|
Index
SETMA has long had the philosophy that if healthcare providers are going to be held accountable for certain actions, they ought to:
- Know what they are going to be held accountable for.
- Measure their performance before an external organization reports this performance at some distant time in the future.
- Have a plan and a method for improving their performance.
Below this tutorial is a lengthy discussion of SETMA’s 8-day pilgrimage to excellence in HCAHPS performance as a function of patient-centeredness in inpatient care. This is the beginning of our becoming patient-centered in our inpatient care.
The following are the vendor questions, which reflect the responsibility of the healthcare provider, in the HCAHPS Survey.
- During this hospital stay, how often did doctors treat you with courtesy and respect?
- During this hospital stay, how often did doctors listen carefully to you?
- During this hospital stay, how often did doctors explain things in a way you could understand?
The scale for rating these questions is “always,” “usually,” “sometimes” and “never.”
Discharge Instructions is considered an HCAHPS “summary measure” because it consists of two questions from the survey reported as one measure. By combining related questions into summary measures, similar questions are tied together. The Centers for Medicare & Medicaid Services reports that the statistical reliability of HCAHPS measures increases with the use of summaries. HCAHPS measurements of effective discharge planning are consumers’ assessment of these specific components of hospital care:
- During this hospital stay, did doctors, nurses, or other hospital staff talk with you about whether you would have the help you needed when you left the hospital?
- During this hospital stay, did you get information in writing about what symptoms or health problems to look out for after you left the hospital?
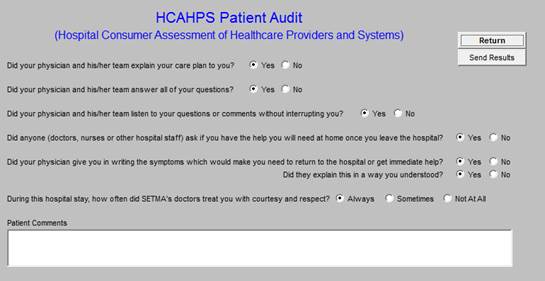
On July 19th SETMA’s Department of Care Coordination took the work from earlier in the week and defined the questions which would be asked in SETMA’s Internal HCAHPS Survey; they are:
“As part of SETMA’s continuing effort to assure that all patients receive exceptional care by our providers, these questions will be asked of the patient at the time of the Hospital Follow-up Call by the staff of the Care Coordination Department. This allows our patients to express their own feelings about the care received during their most recent hospitalization. This is an internal audit that will allow all SETMA providers to evaluate themselves from their patient’s point of view.
- “Did your physician and his/her team explain your care plan to you? Yes No
- “Did your physician and his/her team answer all of your questions? Yes No
- “Did your physician and his/her team listen to your questions or comments without interrupting you? Yes No
- “Did anyone (doctors, nurses or other hospital staff) ask if you have the help you will need at home once you leave the hospital? Yes No
- “Did your physician give you in writing the symptoms which would make you need to return to the hospital or get immediate help? Yes No Did they explain this in a way you understood? Yes No
- “During this hospital stay, how often did SETMA’s doctors treat you with courtesy and respect? Always Sometimes Not at all
Patient Comments:”
These steps, along with that which follows the Tutorial, provide the basis for SETMA’s solution to HCAHPS.
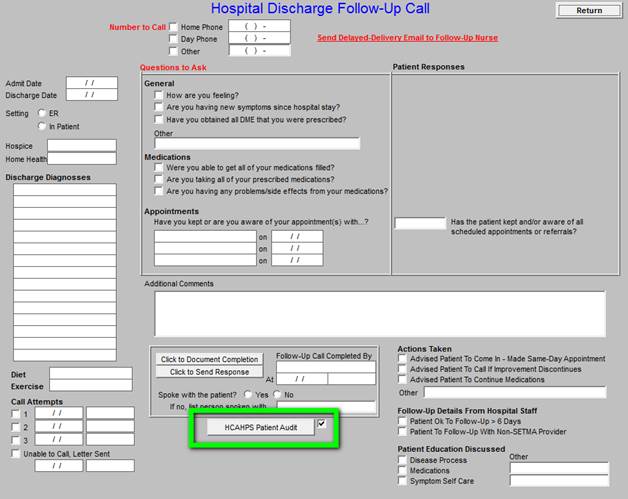
This is the Hospital Discharge Follow-up Call template which his sent by SETMA’s Hospital Care Team to SETMA’s Department of Care Coordination. All patients discharged from the hospital receive a “care coaching” call the day after leaving the hospital. The Department is currently making over 30,000 patient calls a year. This internal survey will only add a couple of minutes to each call. (The Hospital Discharge Follow-up Call Tutorial can be reviewed at http://jameslhollymd.com/epm-tools/Tutorial-Hospital-Follow-up-Call.)
Outlined in “green” on this template is the button which deploys the HCAHPS Patient Audit.
When deployed this button launches the HCAHPS Patient Audit template. It is on this template that the SETMA Internal HCAHPS Survey questions are listed. This template will allow the patient’s responses to be captured in data fields which will allow:
- Auditing by provider name.
- Public Reporting by provider name the aggregate performance result.
- Sending to each provider substandard results so that the provider can review for themselves their care for particular patients. We believe that daily reporting of results to the provider only by patient name is the only way to effect change in HCAHPS performance.
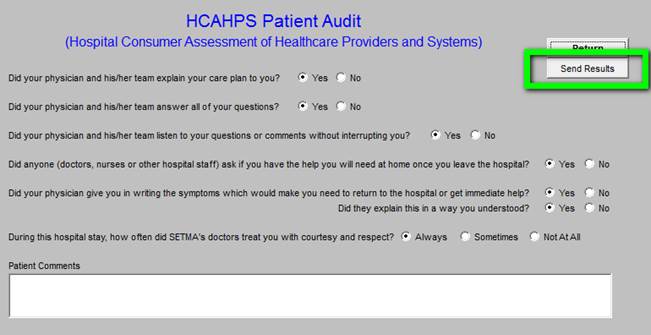
The button outlined in “green” entitled “Send Results” allows the results of the HCAHPS survey on a single patient to be sent to the attending physician so that immediate feedback can effect changes in the provider’s approach to patients. This result will not be discussed with the patient but is only for the benefit of the provider, who having this result the day after the patient leaves the hospital will benefit from the feedback. Being the feedback from a single patient, the provider will have more possibility of recognizing where improvement can be made.
What I thought was impossible turned out to seem so, simply for the lack of totally understanding the concept of patient-centeredness. Having been an NCQA Tier Three Patient-Centered Medical Home (PC-MH) for three years and having had AAAHC accreditation for Ambulatory Care and for Medical Home for the same period, SETMA had worked on transforming our ambulatory practice. As we renewed our NCQA PC-MH Recognition for 2013-2016, we realized that we had made major strides toward this transformation.
However, one aspect of practice transformation which mystified us was our perception of the subtle change of the vocabulary of the Institute for Healthcare Improvement’s Triple Aim; as it turns out, the change was more in our understanding of the Triple Aim. When first enunciated in 2008 in Health Affairs, Don Berwick and his colleagues called for “improved care, improved health and decreased cost” (again this was my concept of the Triple Aim) as the principle goals of healthcare transformation. Today (July 22, 2013), as I have reviewed the original statement of the Triple Aim in The Health Affairs 2008 article, the first goal was actually defined as “improved experience of care,” which is not significantly different from the 2013 vocabulary of the Triple Aim which is:
- “Improving the patient experience of care (including quality and satisfaction);
- “Improving the health of populations; and
- “Reducing the per capita cost of health care.”
As SETMA has taken on the responsibility of fulfilling the Triple Aim, we focused on the improvement of Quality of care which we associated with the improvement of the processes of care. As we transformed our ambulatory practice into a PC-MH, we began to understand that patient convenience and patient satisfaction were important aspects of healthcare transformation. In August of 2010, SETMA struggled with whether “patient convenience” was a worthy goal. As we formed our Department of Care Coordination, we began to realize that “coordination” meant scheduling which translates into:
- “Convenience for the patient which
- “Results in increased patient satisfaction which contributes to
- “The patient having confidence that the healthcare provider cares personally which
- “Increases the trust the patient has in the provider, all of which,
- “Increases compliance (adherence) in obtaining healthcare services recommended which,
- “Promotes cost savings in travel, time and expense of care which
- “Results in increased patient safety and quality of care.
“As with the structure of quality metrics in tracking, auditing, analyzing and public reporting process and outcomes measures, coordination requires intentional efforts to identify opportunities to:
- “Schedule visits with multiple providers on the same day, based on auditing the schedule for the next 30-60 days to see when a patient is scheduled with multiple providers and then to determent if it is medically feasible to coordinate those visits on the same day.
- “Schedule multiple procedures, based on auditing of referrals and/or based on auditing the schedule for the next 30-60 days to see when a patient is scheduled for multiple providers or tests, and then to determine if it is medically feasible to coordinate those visits on the same day.
- “Scheduling procedures or other tests spontaneously on that same day when a patient is seen and a need is discovered.
- Recognizing when patients will benefit from case management, or disease management, or other ancillary services and working to resources those needs.”
This was our initial effort at seriously dealing with the first element of the Triple Aim. We would, of course, come to understand that “Improving the patient experience of care (including quality and satisfaction)” involved a great deal more than scheduling, but our focus at that time was ambulatory exclusively.
For several years, SETMA’s physicians who care for inpatients at Baptist Hospital of Southeast Texas have monthly met with hospital administration to review provider performance in regard to total cost, lengths of stays, utilization of laboratory, imaging services, and consultations in contrast with case mix index, mortality, severity index, HCAHPS scores, etc. In our July 15, 2013 meeting, we had a vigorous and somewhat heated discussion of HCAHPS. SETMA-provider HCAHPS scores were not terrible but except for one provider, they were not exemplary. SETMA’s providers expressed their frustration with the subjectivity of the HCAHPS evaluation and asked for the details of what is included in the survey.
On Tuesday, July 16, 2013, at 6:34 AM, SETMA published an analysis of how we would approach the HCAHPS survey. We determined to do it in a systemic, sustainable fashion. It is noteworthy that the SETMA/Baptist meeting concluded at 1:45 PM on the 15th. The following was distributed less than sixteen hours after the conclusion of the meeting in which HCAPS was discussed at length. (The entire discussion, which went on the entire week, can be reviewed on SETMA’s website at http://jameslhollymd.com/letters/ under Hospital Consumer Assessment of Healthcare Providers and Systems -- HCAHPS
At the July 15th meeting, “the major discussion was around the HCAHPS patient satisfaction survey done by a contractor for Baptist. There was on the part of providers a sense of futility as the standard required is extraordinarily high and the judgment of whether, or not a provider meets that standard is totally subjective on the part of the patient and/or patient’s family. Because we deal with an extremely vulnerable population, including a large population of those who have not been part of the healthcare system previously, we find these standards difficult.
“SETMA’s goal is to solve this problem in a systemic and sustainable fashion rather than simply trying to use gimmicks which are a hit and miss effort. And, it is our goal to solve this problem in a manner which will contribute to the quality of care all of our patients receive. SETMA requested a copy of the content of the standard and that has been given to us. We will review that this morning (July 16th) in our monthly provider training meeting. A copy of the attached (The Vendor HCAHPS Survey tool) will be given to each SETMA’s providers and I will hold a meeting with our hospital care team and review it with them.
- “Hospital Admission Plan of Care - For almost a year now, SETMA has been producing a document upon the patient’s admission to the hospital which includes: diagnoses, reconciled medication list, procedures, tests, consultations planned for the hospitalization, potential for readmissions and detailed contact information. We are going to make one change. Rather than the hospital staff giving this to the patient, it will be placed at the front of the chart and the attending physician will give this to the patient and explained it to them. For those unfamiliar with this document a de-identified copy of a recent admission is attached above.
“The Hospital Care Team will review this document to see how we can strengthen it. We will ask the attending physician to note on the Daily Progress Note after admission that this document has been given to the patient and explained to the patient and/or family.
- “Notification to the patient of the attending - Our Hospital Care team will be given a script for how to address the identity of the patient’s attending physician. It will say something like, “I am a member of SETMA’s hospital care team and I work closely with Dr. ______, who will be your attending physician for this admission. We know that Dr. __________ is your personal physician but he has asked Dr. __________ to see you during this hospitalization. All of your information will be communicated to Dr. __________ and I and your attending physician have access to all of your medical history and past medical treatment. Don’t hesitate to ask us about your care. We will be happy to explain anything that is not clear. We want your hospital care experience to be a good one.”
- “For Those Who Round Early - There is a tremendous advantage to the patient for early rounding, but on occasion (over 80% of the patients are awake and eager to talk to the doctor no matter how early he/she makes rounds. There is more frustration for the patient and family when the provider rounds very later in the day - after 3 PM - than when a provider rounds early), the patient is not alert. As a consequence, we will ask all provider who round before 6 AM to make the following statement to the patient AND to document this on the patient’s chart.
‘SETMA has a healthcare team who works in the hospital all day to make sure that you get the care you need. That team communicates throughout the day with me (the attending), but because I round early, I know sometime all of your questions do not get answered. Therefore, the Hospital Plan of Care which I have given you has my office and cell phone number on it. If you have a question, call me. If your family or medical power of attorney would like to meet with me, call my office and they will schedule a conference at the office in the afternoon. It is important to me that you and I work together to provide you the best possible care. We start early because we do not want to waste your time and we want all of your care to begin as soon as possible.’
- “Further Step for Those Who Round Early - When a patient’s care is complex and when the patient is unable to comprehend their care and when others are not present, the attending will ask a member of the Hospital Care Team to return during the daylight hours to explain the plan of care to the patient’s family and to arrange for a conference with the attending if it is desired.
- “Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan -- Upon discharge, the patient is presented with a copy of their Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan and their personalized Hospital Follow-up instructions. (A copy of that document is attached for the same patient whose Hospital Admission Plan of Care is presented above. In the past 4.3 years SETMA has discharged more than 21,000 patients from the hospital. 98.7% of the time, the Hospital Care Summary and the Follow-up instructions have been given to the patient at the time of discharge.
“SETMA’s providers and hospital care team will review this document to make sure that it is complete and a renewed effort will be made to make sure the patient and/or family receives the Follow-up Plan with the following statement, “Dr. ______ has asked me to make sure that you receive this document so that you know exactly what your care is to be. Is there anything you don’t understand and are you able to carry out these plans? Dr. ____ has asked me to arrange for you to receive a follow-up telephone fall tomorrow to make sure that you have your medications and understand you care.”
- “Care Coordination Follow-up Call- Every patient discharged from the hospital receives a 12-30 minute telephone call from SETMA’s Care Coordination Department the day after discharge. They will be instructed to say, “Your attending physician, Dr. ________, has asked me to call you to see if you have any questions about your hospitalization, your medications or your follow-up care.” The Coordination Department will repeat the medication reconciliation and will review all follow-up plans.
- “Follow-up with Primary Care Provider - If a patient is high risk for readmission, he/she will be seen by SETMA within two days of discharge and if they are not they will be seen by their primary care provider within five days of discharge.”
From the meeting on July 15th, through the analysis and realizations of the 16th, 17th, and finally the 18th, it became obvious to SETMA that while our providers had been practicing excellent medicine, we had not been practicing patient-centered care in the hospital. We had transformed our ambulatory clinics into patient-centered care, but we had retained the old structures and patterns of provider-centric care in the hospital.
The language in the Seven Steps above began the process of transforming our inpatient care to a patient-centric model but the capstone was a 2011 White Paper. published by the Baptist Leadership Group, entitled, “The HCAHPS Imperative for Creating a Patient-Centered Experience.” That paper can be found at http://www.healthstream.com/Libraries/whitePapers/HCAHPS_Imperative.sflb.ashx. While this paper principally deals with issues which are the responsibility of hospital administrations, the patient-centeredness is a clarion call to SETMA.
“On rounds this morning (Wednesday, July 17th), I sat in a chair by the bedside which was awkward and difficult particularly since the chairs are across the room and are heavy. It seems odd but I’ll give it a try. In addition to the history and physical with each patient, I did add some new dialogue including:
- “After explaining the diagnoses and the plan for the patient’s care, I asked, “Do you have any questions about your care?”
- “’Do you understand what is going to take place?’
- “’Do you have adequate help and support when you go home?’ This is not a new question.
- “’Concluding the visit with, “Is there anything else you need or that I can do for you?’
- “I then documented this conversation in the progress note in the chart.
“After rounding, I felt a little like the Boy Scout who returned to the Scout Hut eight hours after leaving. The South Master said, “Where have you been?” The Scout said, ‘I was doing my good deed for the day.’ The Scout Master said, ‘What did you do?’ To which the Scout responded, ‘I helped a little, old lady across the street.”’ The Scout Master said, ‘Why did it take so long?’ The Scout said, ‘She didn’t want to go!’ Rounding took longer sitting in a chair by the bed because in two instances the ‘little, old lady’ in that chair didn’t want to get out of it and it took a while to wrestle the lady out of the chair. (Smile)
“We will see how this goes but at present our plan is:
- “For the provider to give the patient their Plan of Care in writing on the day of admission and explain it to them.
- “Sit while talking to the patient - this actually is valuable as it places you on the level of the patient.
- “Offer a conference at the office with any family not present, who is on the patient’s HIPPA form, and who wants to know what the plan and expectations are for the patient. In one case this morning the patient wants one thing (she is competent) and the family wants another. We have arranged a conference for the afternoon in my office.
- “Give the patient a business card with identification and contact information for the SETMA team member seeing them and add, “Dr. _____ (naming the attending) has asked me to see you....” Every SETMA team member will relate their contact with the patient back to the attending. In some ways this violates my concept of a “team” but in that it is the attending who is being judged by the HCAHPS, we will focus attention on that person.
- “SETMA’s Care Coordination Department will add the following questions to their follow-up call:
- “Did your physician and his/her team explain to you your care plan?
- “Did your physician and his/her team answer all of your questions?
- “Did your physician and his/her team listen to your questions or comments without interrupting you?
- “Did anyone ask if you have adequate help at home once you leave the hospital?
- “Did your physician give you in writing the symptoms which would make you need to return the hospital or to get immediate help? Did they explain this in a way you understood?
- “During this hospital stay, how often did doctors treat you with courtesy and respect?
- “During this hospital stay, how often did doctors listen carefully to you?
- “During this hospital stay, did doctors, nurses, or other hospital staff talk with you about whether you would have the help you needed when you left the hospital?
- “During this hospital stay, did you get information in writing about what symptoms or health problems to look out for after you left the hospital?”
Test Sample
“The HCAPS Survey done by the hospital’s vendor only questions a small percentage of the patients (5% or less) we care for. SETMA’s Care Coordination team will question all patients. We will compare our result with the result the hospital gets”.
- “Continue to expand our understanding of HCAHPS and of CAHPS-PCMH
- “Incorporate the following into our hospital care of patients:
- “Knock on the door before entering in order to respect patient privacy
- “Sit at eye level with the patient when addressing their care. Each provider will develop their own “style” some will examine the patient before sitting. Others will sit and talk and then examine the patient but all will talk to the patient rather than talk down at them. There will be exceptions such as in ICU it is not always possible to sit and talk to the patient but is possible to sit when talking to the family.
- “Offer the patient and/or family the opportunity to ask questions or to voice concerns without being interrupted.
- “Beginning with the first visit determine if there are special care needs which must be met before the patient can be safely discharged home. This will include but not be limited to determining if the patient lives alone and if they do to have that documented in the patient’s medical record. (Remember, that ICD-9 and ICD-10’s code has a description of ‘Lives Alone,’ but that SNOMED, which all providers must use by 2015 describes this code as ‘Lives Along - No Help Available.’ This is the critical issue.
- “Also, at the first visit the attending physician will give the Hospital Plan of Care to the patient. This morning the nurse on T3 had placed those on the chart for two new admissions, because she heard me say yesterday that this will be the new SETMA plan. (The nurses especially like our new approach to rounding).
- “Before terminating the visit every provider will ask, “Do you have any other questions or concerns?” “Do you have anything else on your mind that you would like to address.”
- “Here is my contact information; don’t hesitate to call me if you have a question or concern.
- “I know that Dr. _____ is your personal physician. I will make sure that he/she knows that you are here and that he/she knows what is going on with your treatment.
- “Have our Care Coordination include HCAHPS questions in their follow-up telephone calls. This will give us “real time” responses from all of our patient (not just a sampling) which will allow us to measure our own performance quickly) and it will let our patients know we value the quality of their experience.”
Who is included in HCAHPS samples?
- Patients 18 years or older at time of admission
- Include patients of all payer types (not just Medicaid)
- Admission includes at least one overnight stay in the hospital
- Non-psychiatric patients (defined by MSDRG) as principle diagnosis at discharge
- Alive at time of discharge
Who is excluded from HCAHPS samples?
- “No-Publicity” patients
- Court/Law enforcement patients (i.e., prisoners)
- Patients with a foreign home address
- Patients discharged to hospice care
- Patients who are excluded due to state regulations
“With SETMA’s new commitment to master the HCAHPS standards (Hospital Consumer Assessment of Healthcare Providers and Systems), I wondered how SETMA’s commitment work with weekend call. This morning (July 20th), I saw 41 patients at Baptist. It took over five hours. All were treated as described below. Also, knowing that HCAHPS is done only with Fee-for-Service Medicare and Medicaid patients, SETMA has determined to follow the same standards with all patients. Also, knowing that patients discharged with hospice, who expired before discharge, or that are inmates are not included in HCAPS, SETMA will treat these patients as if they are in the HCAHPS Survey, i.e., they will be included in SETMA’s internal HCAHPS Survey.
The following is the summary of the three initiatives which we have undertaken in different responsibilities in the hospital:
Administrative Standards - Medical Records Quality
- All H&Ps on charts were signed.
- All telephone orders in Physicians Orders were signed.
- All discharge orders were written before noon.
Preventive Medicine and Standards of care
- All immunizations particularly pneumovax were brought up to date
- New patients to SETMA were asked if they had a flu shot and when they did that was updated in the EMR
- All patients that did not have a CODE status - had code status addressed
- All hospice eligible patients had hospice addressed.
- All patients who smoked had cessation discussed with them
- The hemoglobin A1C on all patients with Diabetes was reviewed or ordered.
- Knocked on all doors before entering room - this is not new.
- Sat in chair by bedside to talk to all patients - with three exceptions - no chair available or chair too heavy to move.
- Introduced myself and reminded patients of my name - hospital business cards with attending physicians’ picture on the card being printed.
- All patients’ PCP identified and I introduced myself as the representative of their primary care doctor.
- SETMA’s Hospital Plan of Care was given to the patient by me and explained for new admits.
- All patients asked if they had additional questions or issues.
- I intentionally never interrupted a patient, letting them finish their thought and pause before I began talking.
- All patients asked if they have adequate help at home once they leave the hospital.
- All patients ready for discharge had their follow-up care addressed.
- All follow up instructions were discussed with the patient including whom they would see, when and where.
- If any tests results were not back, I let them know when and how they would get the results.
- All patients were treated with courtesy and respect: addressing them by their name and title. Not interrupting them, answering all their questions and asking multiple times if they had anything else they wanted to discuss.
- I made sure that patients understood the vocabulary I used.
We will learn more, but this is a good start. It is only eight days since we began this pilgrimage. The exciting thing is that, we believe this has expanded our understanding of patient-centeredness in the hospital and at the same time, we are learning more about patient-centeredness. In a dialogue about SETMA’s HCAHPS project, Dr. Carols Jaen, Chairman of Family and Community Medicine and The Dr. & Mrs. James L. Holly Distinguished Professor of Patient-Centered Medical Home at the University of Texas Health Science Center at San Antonio School of Medicine shared his article “Have you really you really addressed your patient’s concerns?” The patient/provider dialogue in this article helps further clarify patient-centeredness. That article can be read at http://www.aafp.org/fpm/2008/0300/p35.html.
We expect to complete the Internal SETMA HCAHPS Survey weekly, monthly and quarterly for the next six months. At the end of that time, we expect that our approach to inpatient care will have changed permanently.
|