adopted the structure of medical home but we were only beginning to learn and practice the dynamic. Our relationship with NCQA would continue to challenge us to learn and to change so that by the time we renewed our recognition we were much more confident of our medical home. We expect that same process to continue as NCQA grows and changes, so we do. We are anticipating that by the time we renew our Recognition in 2016 and in 2019, we will be amazed at the changes and differences we will see from 2010 when we were first recognized.
SETMA believes that the key to the future of healthcare is an internalized ideal and a personal passion for excellence rather than reform which comes from external pressure. Transformation is self-sustaining, generative and creative. In this context, SETMA believes that efforts to transform healthcare may fail unless four strategies are employed, upon which SETMA depends in its transformative efforts:
- The methodology of healthcare must be electronic patient management.
- The content and standards of healthcare delivery must be evidenced-based medicine.
- The structure and organization of healthcare delivery must be patient-centered medical home.
- The payment methodology of healthcare delivery must be that of capitation with additional reimbursement for proved quality performance and cost savings.
At the core of these four principles is SETMA"s belief and practice that one or two quality metrics will have little impact upon the processes and outcomes of healthcare delivery and, they do little to reflect quality outcomes in healthcare delivery. In the Centers for Medicare and Medicaid Services (CMS) Physician Quality Reporting System (PQRS), healthcare providers are required to report on at least three quality metrics. This is a minimalist approach to providers quality reporting and is unlikely to change healthcare outcomes or quality. PQRS allows for the reporting of additional metrics and SETMA reports on 28 PQRS measures.
SETMA employs two definitions in our transformative approach to healthcare:
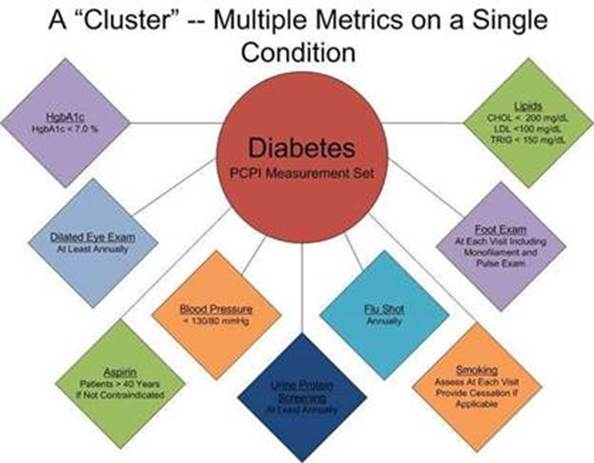
- A “cluster” is seven or more quality metrics for a single condition, i.e., diabetes, hypertension, etc.
- A “galaxy” is multiple clusters for the same patient, i.e., diabetes, hypertension, lipids, CHF.
SETMA believes that fulfilling a single or a few quality metrics does not change outcomes, but fulfilling “clusters” and “galaxies” of metrics, which are measurable at the point-of-care, can and will change outcomes. The following illustrates the principle of a “cluster” of quality metrics. A single patient, at a single visit, for a single condition, will have eight or more quality metrics fulfilled for a condition, which WILL change the outcome of that patient’s treatment.
The following illustrates a “galaxy” of quality metrics. A single patient, at a single visit, may multiple “clusters” surrounding multiple chronic conditions thus having 60 or more quality metrics fulfilled in his/her care, which WILL change the quality of outcomes and will result in the improvement of the patient’s health. And, because of the improvement in care and health, the cost of that patient’s care will decrease as well.

SETMA"s model of care is based on these four principles and the concepts of “clusters” and “galaxies” of quality metrics. Foundational to this concept is that the fulfillment of quality metrics is incidental to excellent care rather than being the intention of that care.
The SETMA Model of Care
- The tracking by each provider on each patient of the provider’s performance on preventive care, screening care and quality standards for acute and chronic care. SETMA"s design is such that tracking occurs simultaneously with the performing of these services by the entire healthcare team, including the personal provider, nurse, clerk, management, etc.
- The auditing of performance on the same standards either of the entire practice, of each individual clinic, and of each provider on a population, or of a panel of patients. SETMA believes that this is the piece missing from most healthcare programs.
- The statistical analyzing of the above audit-performance in order to measure improvement by practice, by clinic or by provider. This includes analysis for ethnic disparities, and other discriminators such as age, gender, payer class, socio-economic groupings, education, frequency of visit, frequency of testing, etc. This allows SETMA to look for leverage points through which SETMA can improve the care we provide.
- The public reporting by provider of performance on hundreds of quality measures. This places pressure on all providers to improve, and it allows patients to know what is expected of them. The disease management tool “plans of care” and the medical-home-coordination document summarizes a patient’s state of care and encourages them to ask their provider for any preventive or screening care which has not been provided. Any such services which are not completed are clearly identified for the patient. We believe this is the best way to overcome provider and patient “treatment inertia.”
- The design of Quality Assessment and Permanence Improvement (QAPI) Initiatives - this year SETMA"s initiatives involve the elimination of all ethnic diversities of care in diabetes, hypertension and dyslipidemia. Also, we have designed a program for reducing preventable readmissions to the hospital. We have completed a Business Intelligence (BI) Report which allows us to analyze our hospital care carefully.
The structural differences include that they would be given information about our medical home. They would see our mission statement and framed copies of The Baton, a depiction of the patient’s plan of care and treatment plan which is part of the dynamic of PC-MH defined by terms such as patient activation, engagement, shared-decision making, patient-centeredness, etc. Dynamically, they would experience a fundamental change in how our patient encounters are conducted with a patient-centered conversation where the patient is encouraged to “tell their story” and where attention is given to the patient’s expectation of their visit results.
They would experience the efficient fulfillment of hundreds of quality metrics which are not intrusive to the provider/patient relationship and interaction but which are supportive of it. They also now receive a document with their quality metric information which is also published publicly (without patient identifier) by provider name. Information on over 300 quality metrics for 2009, 2010, 2011, 2012, 2013 are displayed on our website. It was NCQA which motivated us to do that as one of their requirements in 2009 was that we report on 10 NQF endorsed measures to an external organization. We decided to leap over that requirement and to report publicly for all to see and not on 10 NQF measures but on over 60.
While we had taken measures to transform SETMA, we were surprised by the standards which challenged us to go further. We were challenged by the standard to put the patient in charge of their healthcare experience and we were challenged by the degree to which NCQA emphasized patient convenience. It took us a while to understand the value of convenience and coordination. Coordination” came to mean to SETMA, scheduling which translates into:
- Convenience for the patient which
- Results in increased patient satisfaction which contributes to
- The patient having confidence that the healthcare provider cares personally which
- Increases the trust the patient has in the provider, all of which,
- Increases compliance in obtaining healthcare services recommended which,
- Promotes cost savings in travel, time and expense of care which
- Results in increased patient safety and quality of care.
In February 2012, I was asked to present this concept to a Leaders and Innovators meeting under the title, Convenience Is The New Word For Quality. (HIMSS 2012: Leaders and Innovators Breakfast Meeting)
Now we know academically and practically what patient activation, engagement, shared decision making and patient-centric conversations are. We continue to study (see our provider training under Presentations on our website). In 2010, these were novel and mysterious terms to us. Our understanding can be reviewed on our website under Medical Home in an article entitled SETMA.com | Medical Home | Teaching Tool for PC-MH Course - Patient Care Activation, Engagement, Shared-Decision Making (Teaching Tool for PC-MH Course - Patient Care Activation, Engagement, Shared-Decision Making).
Perhaps the most surprising thing was the degree of contact with patients which NCQA required of practices through follow-up telephone calls and other contacts. When SETMA launched its Care Coordination Department in August of 2010 as a result of NCQA recognition, we designed tools which allowed all patient discharged from the hospital (21,000 patients over five years) to receive a Care Coaching Call the day after discharge from the hospital and which allowed providers to schedule a care coaching call with patients from the ambulatory clinic who were complex and vulnerable. Today, SETMA’s Care Coordination Department completes over 30,000 calls a year to our patients.
SETMA has done internal patient-satisfaction survey’s for 19 years. But, we always knew these were inadequate to assess the dynamic of patient-centered, medical home care. The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS, hospital setting) and the Consumer Assessment of Healthcare Providers and Systems (CAHPS, ambulatory setting) had always seemed daunting to healthcare providers. In July, 2013, SETMA had its monthly review of our quality performance in the hospital and one of the metrics is HCAHPS performance. At that time, I asked for the details on HCAPHS. Starting on July 15, 2013, SETMA launched a tracking tool in our EHR whereby HCAHPS was added to SETMA’s Care Coaching Call completed by SETMA’s Care Coordination Department. By July 30, 2013, we were completing our own HCAHPS survey. While it did not replace the hospital’s vendor produced data, it gave SETMA a quality improvement method so that we could measure our performance ( Hospital Consumer Assessment Of Healthcare Providers and Systems (HCAHPS)).
This process revealed to me the value of HCAHPS and CAHPS PC-MH in measure the patient-centeredness of our care. In August, 2013, we contracted with an NCQA certified vendor to complete quarterly surveys. The following links shows the public report SETMA did on our first quarter CAHPS survey: NCQA's New Distinction in Patient Experience Reporting. The following was reported in a Southeast Texas newspaper.
This graph is the Expanded Executive Summary of SETMA’s first quarter of our gathering of the Consumer Assessment Healthcare Providers and Services measurement of patient satisfaction. The first column is the CAHPS PCMH Benchmark from 2012 CAHPS Data. The other five columns are the results of the CAHPS survey for each of SETMA’s five clinics: SETMA 1 on Calder; SETMA 2 on College; the Mark Wilson Clinic on Dowlen; and our Mid County and Orange Clinics.
The “Noteworthy Findings” of the Expanded Executive Summary of the CAHPS survey are that SETMA’s “results are not significantly different in any of the categories“ from the Benchmarks. This means that SETMA is doing well, however, not as well as we would like. In our January 21st Provider Training Session, we will review each of the below “composite ratings” and discussion ways in which we can improve. We expect that while we are doing “OK,” that in coming quarters, we will see significant improvement. That is the goal.
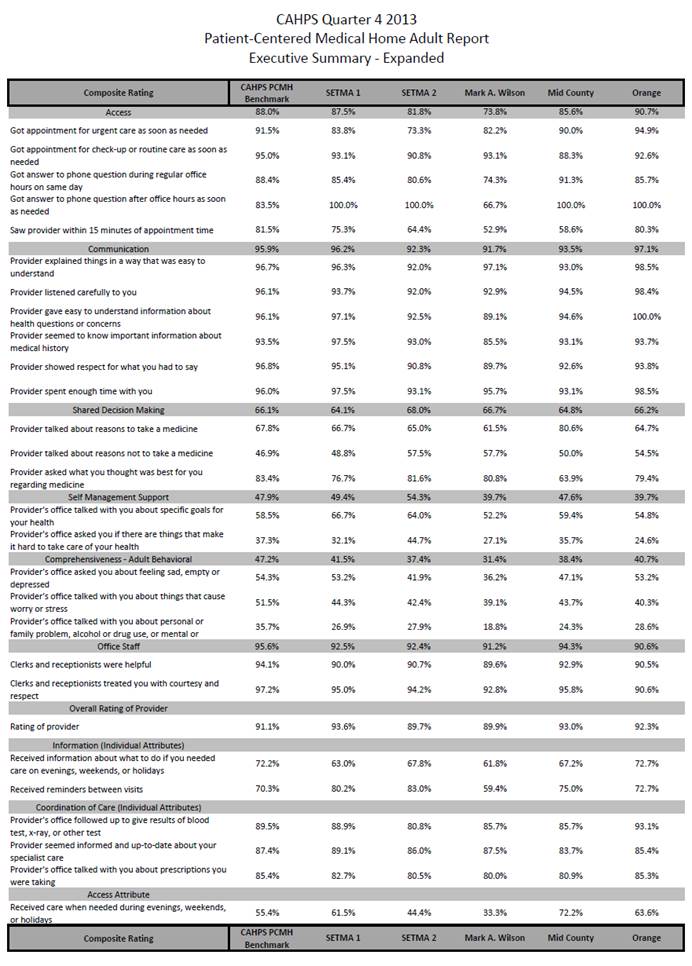
As more of SETMA’s patients participate in the CAHPS surveys and as SETMA’s providers and staff study the results, we will improve the care we deliver. Patient satisfaction is a key part of the transformation of healthcare. These surveys are providing SETMA will opportunities to improve our patient-centric care.
These are also safe guards against abuse and/or misuse of the patient-provider relationship are in place at SETMA by:
- Our Care Coordination Department’s completion of the Hospital Consumer Assessment of Healthcare Providers and Services (HCAHPS) on every patient who leaves the hospital. An explanation of this program is made on SEMTA’s website for review by our patients and community at Hospital Consumer Assessment Of Healthcare Providers and Systems (HCAHPS).
- SETMA’s employment of an independent, NCQA-endorsed agency for the quarterly completion of the Consumer Assessment of Healthcare Providers and Systems (CAHPS). An explanation of this program is made on SETMA’s website for review by our patients and community at Consumer Assessment of Health Care Provider and Systems.
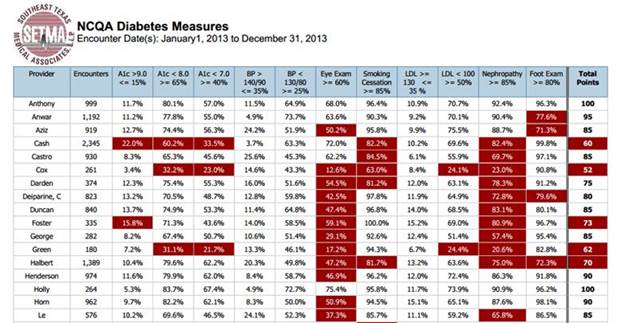
SETMA deployed a Business Intelligence program which we customized for healthcare analytics. Quarterly, we post our quality data on our website. We have five years of data identified by provider name and have started our sixth year. The following NCQA report takes 23 seconds to produce making data tracking very easy.
SETMA is a multi-ethnic, multi-cultural, multi-faith practice. This is true among the partners, the providers, the patients, and the management of SETMA. As a result, we are particularly sensitive to disparities in access to care, or in the outcomes of care for any group regardless of a discriminator which may describe or define any person or group of persons. There is no place this is truer than in the case of ethnicity. While nationally there are significant disparities of care between various racial groups, SETMA has worked hard to eliminate those differences.
With SETMA's COGNOS Project (see www.jameslhollymd.com Your Life Your Health under COGNOS Project), we are now able to understand the processes and outcomes of the care we delivery to all of our patients and to compare those processes and outcomes by ethnic groups, gender groups, socio-economic groups and other categories. The following are SETMA's results for treating 6,238 patients with diabetes. The goal is to successfully treat all patients with diabetes to goal and to eliminate totally ethnic disparities in the care of diabetes. SETMA's results are good and do demonstrate that ethnic disparity of care has been dramatically decreased particularly in the care of diabetes.
Diabetes
For an analysis of ethnic disparities, our data for the treatment of diabetes for the past twelve months is as follows:
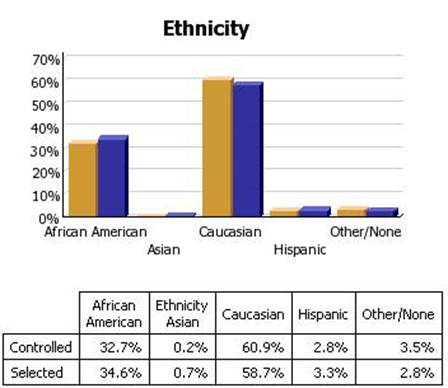
Before the judgment is made that Caucasians receive significantly better healthcare, the bar graph must be described.
- 3783 patients seen by SETMA providers in the past twelve months had diabetes.
- As a percentage of the 3783 patients with diabetes 1,323 were controlled. (For this audit, "controlled" is defined as the patient having had a HgbA1C below 6.5 % for the entire year.) If, as in the case of the National Quality Forum (NQF) Comprehensive Diabetes Measurement Set, "controlled" were defined as below 7% and the measure called for an examination only of the most recent HgbA1C, the percentage of those designated as "controlled" would rise to 59.9%.
- 60.9% of the patients who had diabetes and who were seen in the past twelve months and whose HgbA1c was below 6.5% for the entire year, were Caucasians
- 32.7% of African American treated by SETMA who had diabetes, who were seen in the past twelve months and who had HgbA1C had a HgbA1C continuously below 6.5%.
- The second classification on this graph is entitled "selected." In the case of the above bar graph, "selected" refers to all patients whose diabetes, at any point in the year, was above 6.5%. There were 2460 of them.
At first glace, it might be assumed that the care of Caucasians was twice as good as that of African Americans. But note that the percentage of "controlled" and "Selected" is not of a subset but a percentage of the same whole. As a percent of the whole, SETMA treats twice as many Caucasians as African Americans. As a percent of those who exhibited continuous control of their diabetes, it is the same proportion of African American as Caucasian. Their treatment judged by process measures or by outcomes measures is identical. The conclusion is that the ethnic distribution of all of SETMA's patients with controlled diabetes is nearly identical to the ethnic distribution of SETMA's patients with uncontrolled diabetes.
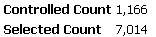
Cholesterol (Dyslipidemia)
In the case of the treatment of cholesterol (dyslipidemia), the case for the elimination of ethnic disparities of care is not as clear. In the current audit the definition of "controlled" for lipids is a Low Density Lipoprotein (LDL) below 70 mg/dl.
As can be seen by the bar graph below, there is a statistically significant disparity in the care of African Americans with dyslipidemia. Because we have eliminated the financial barriers of access to care for our patients, we recognize that the remaining disparity has to do with life-style, cultural and socio-logical problems. All for which we are working to design solutions. These data represent a total of 8,170 discreet patients with the diagnosis of dyslipidemia.
Approximately 23% of those number are African American and slightly over 70% are Caucasians.
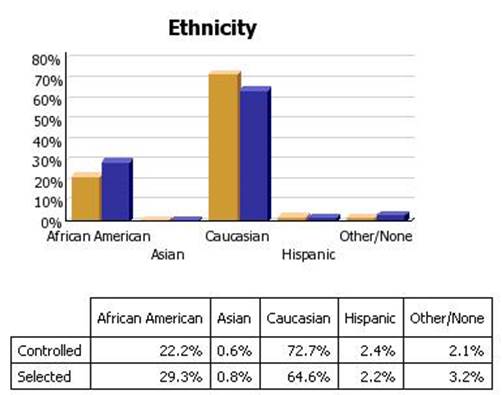
Hypertension
The same explanation applies to hypertension. The goal is to have blood pressure below 130/90 which is defined as "controlled." Again, this audit is displays as "controlled" only those patients whose blood pressure is below 130/90 for the entire year. If we changed the auditing criteria to the last blood pressure being below 130/90, the "controlled" group would rise to over 70%. A total of 8,180 patients where seen in the past 12 months with the diagnosis of hypertension.
Approximately 9,632 discreet patients with hypertension were treated at SETMA in the past twelve months. 6,476 of them had blood pressure readings consistently below 130/90. 3,156 had at least one reading above 130/90.

This disparity is less than that of dyslipidemia but it still exists.
We are designing education programs, dietary management programs and other interventions in an attempt to overcome the remaining disparities in the outcomes of our care of African Americans with these serious health problems.
I totally disagree with this A well-designed EHR allows quality data to be collected incidental to excellent care. She implies that the intent of quality care is to track and measure quality metrics. That is not the case. Due to a bad experience or an inadequate EHR design she thinks that her perception is correct. However, it is not a failure of the method but of the practice deployment of the EHR with which she is experienced. This is a link to my response to an article in the New England Journey of Medicine objecting to quality metrics: Response to New England Journal of Medicine on Quality Metrics by James L. Holly, MD
The article from the August 12, 2010, New England Journal of Medicine was sent to me by a friend who is an outstanding physician and a leader in quality improvement in medicine. A brief note was attached which stated, "This is more my bias." As I read this "perspective piece," I felt the angst of the physician whose clinical support and treatment resources are limited. I was not concerned that the physician's quality metrics were not good, none of us can claim not to have been surprised with the objective evidence that we are not doing as well as we hoped and as we wanted in the treatment of our patients. The disturbing thing about the "perspective" is that with the quality outcomes not improving from year to year, the physician expressed no alarm, and apparently rather than looking for ways to improve, chose to attack the quality-metric process. The poor "report card" which the physician received is not nearly as important as the fact that treatable disease processes continue to ravage her patients without any expressed plans by the physician to improve her performance, and thereby improve patients' health.
Treatment, or clinical inertia is well documented in the medical literature. Practice administrations struggle with methods for overcoming this barrier to effective care. The tendency of physicians not to change a treatment plan when a patient is not moving toward or reaching a treatment goal is a problem for large medical organizations, for healthcare centers and for small group or solo practicing physicians. Nevertheless, the audacious declaration by this physician that her documented, continuing poor treatment outcomes only makes this physician hold those who design quality measures in contempt is a new twist in treatment inertia, a twist for which there is no obvious solution.
Healthcare delivery in America must change and the attitude reflected in this perspective is one illustration of why that change may have to come from political pressure, if the medical profession does not effect real change internally. When I started my medical career in 1969, there was no effective way of measuring quality other than by tedious chart reviews which were expensive and time consuming. Now, due to technology, we can measure performance in real time. To ignore that measurement is not an acceptable alternative.
No one would argue that quality metrics are the only solution to healthcare improvement. Those who grapple with the design of quality metrics do not sit around thinking up new ways to aggravate healthcare providers. Using scientific methodology and a growing body of medical literature on quality metrics, these pioneers look for leverage points in identifying potential for real change in healthcare-delivery processes, which will reflect real change in the quality of patient health. Unfortunately, quality metrics are not static such that once you identify one metric that it will have permanent relevance to quality improvement. Once processes are in place, such that the outcomes are virtually totally dependent upon the process, rather than healthcare provider performance, new metrics must be found to move the system further toward excellence.
A single quality metric for a complex disease process will have little if any impact upon patient safety and health. And, all quality metrics of value should point to treatment change which will improve patient health. Though a single metric is of extremely limited value, a "cluster," or a "galaxy" of quality metrics can effect real change in healthcare quality and in patient health. A "cluster" is defined as a group of quality metrics (seven or more) which define quality treatment standards in both process and outcomes for a single disease process. "Comprehensive quality measures" for diabetes are a good illustration. Unfortunately, PCPI, NQA, NCQA Diabetes Recognition, AQA, PQRS, HEDIS and Diabetes Center of Excellence, all have comprehensive quality measures for diabetes; and, they are all different.
A "galaxy" of quality measures is a group of "clusters" which relate to the health of a single patient. When "comprehensive quality measures" for diabetes, hypertension, dyslipidemia, CHF, Chronic Stable Angina, Cardiometabolic Risk Syndrome, Chronic Renal Disease Stage 1-III and then Stages IV-ESRD are identified and measured for a single patient, the successful meeting of those metrics, which may exceed 50 in number, WILL reflect quality treatment and WILL result in improved health.. Quickly, physicians will say, "But, that will take a two-hour visit for each patient." That would be the case if we were using paper records; if fact, two hours by paper may not be enough time to accomplish all of this. However, with electronic patient management via a well-designed electronic patient record, and with a well-trained and highly functioning healthcare team, this "galaxy" of metrics can be met within in the time and economic constraints currently existent in healthcare in the United States.
While quality metrics will always reflect quality, they will not always effect quality unless they are transparent to the healthcare provider at the time and point of a patient encounter. A "report card" delivered retrospectively, six months to two years after the care event which was measured, will have absolutely no impact on provider behavior. But, if the provider is able to "see" his/her performance at the time of the patient encounter, behavior will begin to change. And, if the panel or population a single provider manages, or participates in managing, has data aggregated daily, monthly, quarterly and annually, treatment inertia can be overcome. And, finally, when that provider's performance is publicly published by provider name, treatment inertia will disappear.
In a June 3, 2010, article entitled "The SETMA Model of Care - Diabetes Precision Medicine, Quality Performance," (see www.jameslhollymd.com), the limitations of quality metrics were address. That article stated in part:
"Even as we want to talk about 'precision medicine' and even as we want to measure quality using quantifiable processes and outcomes, we still have to admit that there are limitations to quality metrics. Because healthcare does not deal with machines but with people, there will always be subjective, poorly quantifiable elements to quality in healthcare. This question of the balance between technology and humanity was the subject of Your Life Your Health, May 6, 2010. It can me read at www.jameslhollymd.com under Your Life Your Health.
"There are several critical steps which can help bridge the gap between quality metrics and true quality in healthcare. These were discussed in the April 22, 2010, Your Life Your Health. Part of that discussion addressed the place of patient-centered medial home, Medicare Advantage health plans, and Evidenced-based medicine.
"...At the foundation of quality healthcare, there is an emotional bond - a trust bond -between the healthcare provider and the patient. It is possible to fulfill all quality metrics without this bond; it is not possible to provide quality healthcare without it. That is why the patient-centered medical home (PC-MH), coupled with the fulfilling of quality metrics is the solution to the need for quality healthcare.
"The genius of PC-MH is to discover the true implications of SETMA's motto which was adopted in August, 1995, which is, 'Healthcare Where Your Health is the Only Care'" It is to put the patient and their needs first. And, it is to include the patient as a member of the healthcare team. There are 8,760 hours in a year. If responsibility for a patient's healthcare is seen as a 'baton,' the patient carries that 'baton' for over 8,700 hours a year. PC-MH promotes methods for effectively 'passing the baton' to the patient so that the patient's healthcare does not suffer under the patient's own supervision. SETMA has placed the patient's healthcare at the center of our healthcare delivery in many ways. One way is that we developed The SETMA Foundation, through which we help provide funding for the care of our patients who cannot afford it. Our resources are meager in comparison with the need, but it is a start.
"The following is one example of how PC-MH and the SETMA Foundation have worked together to produce quality healthcare. A patient came to the clinic angry, hostile and bitter and was found not to be a bad person but to be depressed because he could not work, could not afford his medication and was losing his eye sight. He left the clinic with The Foundation paying for his medications, giving him a gas card to get to our ADA certified DSME program, waiving the fees for the classes, helping him apply for disability, and getting him an appointment to an experimental program for preserving his eyesight. He returned in six weeks with something we could not prescribe. He had hope and joy. By the way, his diabetes was treated to goal for the first time in years. This is PC-MH; it is caring and it is humanitarianism.
"...As the Patient-Centered Medical Home is restoring the personal aspect of healthcare, the Medicare Advantage (MA) program and/or the Accountability of Care Organizations (ACO) are modifying the 'piece' payment system of healthcare. While the President has been convinced that Medicare Advantage is the problem; it is the solution. The supposed increase in the cost of Medicare Advantage is because it is being compared to traditional Medicare costs where the administrative cost of Medicare is not calculated in the formulae. There are bright examples of success with Medicare Advantage, success marked by quality outcomes and high patient satisfaction. That success also is marked by a dramatic change in the trajectory of health care cost while maintaining its quality.
"The third piece to true healthcare transformation is including quality process and quality outcomes in the payment formula. There are fledgling programs such as the Physician Quality Reporting System (PQRS) where healthcare providers are being paid for the demonstration of quality outcomes rather than just for piece work. The accountability of the public reporting of provider performance on quality measures completes this picture. This is why SETMA has begun quarterly reporting on our website of our providers' performance on multiple quality metrics. Included in that reporting is the examination of whether disparities of care in ethnic and socio-economic groups have been eliminated.
"...Quality healthcare is a complex problem. Measureable processes and outcomes are only one part of that complexity. Communication, collaboration and collegiality between healthcare provider and patient, between healthcare provider and healthcare provider, between healthcare providers and other healthcare organizations are important aspects of that complexity also. Data and information sharing within the constraints of confidentiality add another layer of complexity. All of these aspects of healthcare quality can be addressed by technology but only when that technology is balanced by humanitarianism.
"The good news is that the right questions are being asked and historically in that setting .the right answers have been found."
Conclusion
Physician hubris or stubbornness may reject quality metrics for a while, but patient and societal demands will rightly press for change. I am confident that the author of the attached perspective piece is a "good doctor" and cares about her patients. Unfortunately, caring in the 21st Century will no longer be measured by personality or friendliness, it will be measured by competence which will increasingly be an objective measurement. To reject that reality is to prepare oneself for obsolescence when that is not necessary.
Without intrusion into the patient/provider interaction or relationship, SETMA currently tracks the following:
- 34 NCQA HEDIS measures;
- 14 NCQA Diabetes Recognition Metrics;
- 35 NQF-endorsed measures;
- 27 PQRS measures;
- 9 PCPI measures related to the physician role in hypertension management;
- 43 measures of the Bridges to Excellence program for Asthma, Chronic Stable Angina, Congestive Heart Failure, COPD, Diabetes and Hypertension;
- 10 PCPI related to Diabetes;
- 6 PCPI for Stages 4 and 5 of Chronic Kidney Disease;
- 5 PCPI for Chronic Stable Angina;
- 7 PCPI for Congestive Heart Failure;
- 20 PCPI Transition of Care measures.
SETMA's approach to quality metrics and public reporting is driven by these assumptions:
- Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care.
- Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare “Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there.
- The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and patient- population data.
- There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- The collection of quality metrics should be incidental to the care patients are receiving and should not be the object of care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
The New York Times Magazine of May 2, 2010, published an article entitled, "The Data-Driven Life," which asked the question, "Technology has made it feasible not only to measure our most basic habits but also to evaluate them. Does measuring what we eat or how much we sleep or how often we do the dishes change how we think about ourselves?" Further, the article asked, "What happens when technology can calculate and analyze every quotidian thing that happened to you today?" Does this remind you of Einstein's admonition, "Not everything that can be counted counts, and not everything that counts can be counted?"
Technology must never blind us to the human. Bioethicist, Onora O'Neill, commented about our technological obsession with measuring things. In doing so, she echoes the Einstein dictum that not everything that is counted counts. She said, "In theory again the new culture of accountability and audit makes professionals and institutions more accountable for good performance. This is manifest in the rhetoric of improvement and rising standards, of efficiency gains and best practices, of respect for patients and pupils and employees. But beneath this admirable rhetoric the real focus is on performance indicators chosen for ease of measurement and control rather than because they measure accurately what the quality of performance is."
In our quest for excellence, we must not be seduced by technology with its numbers and tables. This is particularly the case in healthcare. In the future of medicine, the tension - not a conflict but a dynamic balance - must be properly maintained between humanity and technology. Technology can contribute to the solving of many of our disease problems but ultimately cannot solve the "health problems" we face. The entire focus and energy of "health home" is to rediscover the trusting bond between patient and provider. In the "health home," technology becomes a tool to be used and not an end to be pursued. The outcomes of technology alone are not as satisfying as those where trust and technology are properly balanced in healthcare delivery.
Our grandchildren's generation will experience healthcare methods and possibilities which seem like science fiction to us today. Yet, that technology risks decreasing the value of our lives, if we do not in the midst of technology retain our humanity. As we celebrate science, we must not fail to embrace the minister, the ethicist, the humanist, the theologian, indeed the ones who remind us that being the bionic man or women will not make us more human, but it seriously risks causing us to being dehumanized. And in doing so, we may just find the right balance between technology and trust and thereby find the solution to the cost of healthcare.
It is in this context that SETMA whole-heartedly embraces technology and science, while retaining the sense of person in our daily responsibilities of caring for persons. Quality metrics have made us better healthcare providers. The public reporting of our performance of those metrics has made us better clinician/scientist. But what makes us better healthcare providers is our caring for people.
The ideal setting in which to deliver and to receive healthcare is one in which all healthcare providers value the participation by all other members of the healthcare-delivery team. In fact, that is the imperative of Medical Home. Without an active team with team-consciousness and team-collegiality, Medical Home is just a name which is imposed upon the current means of caring for the needs of others. And, as we have seen in the past, the lack of a team approach at every level and in every department of medicine creates inefficiency, increased cost, potential for errors and it actually eviscerates the potential strength of the healthcare system.
Why is this? Typically, it is because healthcare providers in one discipline are trained in isolation from healthcare providers of a different discipline. Or, they are in the same buildings and often are seeing the same patients but they rarely interact. Even their medical record documentation is often done in compartmentalized paper records, which are rarely reviewed by anyone but members of their own discipline. This is where the first benefit of technology can help resolve some of this dysfunction. Electronic health records (EHR), or electronic medical records (EMR) help because everyone uses a common data base which is being built by every other member of the team regardless of discipline. While the use of EMR is not universal in academic medical centers, the growth of its use will enable the design and function of records to be more interactive between the various schools of the academic center.
And, why is that important? Principally, because more and more healthcare professionals are discovering that while their training often isolates them from other healthcare professionals, the science of their disciplines is crying for integration and communication. For instance, there was a time when physicians rarely gave much attention to the dental care of their patients, unless they had the most egregious deterioration of teeth. Today, however, in a growing number of clinical situations, such as the care of diabetes, physicians are inquiring as to whether the patient is receiving routine dental care as evidence-based medicine is indicating that the control of disease and the well-being of patients with diabetes is improved by routine dental care. Also, as the science of medicine is proving that more and more heart disease may have an infectious component, or even causation, the avoidance of gingivitis and periodontal disease have become of concern to physicians as well as dentist.
In 1993, John Patrick set IBM on another course and changed the company's future. Reading his story made me wonder, is it possible for SETMA to set medicine on another course and to change the future. John did not want people to work “collaterally,” side by side, maybe going in the same direction, maybe even having the same goal, but working independently and at best in a cooperative manner; he wanted people to work “collaboratively,” synergistically, leveraging the generative power of a team in creating a new future which they partially envision but which even they could not control.
What can we do today in healthcare which would mirror the changes IBM experienced? How can we change “collaterallists” into “collaborativists”? How can we use the power of electronics, analytics, and informatic principles to energize radical change to create a new future in healthcare? Testing and measurement is a science. In most industries, quality is determined by testing performance. But, in healthcare we are involved in a new kind of “testing.” The tests used to measure the performance of healthcare providers are unique. Therefore, if you are going to measure the quality of care given by healthcare providers:
- If we are going to give a test to healthcare providers, and
- if we are going to give them the test questions before hand, and
- if the test is open-book, and
- if there is no time limit for taking the test;
Look up the answers before the test so providers can know their performance before they get the test results. Don’t wait until an insurer, an ACO, or an agency measures your HEDIS performance. Know your performance by measuring your performance yourself. In fact, know your performance at the time you see a patient. The ultimate “game changer” in healthcare is when the provider knows how he/she is doing in the care of an individual patient, or in the care of a panel or population of patients and then when the provider turns around and shares this information with patients and with the public at large. The game is changed because the motivation to improve is maximized.
There is no cheating!
Of course, ethically there is no “cheating” in this context. Unlike traditional medical-education tests, this test is not measuring what you know; it is measuring what you have access to and it is measuring to what you pay attention. It is measuring how efficiently and excellently you are applying what you know. The test is not measuring what you remember; it is measuring what you are reminded of. If you have Clinical Decision Support (CDS) which remind you of what needs to be done and if you have CDS tools which allow you to measure your own performance at the point of care, you can consistently improve your performance.
In April, 2013, after a three and a half hours presentation of SETMA’s system to eight Medicare Advantage executives, they asked how they could get other providers to perform as well as SETMA. They were told to develop leaders who will help improve the processes and outcomes of care, but that they must recognize also that some times physician leaders use their positions to resist, or to obstruct change rather than to facilitate it. This is not unlike the French Government after World War I.
Determined never to be invaded by Germany again, in the 1930s the French constructed a fixed, defensive fortification between France and Germany called the Maginot Line. The French did not know what General George Patton intuitively knew. In an era of mechanized warfare, fixed fortifications could be and were easily ignored. The enemy went around the Maginot Line. Similarly, when the barrier to healthcare improvement is created by the refusal of healthcare providers to accept new realities and new standards of care, health systems will simply go around them. The intent is to make the obstructing providers irrelevant to the process. The reality is if healthcare providers become fixed fortifications against the future, the process and the system will go around them.
In addition to healthcare providers obstructing the process, there is also the fact that excellent healthcare makes much greater demands of healthcare providers now than ever before. The reality is that many of those demands can be met without active participation by the provider. For instance, one of the most complicated processes healthcare providers are asked to do is to report to the local and state Departments of Health the diagnoses of certain illnesses. In Texas there are seventy eight such illnesses. Just remembering all these conditions is daunting; add to that the need to stop in the middle of a long day to fulfill the reporting requirement is another and perhaps even bigger problem. (For an a complete explanation of SETMA’s solution to infectious disease reporting see Texas State Reportable Infectious Diseases Tutorial.
The lessons of the industrial revolution give us guidance here. Rather than handmade tools and machines made by artisans who were creative geniuses, machines were made by other machines and they were reproduced in mass. Costs went down and quality went up. so the value escalated geometrically. Apply these lessons of standardization, automation and reproducibility to healthcare, we can get to our goals much faster. Henry Ford made a new machine on an assembly line which was nothing more than a standardized, automated method for producing a product which also required human input. If healthcare providers look at every process and outcome in healthcare as a sum of that which can be automated and standardized, and of that which still requires human input, healthcare quality can improve predictably. The cost can be reduced consistently, and provider and patient satisfaction can improve. Some things in healthcare cannot yet be standardized and automated but the satisfaction of receiving the care that can be, will be increased by determining what can be automated and standardized and then by doing so.
The Texas State Health Department’s Reportable Conditions illustrates the standardization and the automation of parts of healthcare processes. Remember, “The more complex a problem is, the more systemic the solution must be.” Today, SETMA providers make a diagnosis, and when that diagnoses is one of the seventy-eight reportable conditions, automatically, the condition is reported to the state with the provider doing nothing more than making the diagnosis. If an important task is not being done either because the provider is resistant to doing it, or because the provider has “too much” to do, automate it.
That question was asked at a conference in Boston in May, 2012. There were many answers, but the question was answered by asking three other questions:
- How important is the task?
- How much time does it take?
- How much energy does it take?
If you were to create a formulae to represent this process, there would be a direct correlation between how many tasks a provider can or will do and how important the tasks are; the more important the tasks, the more tasks a provider will do. There would be an inverse relationship between how much time it takes and how many tasks will be done; the more time it takes, the fewer tasks will be done. There would also be an inverse relationship between how much energy it takes and how many tasks will be done; the more energy it takes, the fewer tasks will be done. The key to getting more done is to determine what is important and only to do that, and then to make the completion of the important tasks require less energy and less time.
Make it easier to do it right than not do it at all! Imitate Henry Ford who automated the manufacturing of automobiles with assembly lines and in so doing made it possible for those who made cars to afford to drive them. There are many aspects of patient care which can be automated. Classically, SETMA has used clinical decision support as reminders to providers, but now we are realizing that many of the tasks which were the object of CDS, actually could and should be automated, requiring no input from the provider. For instance, the value of the flu immunization is not enhanced by it being ordered by a healthcare provider, or by it being given by a registered nurse. And, the process of a flu immunization can be automated.
- When a patient is given an appointment and the system determines that the patient has not had a current flu immunization and the appointment time is in the appropriate time frame to receive the vaccine, the system should order the flu immunization, and send the order to the nurse, to the chart and to charge posting. The provider is not involved which increases the probability that it will be done.
- Additionally, the system should be programmed so that every patient who has not made an appointment in the time frame for a flu immunization should be notified electronically at the beginning of the flu-immunization season that they need to have a flu shot and toward the end of the immunization season, the system should check again to see who has not had the shot.
This principle can be expanded to all chronic conditions for which the patient is being treated and/or for all screening and preventive care the patient requires. In the future, all healthcare process will be evaluated for:
- That which can and should be automated, all based on evidence-based medicine
- That which requires human input based on patient-centered care
This will give the healthcare provider more time to focus on the patient while fulfilling the processes which we believe will improve the health (outcomes) and which will decrease the cost of excellent care. Automation of care can help healthcare providers fulfill the “triple aim.”
NCQA PC-MH Recognition is worth the process, the price, and the pain. This is the future of healthcare, and it is possible to be part of that future now. It is not easy, but it is not impossible. Measure your success by your own advancement and not by whether someone else is ahead or behind you. In the same way, share your success with others.
he following steps will help:
- Determine where you are and where you want to be.
- Select the template or model you will follow.
- Outline the steps you will take.
- Develop a timeline for completing each task.
- Be innovative. Emulate the best of others, but expand upon the work and make it yours.
- Be patient but eager.
- Enjoy what you are doing and celebrate where you are.
- Be relentless; don't give up.
|