|
Medication Reconciliation Tutorial
Systematized and Automated
Philosophy and Explanation
By James L. Holly, MD
Table of Contents
There was a time, actually quite recently, when the "magic and mystery" of medicine was considered part of the art of medicine and often actually probably made people "feel" safer. Patients had enormous trust in their physicians and looked upon them as their most favored and MOST trusted counselors. Prescriptions written in Latin were reassuring to the patient who believed that their very-well-educated physician knew more than they did because he or she could write a prescription which they, the patient, could not understand.
Most patients took one or two prescriptions a year. Today that number ranges from 25 to 44 prescriptions a year for patients 65 years-of-age and older, depending upon the State in which the patient lives. Medication regimes are much more complicated and are changed much more frequently.
In the 1940s, there were not many medications. In the Health Care financing Review (Winter, 1996/ Volume 18, Number 2, p. 15), it is stated:
"Many of the changes in clinical medicine by the early 1960s were the result of pharmaceuticals: antibiotics, psychotropics, tranquilizers, hormones, and other drugs. It was estimated that 90 percent of the drugs prescribed in 1960 had been introduced in the previous two decades and that 40 percent of the prescriptions could not have been filled in 1954."
The good news was progress increasingly made valuable and useful pharmaceuticals available for treating patients. The bad news was that more and more people were taking multiple medications, some with complicated "sig" codes (written instructions in Latin) and others with an increasing number of serious interactions and with this the potential for mistakes increased significantly. In addition, the following issues produced significant hazards in the use of medications:
- Medication interactions increased to the point to where one of the major pitfalls in dealing with these interactions was "to rely upon your memory in assessing medication interactions." There were just too many for any one person to remember all of them.
- With multiple providers prescribing medications for the same patients, the maintenance of an accurate and complete medication list became increasingly difficult until it became the single most critical and complicated problem in medical records.
- The following sequence of events in prescribing of medications was not uncommon. The provider handwrites a prescription; the patient hand carriers the prescription to the pharmacy; the pharmacist can’t read the prescription or worse yet thinks he/she can read it and gets it wrong; the pharmacist calls the doctor’s office; the office staff asks the doctor what medication he/she prescribed; the doctor does not remember and asks for the chart; the chart can’t be found or has not yet been transcribed and this goes on until sometimes it is several days before the prescription is finally obtained by the patient.
In 2010, it was reported that in the United States annually 7,000 people died due to medical errors that included misreading or otherwise misinterpreting handwritten prescriptions. The following developments created an environment where accurate medication lists in provider records and accurate understanding by patients of what medications they were to take, as well as when and how to take them, became imperative:
- The number of medications grew; today there are over 10,000 prescription medications and over 300,000 over-the-counter drugs.
- The "magic and mystery" of the medical profession decreased both because of an increasingly knowledgeable populace and because of a decreasing trust in physicians.
- More and more people were taking more and more complex medications
- Medications had increasingly serious and dangerous side effects and interactions.
- Technology created new medicines and it would take technology to keep track of them.
A major sociological shift took place in the United States as well. Demand increased to take all of the magic and mystery out of medicine. Hospitals required that abbreviations, particularly Latin abbreviations not be used in hospital records. Medication lists given to patients were required to be written in English instead of Latin abbreviation, i.e., instead of "Sig: 1 po qid," medication directions were required to be written in "Directions: one tablet by mouth four times per day."
As early as the mid, 1970s, healthcare professionals and organizations like the Institute for Safe Medication Practices (ISMP), which describes itself as "A Nonprofit organization educating the medical community and consumers about safe medication practices," began to raise the alarm about the need for safe medication practices. In a 2007 publication entitled, Protecting U. S. Citizens From Inappropriate Medication Use, ISMP stated, "3.4 billion prescriptions (were) dispensed in 2005...an increase of nearly 60% since 1995...81% of adults...take at least one medication...and 27% take five." By 2016, the number of dispensed medications rose to 4.2 billion annually.
The magic of medicine was gone and the mass of medicines had increased. Both are good things but both require new skills and attentiveness by providers. The imperative for and the complexity of “Medication Reconciliation” is the most important result of these changes. And, it is still a fact that one of the two most difficult tasks facing all healthcare providers is maintaining an accurate and up-to-date medication list on all patients.
In 2010, the National Quality Forum (NQF) published a study entitled Preferred Practices and Performance Measure for Measuring and Reporting Care Coordination: a Consensus Report. One of the critical quality measures is Medication Reconciliation. One of those measures is described as: 'The plan of care document should include essential clinical data documenting the patient's current state, including, but not limited, to problem lists, medication lists, allergies and risk factors, age-appropriate standardized clinical assessments and screening tests; immunizations status...". Repeatedly, medication reconciliation is included as an essential part of care transitions at every point whether the transfer of care was made from clinic to home, hospital to ambulatory care, emergency department to nursing home, hospital to hospice, hospital to skilled nursing facility, hospital to long term acute care or other transitions.
In 2007, the American Medical Association published its 37-page monograph entitled, The Physician's Role in Medication Reconciliation: Issues, Strategies and Safety Principles. The preface gives this warning to physicians:
"Medication Reconciliation is essential to optimize the safe and effective use of medications. It is one element in the process of therapeutic use of medications and medication management for which physicians are ultimately held legally accountable...".
The AMA documented that in between 2004 and 2005, "in the United States 701,547 patients were treated for an adverse drug event (ADE) in emergency departments and 117,318 patients were hospitalized for injuries caused by an ADE. Insulin, warfarin and other drugs that require monitoring to prevent overdose or toxicity were implicated in one of every seven ADEs treated in emergency departments." The report stated, "Interactions between prescription medications and over-the-counter (OTC) drugs, herbal preparations or supplements are a growing concern, as concurrent use can lead to serious adverse reactions." And, "in all settings of care, drug-drug interactions are significant but undetected causes of ADEs."
Steps:
- Assembling the lists of medications - notice the word is "lists," not list. In a recent meeting about a regional health information exchange (HIE) an alarm was raised by the potential need to reconcile medication lists from five to ten locations. The response was that the good news was that for the first time, all providers would know that patients were getting medication from multiple sources and providers would have access to the "real" lists for medication reconciliation.
- Ascertaining accuracy (review and compare prior and new lists)
- Reconciling medications and resolving discrepancies
- Formulating a decision, i.e., making a medical judgment, with respect to the patient's condition and medications.
- Optimizing care to best meet the patient's needs with this information.
- Checking the patient's (and/or caretaker's) understanding of their medications
- Documenting changes and providing the patient with a copy of his or her current medication list.
Principles
- Medication reconciliation is a necessary component of safe medication management. The process is ongoing and dynamic, which means it is constantly changing.
- The medication reconciliation process should be patient-centered.
- Shared accountability between healthcare professionals and patients is essential to successful medication reconciliation outcomes.
- All patients should have an accurate medication list for use across sites of care and over time.
- The medication list should not be limited to prescription drugs.
- Within all settings, the medication reconciliation process should happen at every medication encounter, regardless of the care location.
- Across all settings, the medication reconciliation process must happen at every transition in the patient's care, regardless of the care transition.
- The process of medication reconciliation is interdisciplinary and interdependent and reliant on a team approach.
- Physicians are ultimately responsible both ethically and legally for the medication reconciliations process.
- Some medication information may be emotionally or legally charged, but nevertheless significant. It may be added at the discretion of the patient or prescribing health care professional by mutual consent.
- What medications do you take? Can you tell me the names of all your medications, including vitamins, OTC drugs, supplements and nutraceuticals?
- What is it important to take your medications?
- When do you take this medication? How long have you been taking this medication? Do you have a medical condition? What medical condition(s) do you have? What did your doctor say to you about this medication?
- How do you take your medications (e.g., time of day, with food)?
- Are you taking your medications the way the doctor told you to? When was the last time you took it? When was the time before that?
- What do you do when you make a mistake? Do you every skip medication or take two when you miss a dose?
- Is your medication making you feel better or worse or no change?
- What other medications, herbals, supplement, nutraceuticals, drops or sprays are you taking? Do you take other drugs that a physician has not prescribed?
- From where do you get your medications? A local pharmacy? Mail order? The Internet? From another country? Other?
- Who buys the medications in your family? Should we talk to him or her to make sure we have a complete list of all the medicines you take?
- A Reconciled List of Medications including Over the Counter, Herbal and Supplements
- Instructions in English (not Latin) for dosage, directions and timing of prescription
- A list of the patients allergies
- The date and time of the Reconciliation
- The person who did the reconciliation
- The contact information for the Reconciliation
- Use plain, nonmedical language.
- Slow down
- Break information down, use short statements.
- Organize information into two or three key concepts, then check for understanding. Aim for a fifth to sixth grade reading level on all written information.
- Use communication aids to assist in conversations, discussions or education sessions with patients, families and care givers.
- Offer to read materials aloud and explain
- Underline, highlight or circle key points.
- Provide a trained interpreter, when appropriate.
- Use visual aids to help patients navigate the health care system and understand health information.
- Ask patients to teach-back what they were told:
- We have gone over a lot of information. In your own words, can you review for me what we have discussed? How will you make it work at home?
- Sometimes I give a lot of information. Can you let me know what you heard me say? This helps me make sure I gave you the information you want and need
Conclusion
Medication Reconciliation is hard and it is critical. The dynamic nature of medications being taken creates the complexity of maintaining and accurate lists as does the fact that most patients on multiple medications are being seen by two to seven providers annually. The probability for medication reconciliation to result in accuracy in medication administration is increased by the frequency of reconciliation being completed, particularly when each reconciliation is thorough. If a patient has ten to fifteen medication reconciliations or more per year, adverse medication events will decline and hopefully disappear. Such reconciliations are time consuming and require perseverance, but the result will be increased safety and improved care with decreased cost.
- Medications will be reconciled at the following times.
- Hospital admission
- Hospital discharge
- Care Coordination call post hospitalization care coaching calls
- Hospital Follow-up clinic visits
- Post office Care Coordination calls
- Clinic Visits
- Nursing Home Visits
- Emergency Department Visits which are not admitted to hospital
- When performing the reconciliation, staff will ensure no medications are duplicated, outdated, or omitted.
- When medications are prescribed by physicians outside SETMA, these shall be so noted on the medication template by indicating ‘‘prescribed elsewhere’.
- Over the counter medications are to be marked “prescribed elsewhere”. This makes the medications current instead of listing them by provider and having a start date of 2008 and never being updated giving the impression it is not updated.
- Patients should be given a copy of the reconciled medication list when leaving the clinic or upon hospital discharge.
In 2012, SETMA began thinking that a system’s solution (see Peter Senge, The Fifth Discipline, “The more complex a problem the more systemic the solution must be.”) to medication reconciliation would be a huge step forward in patient safety care quality and in the pursuit of the Triple Aim. Whether addressing care transitions, care coordination, hospital readmissions, or patient safety, medication reconciliation is a key element of success.
In preparation for a visit October 29-November 1, 2012 from a Robert Wood Johnson Foundation research team (see the following link for a description of their research project The Primary Care Team: Learning from Effective Ambulatory Practices (PCT-LEAP): Performance Measures Worksheet - Robert Wood Johnson Foundation), SETMA prepared a 57-page document describing SETMA’s auditing and quality programs. The link above will guide readers to that document. The document addresses SETMA’s solution to care transitions, care coordination, etc. Based on the AMA’s monograph, The physician’s role in medication reconciliation Issues, strategies and safety principles(Making Strides in Safety® program ©2007 AMA) and, AHRQ’s Medications at Transitions and Clinical Handoffs (MATCH) Toolkit for Medication Reconciliation, and other studies SETMA understood the potential benefit for a structured, systemic solution to medication reconciliation.
In addition to effective care transitions (the following link is to SETMA’s performance on the Physician Consortium for Performance Improvement (PCPI) Care Transitions Measurement Set for 2009 through 2016, PCPI Care Transitions -- the next link is to the public reporting by provider name for 2012 Care Transition Audit (Section A), SETMA has established the following steps and principles for medication reconciliation:
We think that forming a coalition with pharmacies, clinicians, patients and IT technology could result in a solution to medication reconciliations which could:
- Reduce the time involved in medication reconciliation to less than two minutes
- Advance a practice closer to perfect medication lists
- Make it easy to reconcile medications at every contact and even when the patient is not schedule for a visit.
- Increase patient safety
- If a D. Pharm consultant is involved in the process, it would even be stronger. I look forward to hearing from you.
What has brought us to this day in May, 2016?
- March 30, 1998 - Purchase of Electronic Patient Record System
- January 26, 1999 - Foundation laid and SETMA began documenting patient encounters electronically
- May 20, 1999 - SETMA realized that EMR was too expensive and too hard if all we did was document a patient encounter electronically.
- May 20,1999 - SETMA adopted Electronic Patient Management as our goal and began developing chronic disease management tools and clinical decision support
- May 20, 1999 - Defined ten principles of patient-centered medical home
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to every patient encounter what is known, not what a particular provider knows
- Make it easier to do “it” right than not to do it at all
- Continually challenge providers to improve their performance
- Infuse new knowledge and decision-making tools throughout an organization instantly
- Promote continuity of care with patient education, information and plans of care
- Enlist patients as partners and collaborators in their own health improvement
- Evaluate the care of patients and populations of patients longitudinally
- Audit provider performance based on endorsed quality measurement sets
- Integrate electronic tools in an intuitive fashion giving patients the benefit of expert knowledge about specific conditions
- January, 2000 - SETMA began auditing provider performance
- January 2004 - SETMA began using electronics to increase efficiency and excellent of care with process analysis taking complex and difficult tasks and reducing them to simple problems.
- Used electronics to improve medication management with:
- Maintaining of accurate and complete medication lists -- 1999
- E-prescribing of routine medications -- 2010
- Systematizing of Medication Reconciliation
- E-prescribing of controlled substances -- 2014
- Systemic Monitoring of patient use of opioids - 2014
- Reducing Long Term Care use of Antipsychotics - 2014
- Texas Prescription Program - Electronically verifying patient use of controlled substances - 2015.
- Collaboration with NextGen and SureScripts to create an electronic capacity for efficiency, effective and excellent medication reconciliation
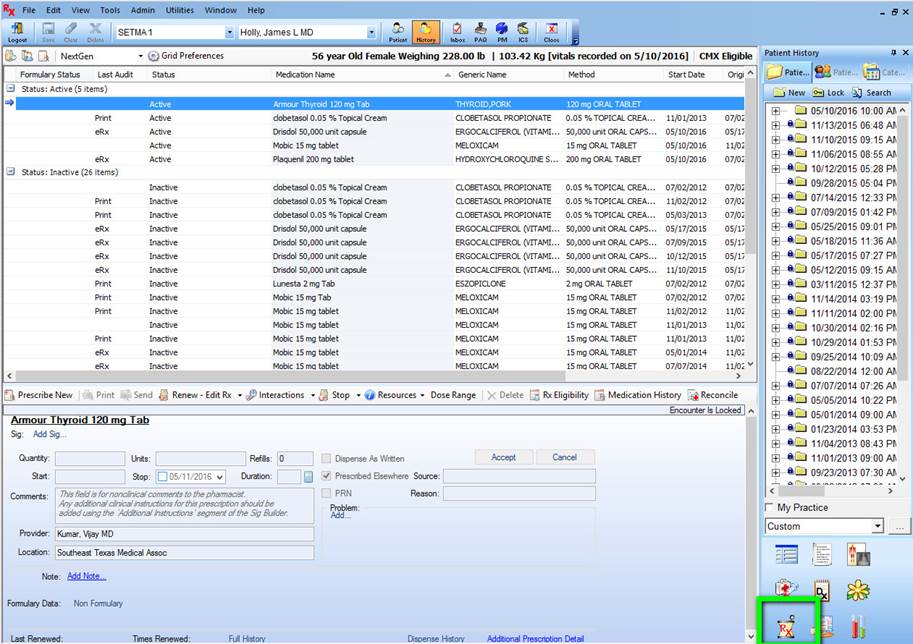
With the above conceptual foundation, most of the functions which needed can be used at present by going to the medication module by clicking on the icon outlined in green below.
Once on the medication module, you can see if this patient is eligible for use of the automated medication reconciliation by looking at the designation in green. As long as this does not read “Not Eligible” then you may use the reconciliation function for that patient.
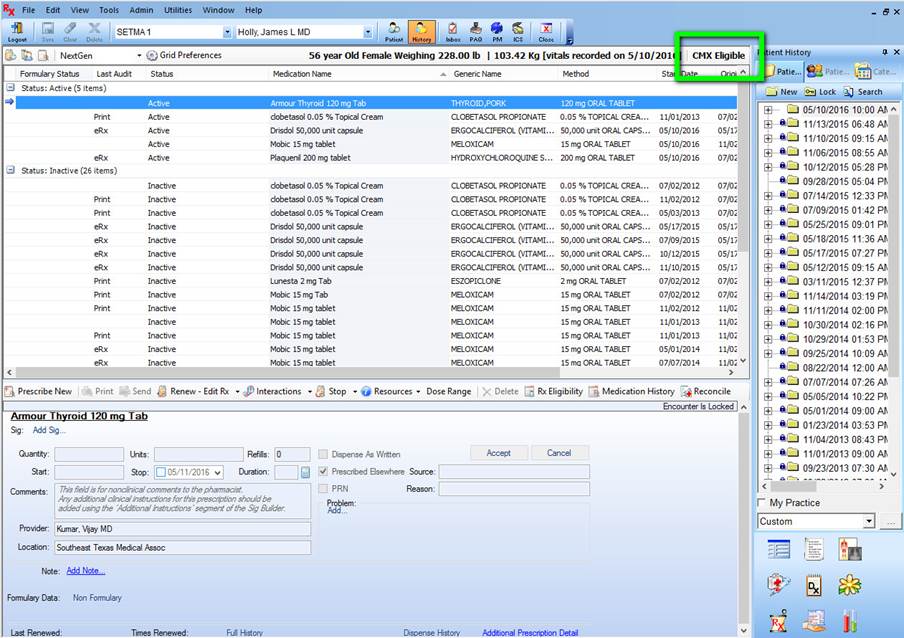
Currently, SureScripts builds their database from medications prescribed from a formulary. Some new insurance companies, such as the Affordable Care Act plans do not yet provide this information. Uninsured patients generally do not have a SureScripts database record. SETMA is currently working with SureScripts and NextGen to expand the access to patient data but what we have gets a good start.
Some medications from SureScripts have “sig” codes and some don’t. Why? SureScripts’ Medication History data consists of two datasets: 1) claims from PBMs and 2) dispensed records from pharmacies. SIG codes are contained in pharmacy dispensed records but are not contained in PBM claims. So within the overall medication list, some meds may contain SIG information and some may not.
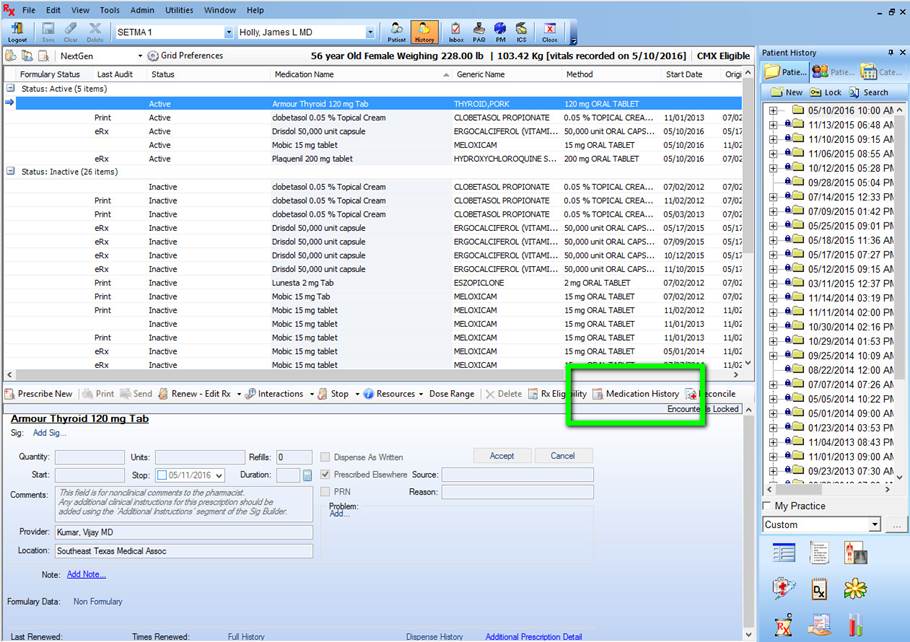
If the record shows that the pateint is eligible for medication reconciliation, you will click on the button entitle “Medication History,” seen below outlined in green.
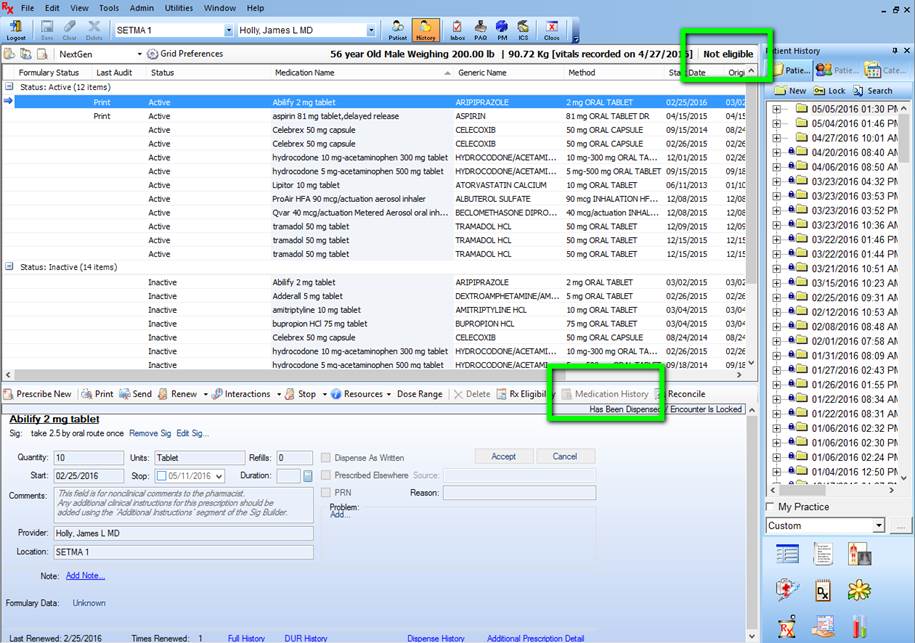
If the patient is not eligible, you will see the designation outline in green below which states, “Not Eligible” and the button “Medication History” will be grayed out.
When the patient is eligible for a “medication reconciliation, you will see the following window which states “Status: Has Not Been Requested.” In order to obtain the “medication history” from SureScripts you must complete this form.
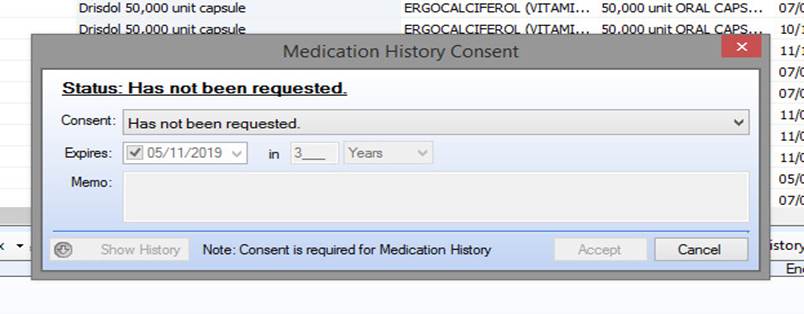
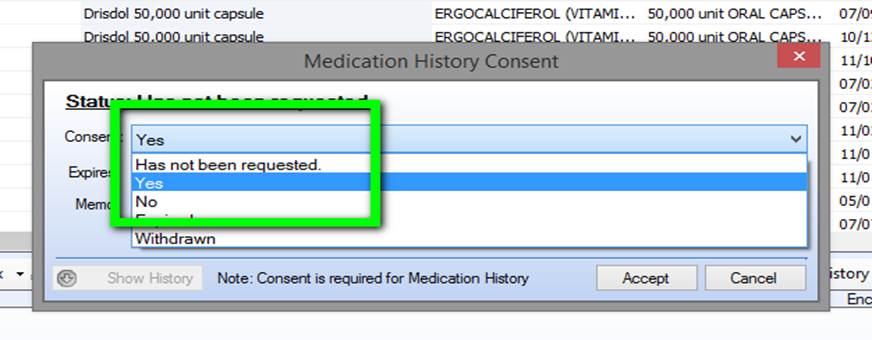
To obtain the “medication history” from SureScripts you must do three things:
- Click on the “Has not been requested” button
- Click on the “Yes” button
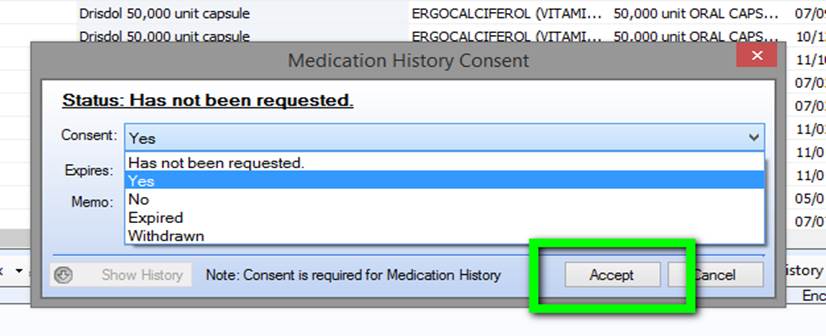
- Click on the “Accept” button out lined in the second screen below
Click on “Accept” button below outlined in green.
When you click on the “accept” button you will see the following screen which states “Queued for processing, please wait.” The first time you do the Medication Reconciliation, this will take a little longer but is very fast once you have used the function.
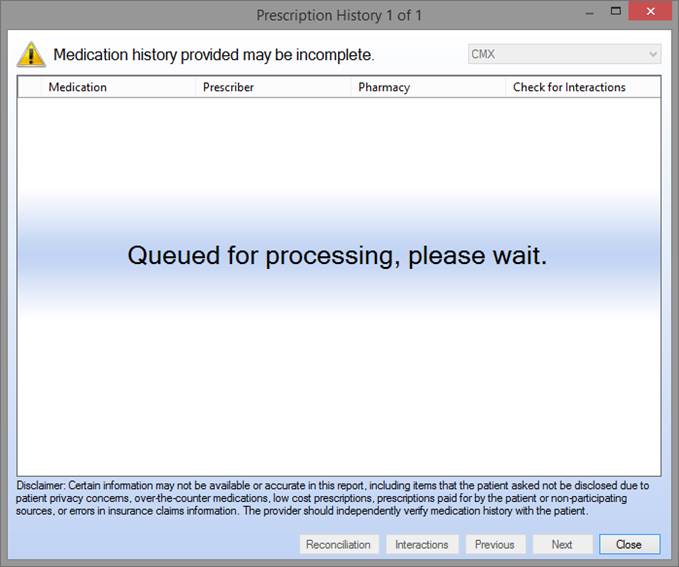
When the process is complete, you will see the following screen which gives you all the medications which this patient has received. Typically, this is up-to-date. I have had a patient who filled his medication at 4 PM the day before being seen at 8 AM the next day and the medication was in the queue.
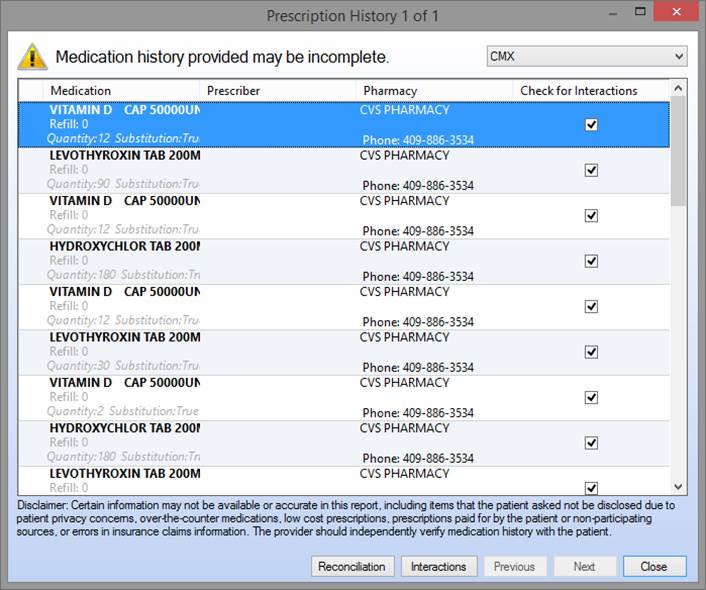
The alert “Medication history provided may be incomplete” is a disclaimer from SureScripts. You now need to click on the button outlined in green, entitled “Reconciliation.”
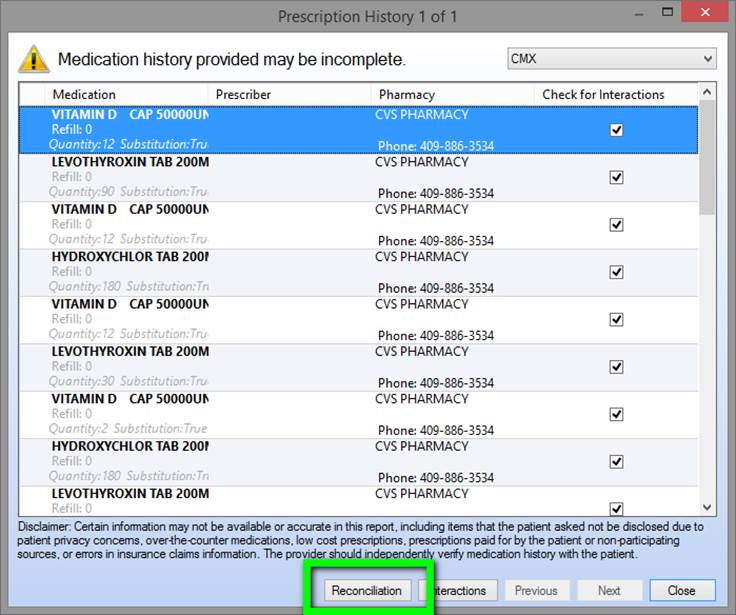
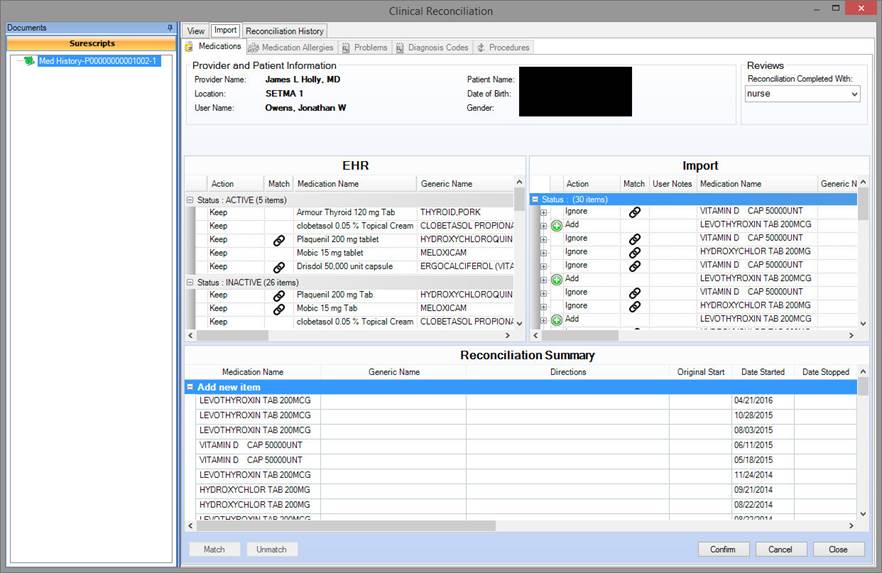
After you click this button, the system will correlate the medications in the EMR record with the medications found from SureScripts.
Those medications in the EMR and in SureScripts Medication History will be tagged with a paperclip.
There will be some medications which are not tagged. These may be duplicates or medications which have been discontinued or have been prescribed by another provider who is not in SETMA’s group.
One of the updates which SETMA has requested from SureScripts and NextGen is to collect at the bottom of the list all the medications not matched. This will make it easier to recognize which medications need your attention.
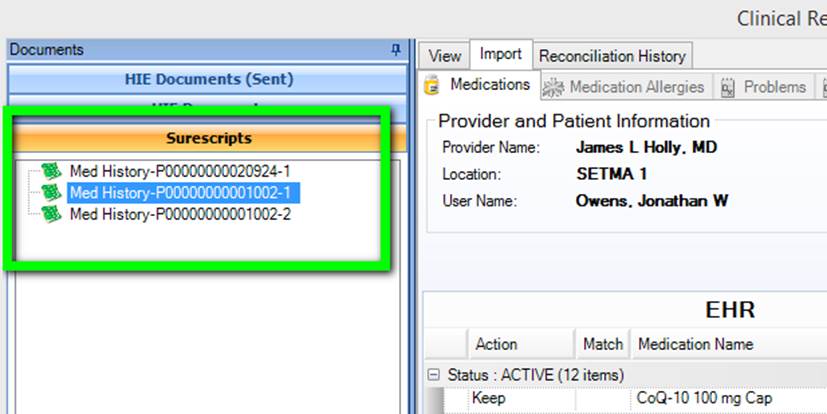
Outlined in green below is a file entitled “SureScripts Med History” with a series of numbers. A SureScripts file can only contained 50 medication events so if the patient has more than 50 there will be more than one “SureScripts Med History” list.
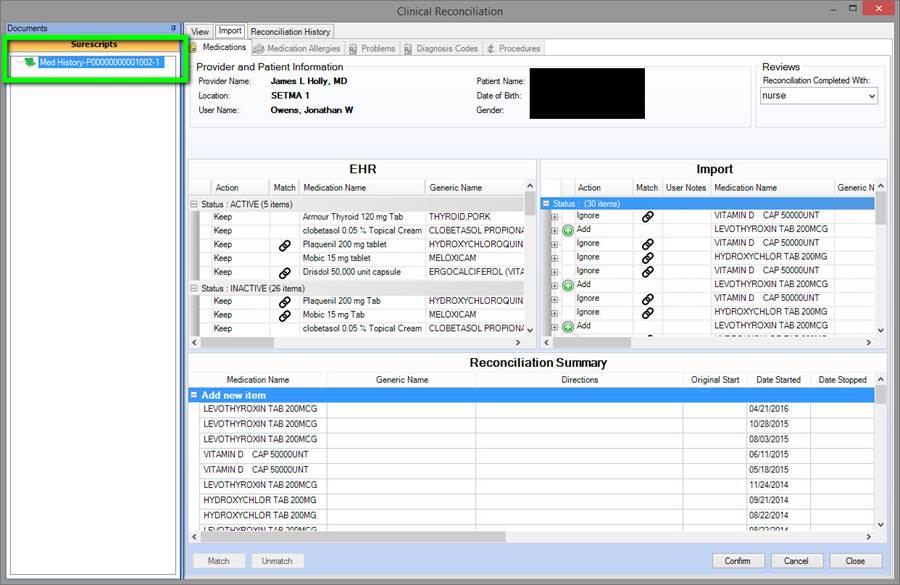
Several deficiencies presently exist which SETMA is working on with NextGen and SureScripts. One is that when you do “Medication Reconciliation” there is no foot print that you have done it. This will be discussed more later.
In the left hand screen below are the medications which appear in the EHR. The medications which are “tagged” are also found in the SureScripts Meducation history. Those which are not in the history are not tagged.
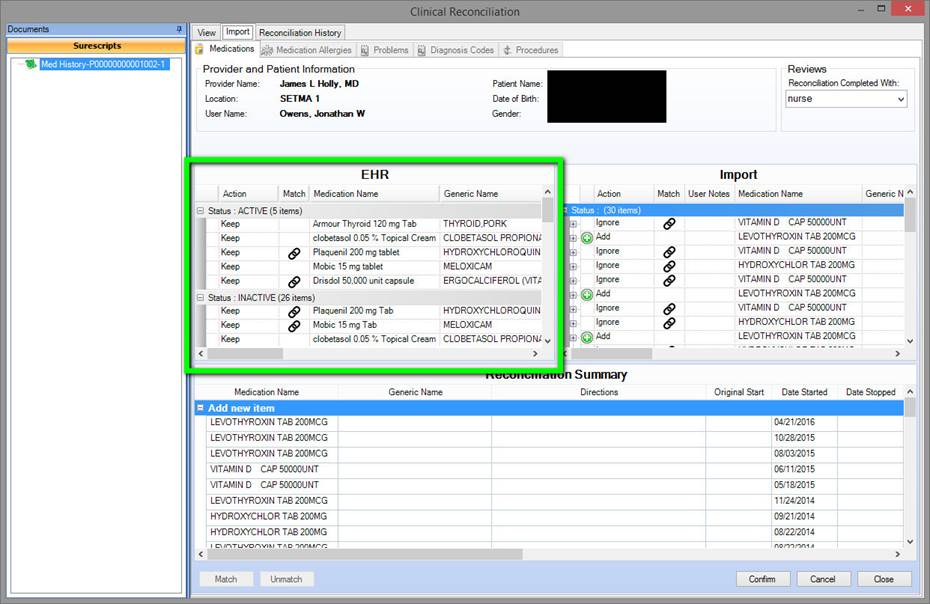
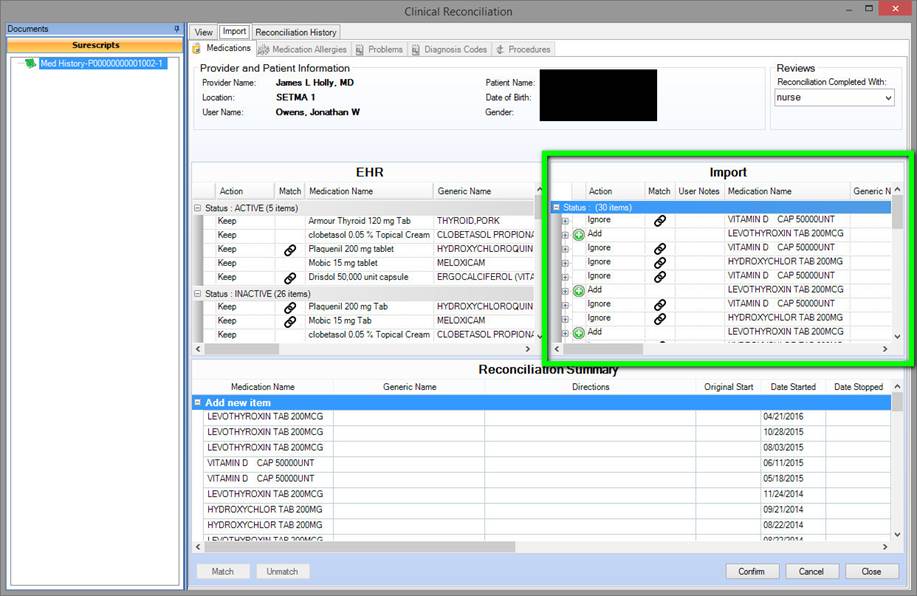
The medications in the right hand screen, outlined in green are from SureScripts.
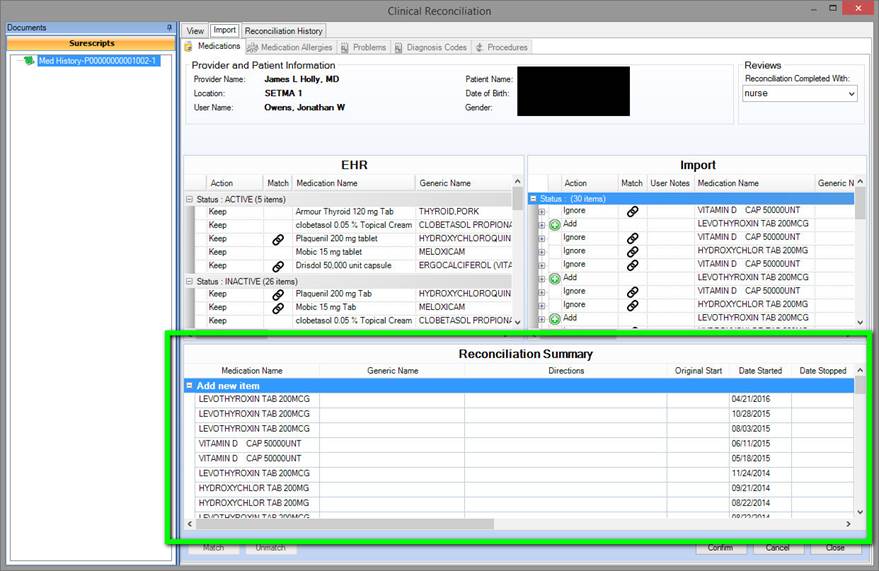
The third window outlined in green below gives you a reconciliation summary.
As is seen in the screen below, if a medication is not tagged, meaning that it does not appear in the EMR but appears in the SureScripts medication history, you need to click on the button under the “action” column where you will designate “add” or “ignore.”
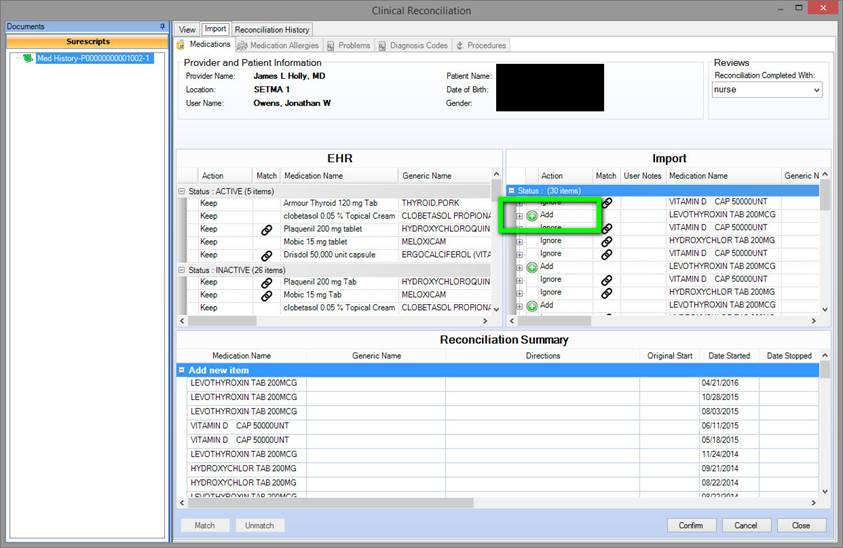
If you click “add” and if that medicine is actually a duplicate, you will be prompted with a note “Do you want to add a duplicate,” which would answer “no.” There are actually four “action” options: None Add, Ignore, Replace.
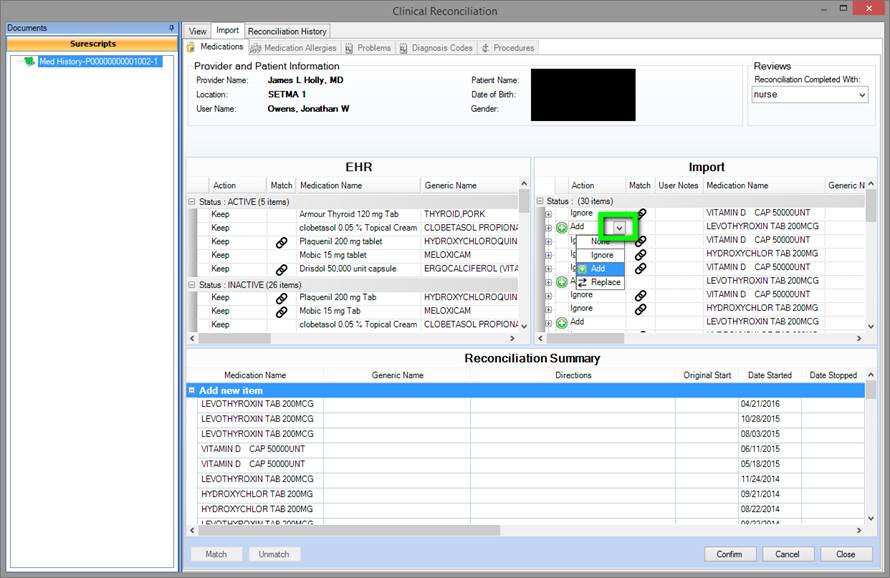
As can be seen in the screen shot below, there can be more than one “SureScripts Med History” as already mentioned above. To do a complete reconciliation, you need to go through all of the files. Generally however, you will find that only the top one or two will have medications which need to be reconciled.
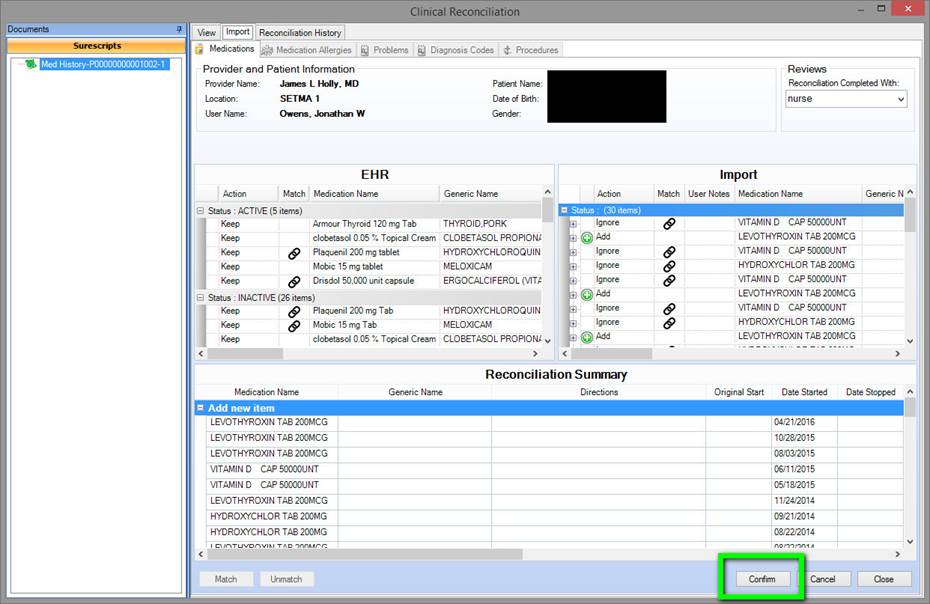
When the reconcilation process has been completed, you must click the button out lined in green below entitled, “confirm.”
The following are functions which would make NEXTGEN's excellent medication reconciliation tool much better:
- In the window on the right where the medications appear which were pulled from SureScripts, it would speed the process up considerably if the medications which do not appear in the EMR could be listed together at the bottom of the list instead of mixed in with those which are matched
- It would be helpful if duplicates with identical names, dosages and sig codes could be electronically aggregated into a single display so that the provider would not have to respond to six or seven of the same medication, same dose, etc.
- When a list of medications have been reconciled that list should be marked as reconciled
- Once an initial reconciliation has been done future queries of SureScripts should only pull information since the last reconciliation, since the last visit, or since the time frame designated by the provider, i.e., 3 months 6 months, etc.
- When there are multiple lists of medications for reconciliation, when a medication is reconciled and it appears in another list it should be electronically marked as reconciled on all lists in which it appears.
Questions
- Medications which appear in the SureScripts list which also appear in the EMR list are marked. However, there are medications on the SureScripts which are not marked as being in the EMR, but when you click the button to update, there are alerts questioning whether you want to move a duplicate into the EMR. Why would those medications not already be marked during the reconciliation process?
- Sure Scripts apparently ties their query to insurance formularies which means the uninsured medications cannot benefit from this incredibly valuable tool. Why? There are other insurance companies such as Travelers Medicare, and many of the ACA Exchange companies which are not eligible for this function. Why?
- When a new patient comes to the practice and SureScripts is queried will their medications be found and then be able to be put in EMR. See below for the fact that Sure Scripts does not bring in the number of medications and the SIG code. That would be very important to enhance this tool.
If we can get a couple of easy updates from NextGen - the Medication Reconciliation Function will be awesome
Current Functions
- A display appears with the medications listed in the EMR in a left-sided screen
- A display of the medications which SureScripts shows the patient to be on in a right-sided screen
- Each medication in the right hand screen which is in SureScripts data, which also appears in the EMR records is tagged
- Each medication in the right hand screen which is in SureScripts data, but which is not in the ERM defaults to “add” but an option for “ignore” can be selected. When the medication is added to the medication module all data comes into the record including dosage, directions, etc.
- Once the two lists are reconciled, you update the record and it is done.
Here is the powerful part of this function:
- You don’t have to go through a bag of medication bottles
- If the patient doesn’t remember the medication or the directions, you have it.
- When you have a new patient, importing the patient’s medications from Sure Scripts is very easy.
- When a medication is imported the drug, dosage, date of filling, directions of use are all automatically included.
- When you use this tool it automatically notes that you have reconciled medications.
- At present the reconciliation files only include 50 instances of medications or refills. If the patient has 500 incidents, you will have ten files to go through - unusual but possible. For instance, if the patient is on 12 medications and they are refilled every month, in a year you will have 144 incidents.
- Currently, there is no way to truncate the SureScripts reconciliation to only see the medications for the past 3, 6, 12, 18, 24 months.
- Once you have completed a reconciliation, there is no current function to note that the medications in that file have been reconciled, so the next time you reconcile the medications you will have to go back through all ten files of all 500 medications.
- In reality, once you have done a reconciliation, in the future, you would probably only want to reconcile the medications from the last time you saw the patient, whether that is six weeks, six months or six years.
With a little work from NextGen, we can get to a 90+% of what we want from Medication Reconciliation. In consultation with SureScripts, in a very short period of time, we can make this process very simply, very fast and excellent. The improvement in patient care quality and safety will be enormous
- We need a scanner in each exam room or in each pod so that then the patient brings in their “bag of medicine,” they can scan rather than transcribed into the EMR.
- If NextGen can design a solution where these scan medications can populate a third window in medication reconciliation with the names, dosages, sig codes and quantity of medications, it would allow us to reconcile EMR meds with Sure Script meds with the patient’s meds
Example from this morning: Saw an established patient today. He had not told my nurse that he saw another doctor yesterday and that he was started on a new medicine. I asked him what it was and while he was pulling out the prescription bottle, I clicked on Medication History.
Even though it was yesterday afternoon that he had the medicine filled, it was already in the list of filled prescriptions that popped up. Rather than having to put the medication into the EMR, I simply clicked on the Reconciliation button and selected “Add” medication. All details medicine, date of filling, number of medications and sig codes were added automatically.
Justin Elliott (NextGen), Ann Gallagher (NextGen), Margaret Ross (SETMA), Jon Owens (SETMA) and I (Dr. Holly, SETMA) had a very profitable conference call this morning. Based on the above file, we discussed the issues with Medication Reconciliation which are NextGen issues and things which are Sure Script issues.
The following were discussed as essential elements of expanding the use of and the usefulness of Medication History which collects Sure Script data and Reconciliation which correlates the EMR Medication Module and the Sure Script data. We identified the following as of great value:
- Including all medications which patients are obtaining.
- Including SIG codes for all medication including PPM.
- Giving the provider the option of reconciling only: medications obtain since the last reconciliation, since the last visit, or in a designated period of time such as 3 months, 6 months. Etc.
- Depending on the length of time since the medication reconciliation has been done there may be multiple files in the Clinical Reconciliation Sure Scripts Med History Lists. This is because Sure Scripts can only include 50 medication events in each file. If the patient is on multiple medications, there may be as many as ten such files. Currently, if a provider goes through all of these files, there is no notation made that all ten files (with 50 medications event in each file) have been reviewed. This compounds the problem. It is imperative that the EMR notes that the provider has reviewed these files.
- Going forward, it is imperative that the system allow for the selection of the Sure Scripts files for reconciliations as per number “3” above.
Everyone agreed that a collaboration with NextGen, Sure Scripts and SETMA would result in functions beneficial to all healthcare providers.
In response to a discussion about SIG Codes and Sure Scripts capturing non formulary and non insured medications, we referenced Christopher Diblasi’s comments from page five in the above attachment:
Christopher from Sure Scripts -- Hi all – if the group is interested in learning a bit more about this, might be worth a quick call to discuss? The characteristics of Surescripts’ Medication History dataset are complex. In the meantime, a couple additional thoughts:
- Surescripts’ Medication History data consists of two datasets: 1) claims from PBMs and 2) dispensed records from pharmacies. SIG codes are contained in pharmacy dispensed records but are not contained in PBM claims. So within the overall medication list, some meds may contain SIG information and some may not. That being said, to Jonathan’s point, the fact that only 3 of 52 meds contained SIG codes is concerning.
- There are other discrepancies across other data fields similar to what I described above. As I mentioned, it is fairly complex. The attached slides break it down somewhat, but it’s often best to discuss rather than read emails/powerpoints.
We will schedule a call in the next two weeks.
|