|
Abstract:
This presentation describes a method for maintaining excellent medical records with Chronic Problem List reconciliation. The process of Chronic Problem List Reconciliation involves the following six steps:
- The ability to select precise and accurate diagnoses from a robust electronic list.
- The ability to re-order the Chronic Problem List with the most important diagnoses at the top.
- The ability to highlight diagnoses in the Chronic Problem List which have not been assessed in a pre-determined period of time.
- The ability to archive resolved or invalid diagnoses in a retrievable fashion electronically with the date on which the diagnosis was archived.
- The ability to copy Chronic Problem List diagnoses into the Acute Assessment.
- Following clear principles of Chronic Problem List creation and reconciliation.
Following these steps will enable complex care to be completed in an electronic medical record system maintaining an effective record for continuity and excellence of care.
Introduction
Medical Records are not an end in themselves, neither are they an exercise for the aggravation of healthcare providers. Medical Records are a method of communication between healthcare providers and patients for continuity, quality and consistency of care. In the outset, medical records were at best a silhouette of the patient’s care. They showed the broad outlines of the patient but with very little granularity. In the 19th Century, health records, when they existed, were brief acknowledgements of treatment or prescriptions, often kept on 3” by 5” index cards. In the 20th Century medical records increased in granularity reaching their pinnacle with dictation and transcription of healthcare delivery records which had a great deal of content. Yet, those records had the same flaws as 19th Century records. They were geographically bound, i.e., they could only be in one place at a time and one part of the record could not interact with another. Each episode of care was a separate record and the only continuity was when previous health information was included in the record of the current episode.
As the 21st Century approached with the explosion of medical information, all previous health record methods proved inadequate. After 1970, and more so in the first decade of the 21st Century health records became increasingly electronic. Electronic Medical Record (EMR) had the benefit of being accessible at many locations simultaneously. They were cumulative and documented patient care longitudinally. Increasingly, portraits of patient’s health care began to emerge, replacing the outlines of care or silhouettes.
EMR offered solutions to some of the most difficult problems associated with medical records. However, EMR created as many problems as they solved. On page 24 below, there are links to thirty-five articles about EMR which SETMA has produced over the past fourteen years. Issues of security, confidentiality, content, interoperability, access, analytics and many more are addressed in these articles.
Perhaps the two most difficult issues in medical record keeping are the maintaining of:
- Valid and complete medication records and
- Valid and complete chronic problem lists.
Unfortunately, these two functions just happen to be the two most important parts of the record. Both issues are foundational to the fulfillment of the Triple Aim and to the achievement of patient safety. Because the chronic problem list is also critical for reimbursement, the sustainability of excellence in care, which is fundamentally an economic issue, the list is critical to quality outcomes. This is particularly related to HCC and RxHCC values (see HCC RxHCC Risk Tutorial for a full explanation of this system) which are important not only in Medicare Advantage, but also in Accountable Care Organizations work with Fee-for-Service Medicare and in Patient-Centered Medical Home.
The critical issues with problem lists are:
- The list must be produced from a robust ICD-9 and soon ICD-10 deployment from which diagnoses can be entered into the problem list, the assessment, disease management tools, referral templates and other parts of the EMR.
- The typing in of diagnoses, which will not work with billing and coding, or with sharing of data and analytics, is lethal to maintaining an accurate problem list.
- Upgrades to ICD-9 and certainly to ICD-10 include social codes such as “lives alone”, “Military Recently Deployed,” etc. There are also codes for such things as “Elevated CRP, etc, which allows you to maintain surveillance on conditions which are not presently under treatment but which need not to be forgotten and which need follow-up. While these upgrades allow for more granular documentation of the patient’s condition, they may produce a problem of growing Chronic Problem List which becomes unwieldy.
- Problem List Reconciliation require real time, routine review of the problem list with the ability to archive in a retrievable fashion diagnoses which are not currently active but which may become active in the future.
- Without these capacities the maintenance of the Chronic Problem List will be increasingly problematical.
Problem List reconciliation is a team effort including the following:
- Chart Maintenance - this is part of ever visit and every review of the patient’s chart.
- When the patient is seen the provider needs to review the problem list, as she/he must review the medication list. It is as if you have a “reconciled” medication list and a “reconciled” problem list at each visit.
- When data, information, tests, procedures, etc., are received on a patient from another provider or organization the clerk has to be given the authority to add diagnoses to the chronic problem list. Then when the patient is seen the provider reviews the diagnoses and determines whether it should remain in the list or not.
- It is ideal if it is possible to reorganize the chronic problem list in order of priority. SETMA has designed a system where it is easy to do this in a matter of seconds even with 18 diagnoses. Thus, the most important diagnoses can appear at the top of the list such as Diabetes, Renal Disease, Prostate Cancer and less critical but important diagnoses can appear last such as “Elevated Sed Rate”, “Hx of Tobaccoism”, “Family History of Diabetes”, etc./ .
- Chart Reviews - nurses charged with going through charts:
- Making certain that for important diagnoses that there is history, physical, testing, etc., information to support the diagnoses and calling it to the provider’s attention if it is not there .
- Reviewing consultations, procedures, etc., to make sure that all valid and accurate diagnoses have been entered into the chronic problem list so that they can be brought to the attention of the provider.
- Making sure that all diagnoses are entered electronically and not by typing so that they interact with the disease functions of the system.
- Quality Improvement - healthcare providers reviewing the charts of other providers
- The same kind of review is done by the provider during a patient encounter and the nurse with chart reviews, but it is more focused on the quality of care based on the documentation in the record and the completeness of the chronic problem list. This is most often done with new providers, or with providers having problems with their documentation.
- After these reviews a face-to-face or a written conversation is had with the provider to address deficiencies.
General Principle: Reconciliation of medications or of chronic problem lists is hard work and must be a priority, if it is going to be done well and consistently.
Tutorial for SETMA’s Chronic Problem List Reconciliation
(Disclaimer: For fourteen years, SETMA used a “home grown” ICD-9 Code list. With the advent of ICD-10 and SNOMED, it was necessary to update our system to a proprietary list. SETMA has no financial interest in the company whose product we selected and we are not paid by this company. We have nothing to disclose. There are other vendors which can be used.)
The tool which SETMA employs is integrated with our EMR. This tool has taken the 15,000 ICD-9 codes and expanded them to a list of 100,000 codes by naming each code in multiple fashions to make it easy to access the correct code. This transition will enable SETMA, we think, to utilize the 150,000 ICD-10 codes more efficiently and more effectively.
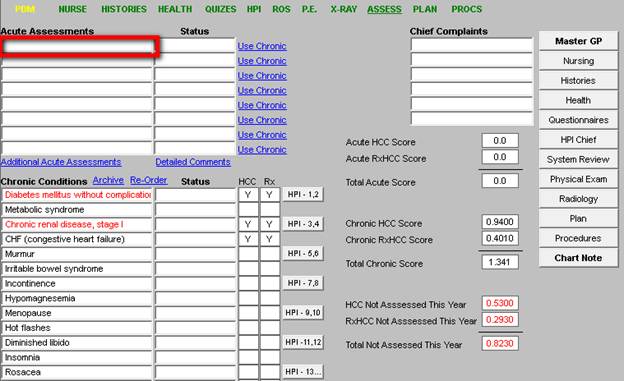
The following is how we use the tool, by clicking in the Assessment space, the tool is launched. In the space below, outlined in red, you would type a name or abbreviation, such as “CHF.”
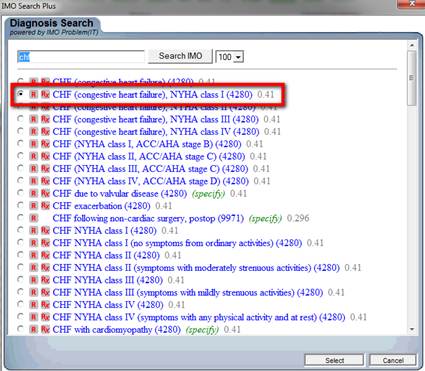
Once the correct code is identified, the radial button next to it is marked and the button entitled “select” is clicked (see below).
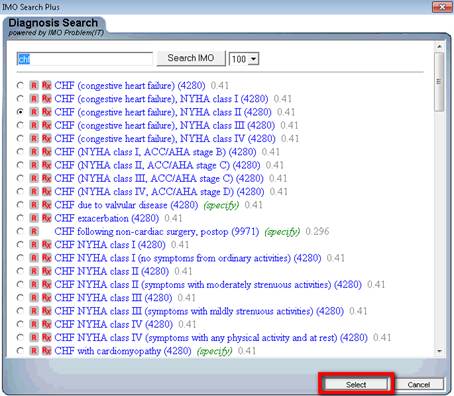
The tool we selected also notes whether the diagnoses is a HCC and/or an RxHCC and the coefficient assigned to that diagnosis is listed. Each is outlined in red below.
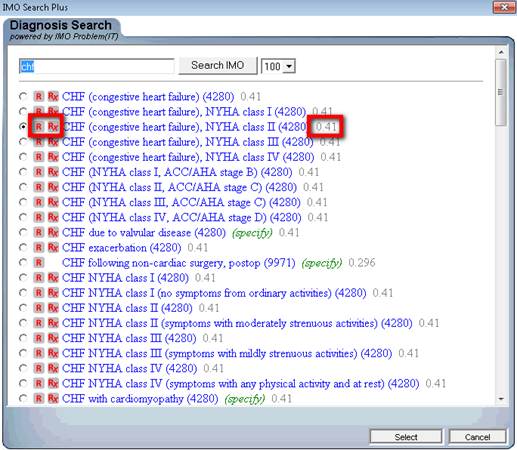
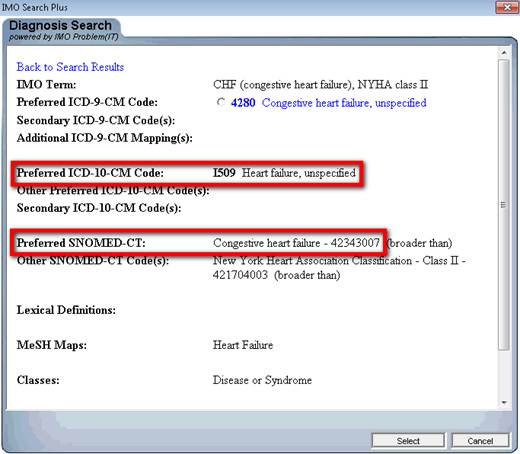
Our tool for ICD-9 Code selection already has ICD-10 and SNOMED cross linked as is seen below. In 2014, when ICD-10 is launched, our use of it will be simply a change at the server level of our EMR. The same will be true for SNOMED.
In this same way diagnoses can be added at many different places in addition to the Acute Assessment, including:
- Chronic Conditions
- Plan
- Referrals
- Disease Management tools
Valid and complete Chronic Problem Lists are critical to excellence of care because if a diagnosis is out of mind, it will not be evaluated. One of the audits SETMA does is to look at all diagnoses which are identified in the hospital medical record. To do this, all of the following are reviewed:
- Daily progress notes
- Procedures
- Laboratory values
- History and Physical examinations
- Consultant notes
- Surgical notes
- Etc.
The Discharge Summary (renamed by SETMA as “The Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan”) is reviewed to see how many of those diagnoses are not in this transition of care document. Any diagnoses not in the hospital summary will routinely be overlooked in follow-up.
The great value of documenting hospital history and physical examinations and Hospital Care Summaries and Post Hospital Plan of Care and Treatment Plan in the same EMR data base is that the documentation element of care continuity is seamless. When the hospital record is completed with all admitting morbidities and co-morbidities, the follow-up of the patient is made straightforward and complete.
Because the medical record and the chronic problem list is a longitudinal record, i.e., it is created with the most remote diagnoses first and the most recent last, it is possible to have important and critical diagnoses mixed in with more routine issues. To maintain accurate, complete and valid chronic problem lists, it is important occasionally to “re-order” the diagnoses so that the most important issues appear first. This function is potentially an appropriate means for monitoring and auditing Chronic Problem Reconciliation. Its value in Chronic Problem List Reconciliation is supported by:
- It requires the healthcare provider to review all diagnoses in the Chronic Problem List.
- It can be done in a few seconds.
- Acknowledgement of the Chronic Problem List being re-ordered can be automatically documented when this re-ordering process is done.
- In that the re-ordering would only take place every several years, it will make it non-intrusive to the provider’s workflow.
- A check box can be deployed on the Chronic Problem List which allows the provider to indicate that the list has been reviewed at times other than when the re-ordering process is completed.
The following is SETMA’s tool for that process.
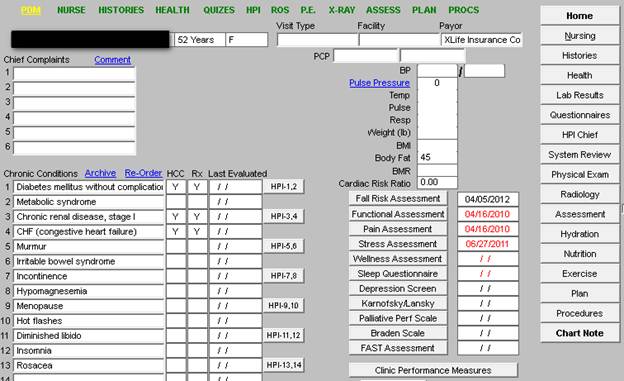
This template is SETMA’s Master GP Template. Outlined in red below is the Chronic Problem list. The first line includes the following: “archive, Re-Order, HCC, RxHCC and Last evaluated.”
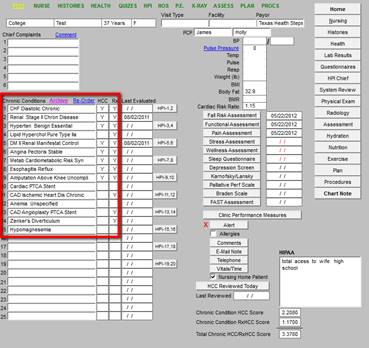
To initiate the process to re-order the Chronic Problem List, the button entitled “Re-order,” which is outlined in red below, should be clicked.
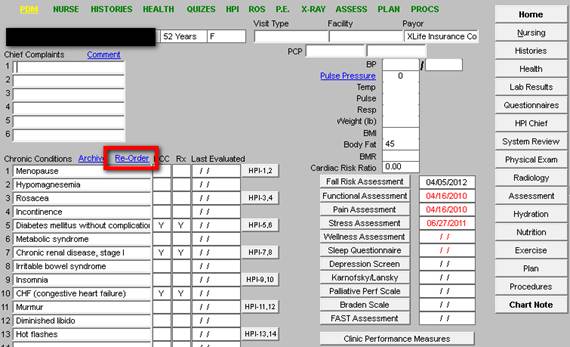
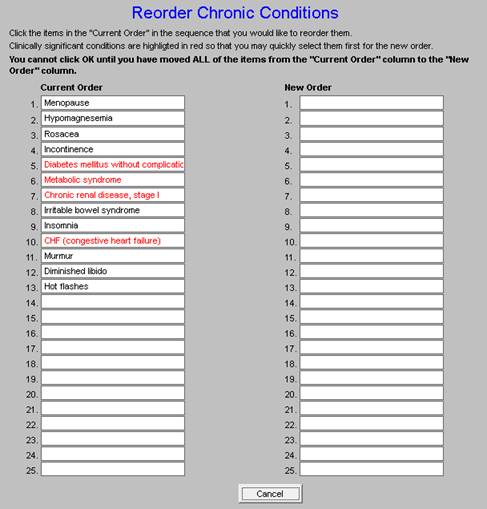
When the button. entitled, “Re-Order,” is clicked, the following template is deployed.
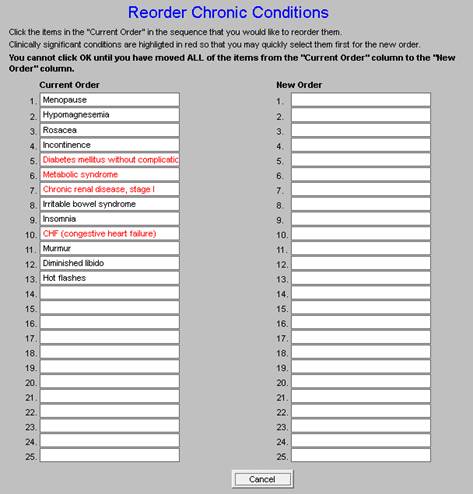
In the left hand column, the Chronic Problem List, as it currently exists, is displayed. In the right hand column, the re-ordering list will be developed. The provider must click on each diagnosis in the “Current Order,” in the order she/he desires for the diagnoses to be displayed. As each diagnoses is clicked, it will appear in the “New Order” list.
On the screen shot below, the Re-order Chronic Conditions List is from a real patient. As can be seen, the principal diagnoses are not at the top of the list. Chronic Problem List Reconciliation requires that providers have an effective and efficient means for moving diagnoses around in the list.
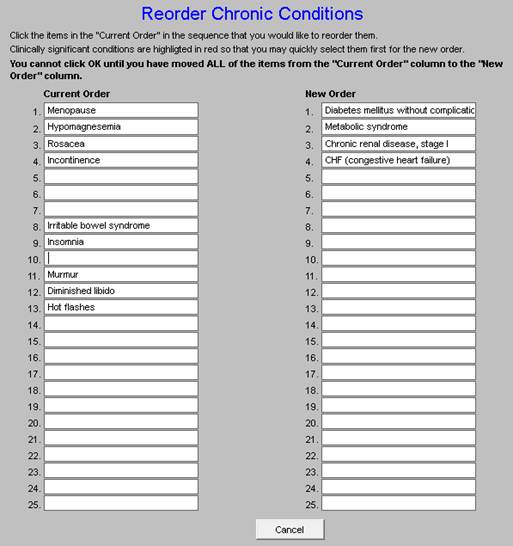
To re-order the list, the provider clicks on each diagnosis in the order the provider wishes for the diagnoses to be displayed in the Chronic Problem List. This process is illustrated in the screen shot below. As each diagnosis is clicked, it is removed from the “Current Order” and moved to the “New Order.”
When all diagnoses have been clicked, a button entitled “OK” will appear. That button is outlined in red on the screen shot below.
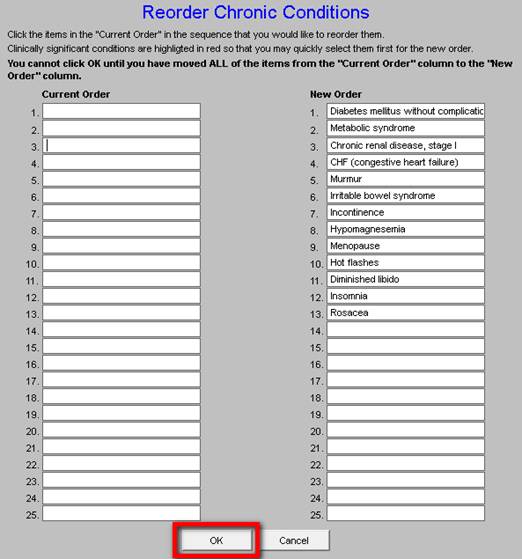
When that button is clicked the new order of Chronic Conditions will be displayed on the Master GP Template.
This process takes less than one minute and is an important issue in “chart maintenance” and should be done by the healthcare provider, or by a highly trained assistant.
- This function allows the archiving in a retrievable fashion of any diagnoses which will then disappear from the Chronic Problem list but which can be restored to the acute assessment and/or to the Chronic Problem list with the click of a button
- The archived Chronic Problem List needs to be accessible by the click of a button.
- The date on which the problem was archived needs to be stored also.
- With the expansion from 15,000 ICD-9 codes to !50,000 ICD-10 codes, it is possible that the number of codes which appear in the Chronic Problem List could increase significantly.
- The ability to archived diagnoses in a retrievable function will be helpful in maintaining Reconciled Chronic Problem Lists.
Clicking the “Archive” button launches the archive function. The Master GP Template is shown with the “Archive” button outlined in red.
GP Master Template
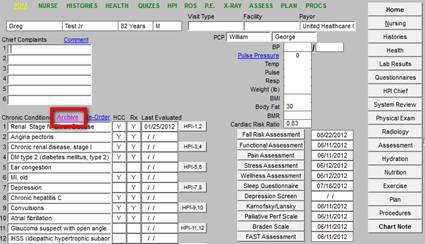
The “archive” button also appears on the Assessment Template as is shown below. Having multiple avenues for performing the same function increases the probability of it being done.
Acute Assessment Template
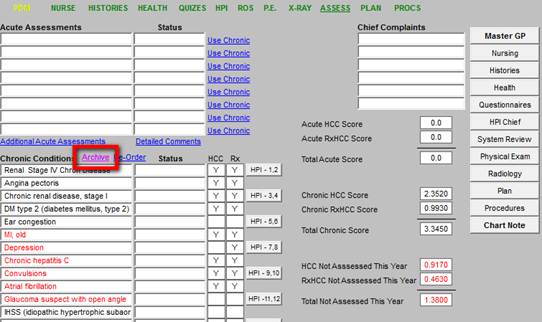
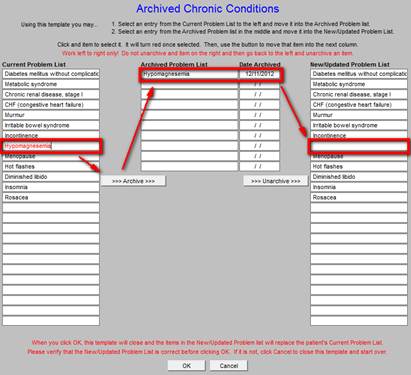
When either of the “archive” buttons is clicked - on the Master GP or the Assessment templates - the following template is deployed. It is entitled, “Archived Chronic Conditions.”
As can be seen below, the Archived Chronic Conditions template displays:
- The Current Problem List
- The Archived Chronic Problem list
- The Date Archived
- The New/updated Problem List
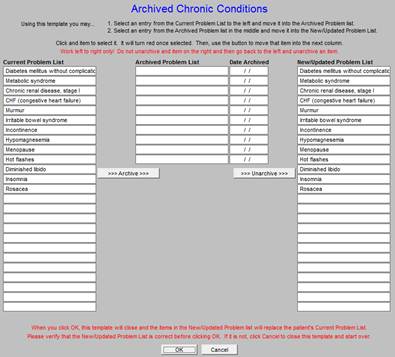
This allows the provider or nurse to review the diagnoses which have previously appeared in the Acute Assessment or the Chronic Problem List but which have now been archived and to know the date on which it was archived. If a diagnosis in the Chronic Problem List no longer applies, it may be archived. The invalid or resolved problem is highlighted by clicking on it whereupon it is automatically moved to the archived list.
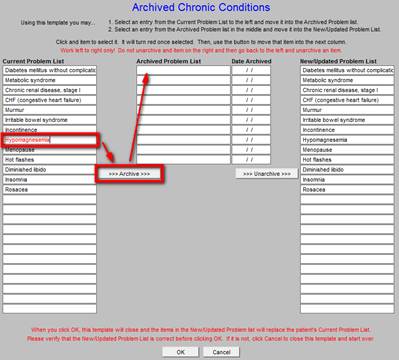
The archived diagnosis is this moved from the Chronic Problem List to the Archived List.
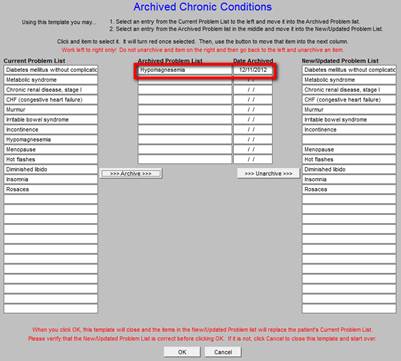
If a previously archived diagnosis becomes valid again, it may be moved back to the Chronic Problem List by clicking on it in the list of archived diagnoses.
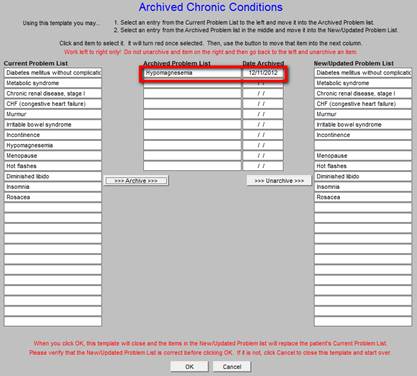
The diagnosis will be restored to the Chronic Problem List.
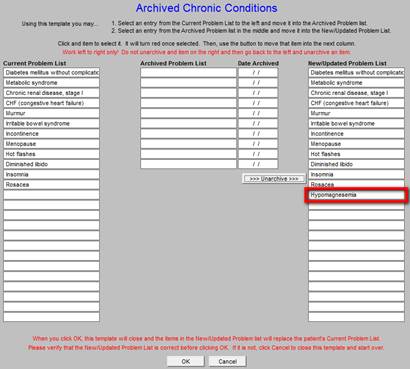
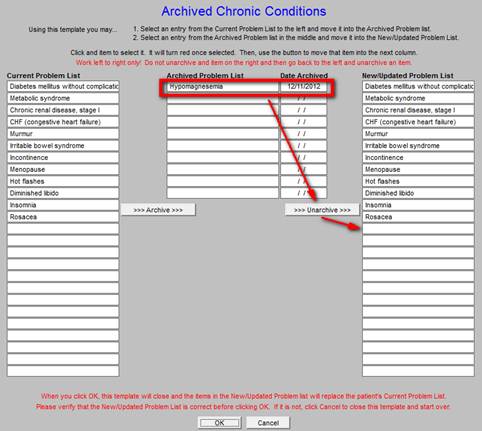
The complete process is shown on the following Archived Chronic Conditions template. A diagnosis is moved from the Chronic Problem List to the Archived List and then is moved back to the Chronic Problem List from the Archived List.
- For instance, those diagnoses which are HCC and/or RxHCC diagnosis must be reviewed annually, if payment is to be received.
- The Chronic Problem List highlights those diagnoses in red until they have been evaluated to alert the provider that the diagnosis needs to be reviewed.
- Of course, any other reason for alerting the provider to review a Chronic Problem can be coded into the system. In fact, a color coded system can be built to where one need is highlighted in red while another purpose can be highlighted in another color.
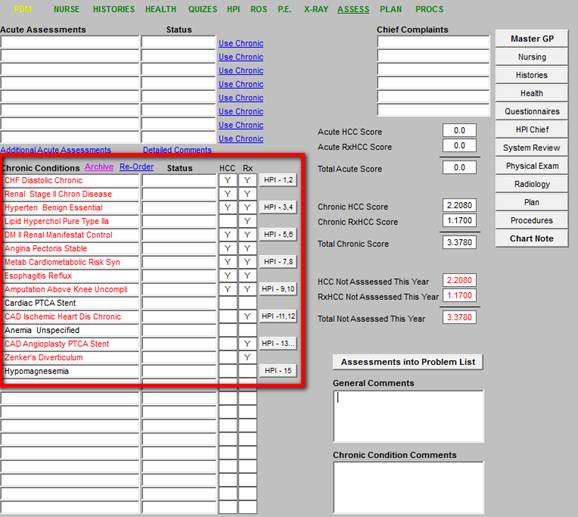
As you can see below, once the diagnoses in red are assessed, the red alert color designation is removed.
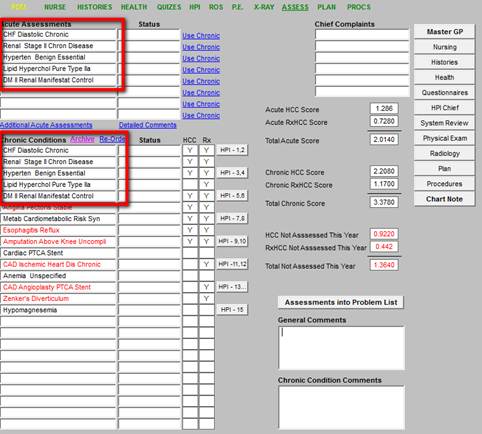
- Once an accurate diagnosis has been established in the Chronic Problem List. a robust ICD-9 code list and certainly an ICD-10 code list with 150,000 options, can require unnecessary review to make sure that the diagnosis in the Acute Assessment correlates with the diagnosis in the Chronic Problem List. Therefore. must be a means for moving diagnoses from the Chronic Problem List to the Acute Assessment for the current encounter.
- SETMA accomplished this by placing buttons next to each space of the acute assessment. When the button is deployed, the Chronic Problem List appears in a new window. When the Chronic Problem being evaluated is highlighted by the provider, a copy of it is moved to the Acute Problem. This allows for consistency in what is being evaluated thus preventing the duplication of diagnoses, or the changing of a precise diagnoses to a more generic one.
- As we migrate to ICD-10 in 2014, accessing Acute Assessment diagnoses will be more complicated when you are drawing from a 150,000 element list. Being able to move an establish Chronic Problem from the Chronic Problem List to the Acute Assessment will make sure that you don’t have multiple codes with slightly different meaning for the same condition.
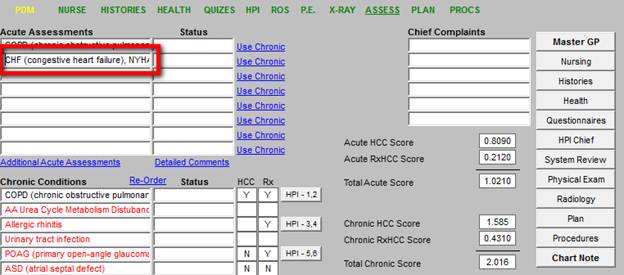
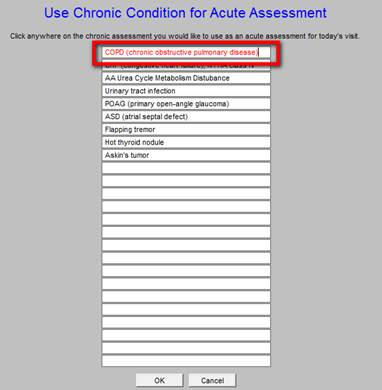
When a provider wishes to move a Chronic Condition to the Acute Assessment, the “Use Chronic” button is clicked. Then the diagnoses is found on the Chronic Condition List. By clicking that diagnoses a copy, with all electronic functions attached, is moved from the Chronic Problem List to the acute assessment while leaving the Chronic Problem List unchanged.
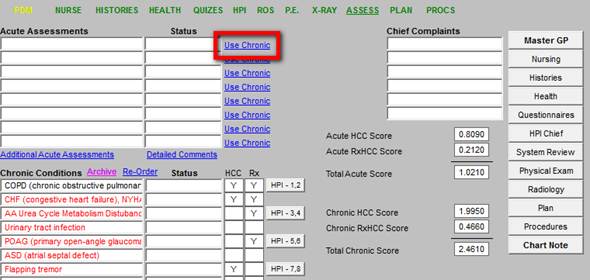
When “Use Chronic” is clicked the following pop-up appears. When a diagnosis is clicked it is copied to the Acute Assessment. This keeps the provider from having to search the ICD-9 or ICD-10 data base to find the same diagnoses.
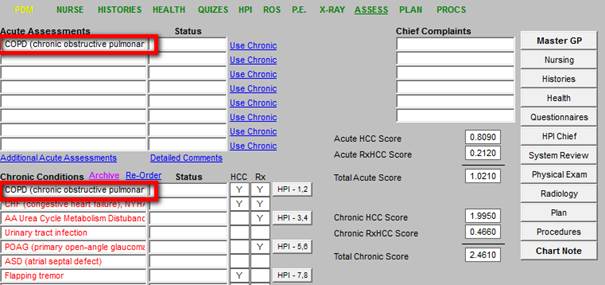
The Chronic Condition then appears in the Acute Assessment for that visit.
- Diagnoses cannot be typed into the Chronic Problem List, they must be chosen from an electronically created list which then interacts with other parts of the EHR particularly the billing and coding functions.
- The list must be reviewed periodically for accuracy. Generally, that periodicity will be at each encounter.
- Duplications and particularly contradictions in the problem list must be corrected, i.e.., if the patent has an above knee amputation on the right and the record says that it is on the left, that must be corrected. This is what we call “chart maintenance.” It is no shame for an imprecise or incorrect diagnosis to be in the record; the shame is if the record is not regularly reviewed in order for such errors to be caught and/or for the record not to be corrected when the error is discovered.
- The reality is that because it is a function of human effort, medical records are only asymptotically approaching perfection. That is the goal and it should be continually pursued as the ideal. Imperfection must never be accepted or tolerated, even though we know that perfection is rarely achieved.
- The creation, maintenance and reconciliation of a complete, valid and current Chronic Problem List is a team effort.
The following are links to SETMA’s Your Life Your Health articles related to Electronic Medical Records.
|