|
SETMA’s published policy on medication refills is as follows:
Southeast Texas Medical Associates, L.L.P.
Nursing/Clinic Policies & Procedures
POLICY Prescription Refills |
Adoption Date: |
1/12/2004 |
Revised Date: |
5/6/2009 |
Reviewed Date: |
07/30/2009; 12/30/10; 7/11/2013 |
POLICY: To ensure pharmacies receive timely response to refill requests.
PROCEDURE:
- With electronic prescribing capabilities, refills from participating pharmacies will be submitted directly into workflow. Any non participating pharmacy will continue to fax prescription refill authorization requests to the centralized fax line, 839-3131.
- Once it is received, the person responsible will fill medications based on set guidelines. These guidelines include the last office visit, date of last refill, and type of medication desired, etc.
- If the refill does not meet the approval guidelines or is a certain category of medications (such as narcotics), the request will be sent to the provider workflow.
- If the medication is to be refilled, it should be submitted electronically if possible. Any refill authorization must be documented in the EMR by updating the medication profile each time a refill is completed.
- If there are questions or the physician needs to authorize the refill, it must be sent to the provider.
- Once the physician response is obtained, notify the pharmacy and complete the necessary documentation.
- If patients call the pods for a refill, have them contact their pharmacy who in turn is to fax or submit the request electronically.
- If pharmacies call the pods for refills, please direct their calls to the above noted fax line or have it submitted electronically.
- If a refill request is denied document who denied the refill and the reason. Both the patient and the pharmacy should be informed of the denial.
The following standing orders are used to refill prescriptions:
Medications
- Diabetic medications - must have been seen within past 4 months
- Hypertensive meds - must have been seen within past 4 - 6 months
- Cardiac meds - must have been seen within past 4 - 6 months
- Respiratory meds - must have been seen within past 4 - 6 months
- NSAIDs and Cox 2’s - must have been seen within past 3 months
- Seizure meds - forward to pod for refill authorization
- Eye meds - must have been seen within past 12 months
- Thyroid meds - must have been seen within past 12 months
- GI meds - must have been seen within past 6 months
- Pain meds - forwarded to pods for refill authorization
- Psychotropic meds - must have been seen within past 3 months
- Migraine - non-narcotic only - must have been seen within past 6 months
- Antidepressant - must have been seen within past 6 months
- Dermatological - must have been seen within past 6 months
- topicals - must have been seen within past 6 months
- oral antibiotics - must have been seen within past 6 months (need CBC)
- Steroids - must be seen within past 3 months and must be given for specific disease states
- COPD
- Lupus
- Emphysema
- Rheumatoid arthritis
- Inhalers - must be seen within past 3 months
- Antihistamines - must have been seen within past 6 months
- Nasal sprays - must have been seen within past 6 months
- Kids chronic conditions - no auto refill on antibiotics except tetracycline for acne (must have CBC every 6 months)
- Anxiolytics -
- Controlled (benzodiazepines) forwarded to pods for refill authorization
- Others (i.e. Buspar) must have been seen within past 6 months
- Prednisone - forwarded to pods for refill authorization
NO REFILL is to be denied by anyone without first discussing with MD
Medication Reconciliation
Medication issues in ambulatory settings deal more with medication reconciliation than with any other issues. The following addresses the details of medication reconciliation, a systems proposal which SETMA continues to pursue for improved medication reconciliation and an explanation of using SETMA medication module in the EHR.
Why is medication reconciliation a subject worthy of special consideration in a medical home setting? To answer that question, consider active conversations which went on among high school students during the 1940s, 1950s and 1960s. Whereas Latin was and still is a part of a classical education - one of my granddaughters will graduate from high school having had four years of Latin - these discussions were about how the study of Latin would help a student who is interested in medicine as a career. Little did those students know that essentially the only place where Latin was of any use was in writing prescriptions. Some of the common Latin prescription abbreviations used on prescriptions by physicians included:
- ac (ante cibum) means "before meals"
- bid (bis in die) means "twice a day"
- gt (gutta) means "drop"
- hs (hora somni) means "at bedtime"
- od (oculus dexter) means "right eye"
- os (oculus sinister) means "left eye"
- po (per os) means "by mouth"
- pc (post cibum) means "after meals"
- prn (pro re nata) means "as needed"
- q 3 h (quaque 3 hora) means "every 3 hours"
Perhaps, we should include ad nauseam in this list? Fortunately, the use of Latin abbreviations in medicine is decreasing and hopefully will soon be eliminated.
There was a time, actually quite recently, when the "magic and mystery" of medicine was considered part of the art of medicine and often actually probably made people "feel" safer. Patients had enormous trust in their physicians and looked upon them as their most favored and MOST trusted counselors. Prescriptions written in Latin were reassuring to the patient who believed that their very-well-educated physician knew more than they did because he or she could write a prescription which they, the patient, could not understand. Most patients took one or two prescriptions a year. Today that number ranges from 25 to 44 prescriptions a year for patients 65 years-of-age and older, depending upon the State in which the patient lives. Medication regimes are much more complicated and are changed much more frequently.
There were not many medications in the 1940s. In the Health Care financing Review (Winter, 1996/ Volume 18, Number 2, p. 15), it is stated, "Many of the changes in clinical medicine by the early 1960s were the result of pharmaceuticals: the antibiotics, psychotropics, tranquilizers, hormones, and other drugs. It was estimated that 90 percent of the drugs prescribed in 1960 had been introduced in the previous two decades and that 40 percent of the prescriptions could not have been filled in 1954."
The good news was progress increasingly made valuable and useful pharmaceuticals available for treating patients. The bad news was that more and more people were taking multiple medications, some with complicated "sig" codes (written instructions in Latin) and others with an increasing number of serious interactions. The first pitfall in dealing with these interactions is "to rely upon your memory in assessing medication interactions." There are too many of them for any one person to remember all of them.
The following developments created an environment where accurate medication lists in provider records and accurate understanding by patients of what medications they were to take as well as when and how to take them became imperative:
- The number of medications grew; today there are over 10,000 prescription medications and over 300,000 over-the-counter drugs.
- The "magic and mystery" of the medical profession decreased both because of an increasingly knowledgeable populace and because of a decreasing trust in physicians.
- More and more people were taking more and more complex medications
- Medications had increasingly serious and dangerous side effects and interactions.
- Technology created these new medicines and it takes technology to keep track of them.
A major sociological shift took place in the United States as well. Demand increased to take all of the magic and mystery out of medicine. Hospitals required that abbreviations, particularly Latin abbreviations not be used in hospital records. Medication lists given to patients were required to be written in English instead of Latin abbreviation, i.e., instead of "Sig: 1 po qid," medication directions were required to be written in "Directions: one tablet by mouth four times per day."
As early as the mid, 1970s, healthcare professionals and organizations like the Institute for Safe Medication Practices (ISMP), which describes itself as "A Nonprofit organization educating the medical community and consumers about safe medication practices," began to raise the alarm about the need for safe medication practices. In a 2007 publication entitled, Protecting U. S. Citizens From Inappropriate Medication Use, ISMP stated, "3.4 billion prescriptions (were) dispensed in 2005...an increase of nearly 60% since 1995...81% of adults...take at least one medication...and 27% take five."
Magic and Mass: The magic of medicine was gone and the mass of medicines had increased. Both are good things but both require new skills and attentiveness by providers. Medication reconciliation is the most important result of these changes. And, it is still a fact that one of the two most difficult tasks facing all healthcare providers is maintaining an accurate and up-to-date medication list on all patients.
In 2010, the National Quality Forum (NQF) published a study entitled Preferred Practices and Performance Measure for Measuring and Reporting Care Coordination: a Consensus Report. One of the critical quality measures is Medication Reconciliation. One of those measures is described as: 'The plan of care document should include essential clinical data documenting the patient's current state, including, but not limited, to problem lists, medication lists, allergies and risk factors, age-appropriate standardized clinical assessments and screening tests; immunizations status...". Repeatedly, medication reconciliation is included as an essential part of care transitions at every point whether the transfer of care was made from clinic to home, hospital to ambulatory care, emergency department to nursing home, hospital to hospice, hospital to skilled nursing facility, hospital to long term acute care or other transitions.
Physician's Role in Medication Reconciliation (all of the following information is from this AMA monograph)
In 2007, the American Medical Association published its monograph entitled, The Physician's Role in Medication Reconciliation: Issues, Strategies and Safety Principles. The preface gives this warning to physicians: "Medication Reconciliation is essential to optimize the sage and effective use of medications. It is one element in the process of therapeutic use of medications and medication management for which physicians are ultimately held legally accountable..." The document then gives illustrations of harm to patient and legal disasters for physicians when transitions of care were made without effective medication reconciliation.
The AMA documented that in between 2004 and 2005, "in the United States 701,547 patients were treated for an adverse drug event (ADE) in emergency departments and 117,318 patients were hospitalized for injuries caused by an ADE. Insulin, warfarin and other drugs that require monitoring to prevent overdose or toxicity were implicated in one of every seven ADEs treated in emergency departments."
Over-the-counter drugs
The report stated, "Interactions between prescription medications and over-the-counter (OTC) drugs, herbal preparations or supplements are a growing concern, as concurrent sue can lead to serous adverse reactions." And, "in all settings of care, drug-drug interactions are significant but undetected cause of ADEs."
Steps and Principles of Medication Reconciliation - STEPS
- Assembling the lists of medications - notice the word is "lists," not list. In a recent meeting about a regional health information exchange (HIE) an alarm was raised by the potential need to reconcile medication lists from five to ten locations. The response was that the good news was that for the first time, all providers would know that patients were getting medication from multiple sources and providers would have access to the "real" lists for medication reconciliation.
- Ascertaining accuracy (review and compare prior and new lists)
- Reconciling medications and resolving discrepancies
- Formulating a decision, i.e., making a medical judgment, with respect to the patient's condition and medications.
- Optimizing care to best meet the patient's needs with this information.
- Checking the patient's (and/or caretaker's) understanding of their medications
- Documenting changes and providing the patient with a copy of his or her current medication list.
Principles
- Medication reconciliation is a necessary component of safe medication management. The process is ongoing and dynamic
- The medication reconciliation process should be patient-centered.
- Shared accountability between healthcare professionals and patients is essential to successful medication reconciliation outcomes.
- All patients should have an accurate medication list for use across sites of care and over time.
- The medication list should not be limited to prescription drugs.
- Within all settings, the medication reconciliation process should happen at every medication encounter, regardless of the care location.
- Across all setting, the medication reconciliation process must happen at every transition in the patient's care, regardless of the care transition.
- The process of medication reconciliation is interdisciplinary and interdependent - and reliant on a team approach.
- Physicians are ultimately responsible both ethically and legally for the medication reconciliations process.
- Some medication information may be emotionally or legally charged, but nevertheless significant. It may be added at the discretion of the patient or prescribing health care professional by mutual consent.
Questions which will help with Medication Reconciliation
- What medications do you take? Can you tell me the names of all your medications, including vitamins, OTC drugs, supplements and neutraceuticals.
- What is it important to take your medications?
- When do you take this medication? How long have you been taking this medication? Do you have a medical condition? What medical Condition?(s) do you have? What did you doctor say to you about this medication?
- How do you take your medications (e.g., time of day, with food)?
- Are you taking you medications the way the doctor told you to? When was the last time you took it? When was the time before that?
- What do you do when you make a mistake? Do you every skip medication or take tow when you miss a dose?
- Is your medication making you feel better or worse or no change?
- What other medications, herbals, supplement, neutraceuticals, drops or sprays are you taking? Do you take other drugs that a physician has not prescribed?
- From where do you get your medications? A local pharmacy? Mail order? The Internet? From another country? Other?
- Who buys the medications in your family? Should we talk to him or her to make sue we have a complete list of all the medicines you take?
Giving Patients a List of Medications at Each Care Encounter
Reconciled Medication lists should be given to all patients at every point of transitioning of care and should include the following:
- A Reconciled List of Medications including Over the Counter, Herbal and Supplements
- Instructions in English (not Latin) for dosage, directions and timing of prescription
- A list of the patients allergies
- The date and time of the Reconciliation
- The person who did the reconciliation
- The contact information for the Reconciliation
Strategies to Assist Patient Understanding
- Use plain, nonmedical language.
- Slow down
- Break information down, use short statements.
- "Chunk and check" or organize information into tow or three key concepts, then check for understanding. Aim for a fifth to sixth grade reading level on all written information.
- Use communication aids to assist in conversations, discussions or education sessions with patients, families and care givers.
- Offer to read materials aloud and explain
- Underline, highlight or circle key points.
- Provider a trained interpreter, when appropriate.
- Use visual aids to help patients navigate the health care system and understand health information.
- Ask patients to teach-back what they were told.
- We have gone over a log of information. In your own words, can you review for me what we have discussed? How will you make it work at home?
- Sometimes I give a lot of information. Can you let me know what you heard me say? This helps me make sure I gave you the information you want and need/
Conclusion
Medication Reconciliation is hard and it is critical. The dynamic nature of medications being taken creates the complexity of maintaining and accurate lists as does the fact that most patients on multiple medications are being seen by two to seven providers annually. The probability for medication reconciliation to result in accuracy in medication administration is increased by the frequency of reconciliation being completed, particularly when each reconciliation is thorough. If a patient has ten to fifteen medication reconciliations or more per year, adverse medication events will decline and hopefully disappear. Such reconciliations are time consuming and require perseverance, but the result will be increased safety and improved care with decreased cost.
A Modest Proposal - A Systems Approach to Medical Reconciliation
SETMA believes that a system’s solution (see Peter Senge, The Fifth Discipline, “The more complex a problem the more systemic the solution must be.”) to medication reconciliation would be a huge step forward in patient safety and in the pursuit of the Triple Aim. Whether addressing care transitions, care coordination, hospital readmissions, or patient safety, medication reconciliation is a key element of success. In preparation for a visit October 29-November 1, 2012 from a Robert Wood Johnson Foundation research team (see the following link for a description of their research project The Primary Care Team: Learning from Effective Ambulatory Practices (PCT-LEAP): Performance Measures Worksheet - Robert Wood Johnson Foundation, SETMA prepared a 57-page document describing SETMA’s auditing and quality programs. The link above will guide readers to that document. The document addresses SETMA’s solution to care transitions, care coordination, etc.. The AMA’s monograph, The physician’s role in medication reconciliation Issues, strategies and safety principles (Making Strides in Safety® program ©2007 American Medical Association), AHRQ’s Medications at Transitions and Clinical Handoffs (MATCH) Toolkit for Medication Reconciliation, and other studies support the potential benefit for a structured, systemic solution to medication reconciliation.
In addition to effective care transitions (the following link is to SETMA’s performance on the PCPI Care Transitions Measurement Set for 2009, 2010, 2011 and 2012 PCPI Care Transitions -- the next link is to the public reporting by provider name for 2012 Care Transition Audit (Section A), SETMA has established the following steps and principles for medication reconciliation:
Steps and Principles of Medication Reconciliation
Steps:
- Assembling the lists of medications - notice the word is "lists," not list. In a recent meeting about a regional health information exchange (HIE) an alarm was raised by the potential need to reconcile medication lists from five to ten locations. The response was that the good news was that for the first time, all providers would know that patients were getting medication from multiple sources and providers would have access to the "real" lists for medication reconciliation.
- Ascertaining accuracy (review and compare prior and new lists)
- Reconciling medications and resolving discrepancies
- Formulating a decision, i.e., making a medical judgment, with respect to the patient's condition and medications.
- Optimizing care to best meet the patient's needs with this information.
- Checking the patient's (and/or caretaker's) understanding of their medications
- Documenting changes and providing the patient with a copy of his or her current medication list.
Principles
- Medication reconciliation is a necessary component of safe medication management. The process is ongoing and dynamic
- The medication reconciliation process should be patient-centered.
- Shared accountability between healthcare professionals and patients is essential to successful medication reconciliation outcomes.
- All patients should have an accurate medication list for use across sites of care and over time.
- The medication list should not be limited to prescription drugs.
- Within all settings, the medication reconciliation process should happen at every medication encounter, regardless of the care location.
- Across all setting, the medication reconciliation process must happen at every transition in the patient's care, regardless of the care transition.
- The process of medication reconciliation is interdisciplinary and interdependent - and reliant on a team approach.
- Physicians are ultimately responsible both ethically and legally for the medication reconciliations process.
- Some medication information may be emotionally or legally charged, but nevertheless significant. It may be added at the discretion of the patient or prescribing health care professional by mutual consent.
We think that forming a coalition with pharmacies, clinicians, patients and IT technology could result in a solution to medication reconciliations which could:
- Reduce the time involved in medication reconciliation to less than two minutes
- Advance a practice closer to perfect medication lists
- Make it easy to reconcile medications at every contact and even when the patient is not schedule for a visit.
- Increase patient safety
If a D. Pharm consultant is involved in the process, it would even be stronger.
Progress as of October 29, 2012 Progress today on our medication reconciliation. Four key parts of our solution:
- Record of filled prescriptions from pharmacy -- SureSscripts already gets this information and it is available through our EMR vendor. This is an existing solution to a big part of the puzzle.
- Bar coding of medication bottles from pharmacies -- Most pharmacies and all of the chains already use bar coding. The biggest hurdle is to get scanners in medical offices that read the bar coding and that deposit the information into the EMR. Each chain has its own bar coding. We can work toward harmonization and get a short term fix.
- Have patient review their own medication list as it appears in their personal health record -- This can be done with our existing secure web portal.
- Reconciling medications via connection between template and medication module -- this can be done. It is awkward but should be able to be improved by our EMR vendor.
Meetings this week with EMR vendor and pharmacist. Should have information on bar coding this week
Restating the Goal
- take 300 of SETMA's patients,
- all with complex medication issues,
- get them linked to our secure web portal.
- Identify ten pharmacies who do bar coding and
- are who are willing to work with us.
- Get those linked to our HIE and hopefully
- in 90 days be able to initiate the project which is identified in the document attached above.
October 31, 2012 -- A Brief Description of the Proposal
- A patient makes an appointment and the following occurs automatically,
- A select group of pharmacies agrees to deploy a “bar coding” for all prescriptions filled for a test group of patients 2-300. The bar code would include the following information:
- Name of patient
- Name of pharmacy
- Name and strength of medication
- Quantity
- Dosing
- Last refilled
- Refills available
- Triggered only by the making of an appointment, a secure, HIPPA compliant request is sent to multiple pharmacies requesting a list of all medications filled in the past 90 days.
- Triggered only by the making of an appointment, a secure, HIPPA compliant note is sent to the patient with a list of the medications (including over-the-counter medications and neuraceuticals) which the EHR says the patient is on and the patient responds with a notation of whether they are on the medications listed, or not, and/or if they are on other medications not listed.
- When the patient arrives in the clinic with the bottles or containers for all current medications, the bar codes are scanned.
A Medication Reconciliation template is automatically populated with four columns:
- The medications which have been filled by the pharmacies
- The medications the patient says he/she is on
- The medications the EHR says the patient is on
- A list of the bar-coded meds scanned at the beginning of the visit
These listed will be organized and color codes as follows:
- All medications which appear on all four lists and are of the same dosage and frequency will appear first and in black (but even these are reviewed by the provider during the reconciliation)
- All medications which are in conflict for any of the following reasons will be high lighted in red:
- They violate a drug/drug interaction
- They violate a patient/drug allergy
- They violate a drug/condition interaction
- Any medication which appears on less than all four lists will be high lighted in red.
The template functionality will allow for the addition or deletion of any medication by the single click of a button over that drug. Once this process is complete, a current medication list will be created with:
- All medications which should be continued
- All medications which have been discontinued
- All medications where a dosage, frequency or timing of dosing will be listed with the new instructions in common language.
- This will be available for everyone in English and Spanish and by special arrangement in other languages as well.
An Introduction to the Medication module - How to use SETMA’s EMR Medication Module
Whether completing a clinic patient evaluation, a hospital admission history and physical, a discharge summary, a hospital order set, a disease management tool, or a nursing home visit, one of the key elements of excellent documentation is an accurate, complete andcurrentlist of medications
In addition, it is imperative that discrete, objective and clear directions for use be included in the medications list. Terms such as "as directed" and "prn," are ambiguous and not helpful, particularly for critical medications such as insulin and coumadin.
The term "SIG" refers to the directions for the use of a medication. Derived from Latin the archaic references in patient medication instructions provide opportunities for medication errors, therefore there is a national effort to eliminate the old Latin "SIG" codes and replace them with English language equivalents, i.e., instead of saying "1 po qid," the new English Language "SIG" code will state, "one by mouth four times a day."
Again, imprecise terms such as "as directed," are never to be used under any circumstance for any reason. The term is meaningless to anyone but the person who gave it, and after a few days, that person would not be able to consistently determine precisely what he/she had told the patient. And, the term does not give the patient or pharmacist clear and precise directions for how the medication is to be used. And, if the term "prn" is to be used, it must be accompanied by the frequency and the indications for the "as needed" directions, i.e., instead of "prn," the SIG code should be "one tablet by mouth every three to four hours as needed for pain."
NextGen's Medication Module has two "windows" for detailing the directions for the use of any medication:
- SIG: this is a limited-space window in which the traditional Latin SIG is placed, i.e., 1 po qid. The system will require you to place such a SIG code in this window in order to properly complete a prescription.
- SIG desc: this is a space with much more capacity in which a precise, English-language description of the medication instructions should be placed, i.e. one tablet by mouth four times a day.
Both SIG codes will appear on all of the various documents - prescription, Rx Sheet, chart note, discharge summary, nursing home note, disease management follow-up notes, etc. - which are generated through NextGen.
Using the medication module
Medication Module Tutorial
The Medication Module is accessed from the NextGen Main Tool Bar. The Main Tool Bar is displayed by the following steps:
- Open a patient’s chart in NextGen.
- Make sure the visit is not a locked visit.
- At the top of the NextGen screen and to the right, you will see four buttons which are beside the space where the provider’s name appears.
- If you place your cursor over the second button, its name will appear: "Show/Hide the History ToolBar."
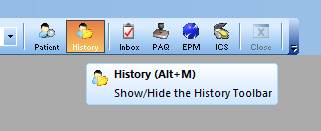
- When the bar is closed, clicking on this button will open it; when it is open, clicking on this button will close it.
- When navigating through NextGen, you should close the Main Tool bar except when using:
- The Medication Module
- The Allergy Module
- The laboratory Module
- The Template access button
- The Document Generator
To learn more about Navigating within NextGen - Click Here
Now that the Main Tool Bar is displayed, you will see nine icons at the bottom.

Click on the Icon at the bottom left of the nine which has a "Rx" on a symbol which looks like a Mortar and Pestle. Once again, if you place your cursor over the icon and leave it there for a second, the name of the Icon will appear.

Clicking on the Rx Icon launches the Medication Module.
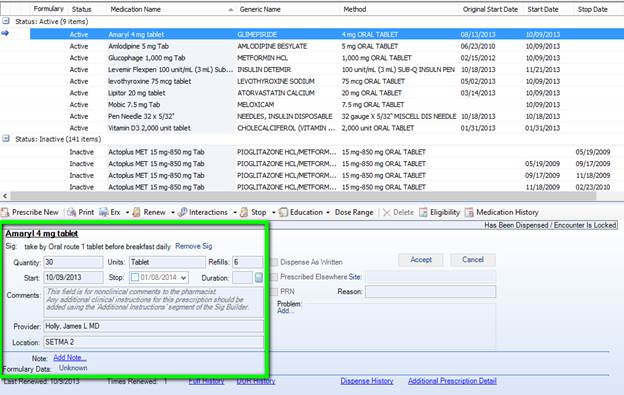
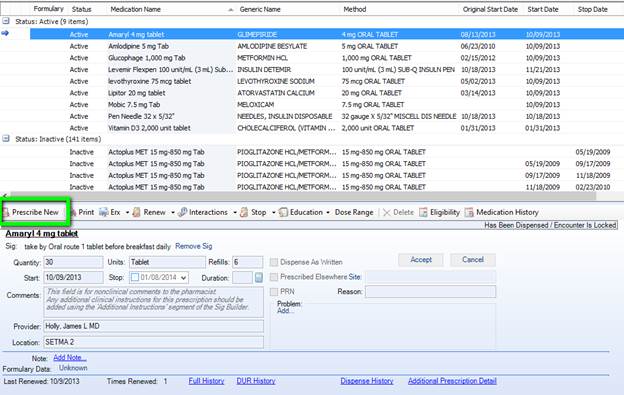
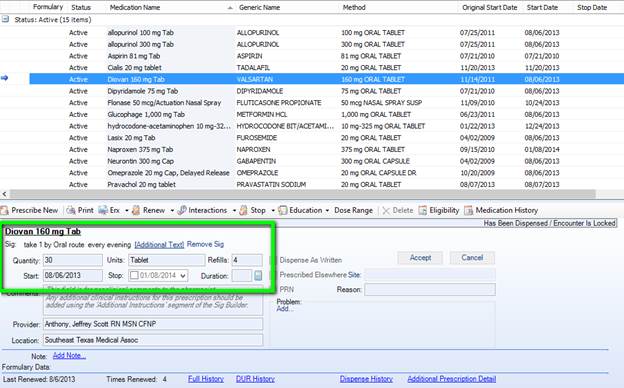
In the window at the top of the Module, you will see a list of medications which the patient is one, or has been on. In a bar across the top of this window there are a number of boxes which lists the various elements of the medications which are documented in the window below. The patient’s active medications are listed at the top under “Status: Active” and you can also see their medication history of their previous medications under “Status: Inactive.”
In order to see all of these you may have to scroll to the right.
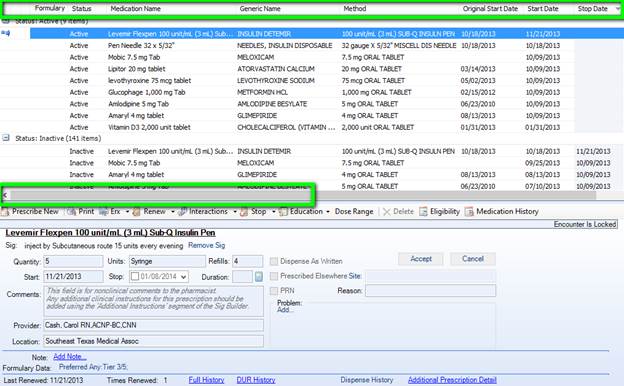
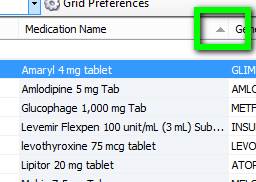
In addition to providing a wealth of information about each drug that is prescribed for a patient, these buttons can be used to sort and display the medications in any order you wish.
For instance, if you click on "medication" the list will be sorted alphabetically; if you click on "start date," the medications will be displayed in the order of their "start date," and so on.
The Toolbar below the Medications Window

Underneath the window which displays the medications, there is a toolbar with the following functions:
- Prescribe New - this will allow you to add a new medication.
- Print - this will print the prescriptions which you have ordered for the present evaluation in a crystal report format.
- Stop - this button places an "I" beside the prescription and places it in the "inactive" list which will appear in the medication window after the "active" or currently prescribed medications. This function allows you to maintain an accurate and complete record of the patient’s prescription history easily and efficiently.
- Interactions - this button launches the NextGen function which indicates if any of the medications you are prescribing interact with any other medications, and, if the patient’s allergy history has been completed, it indicates whether or not the patient is allergic to this medication, or to an ingredient in the medication.
When the interaction button is executed and when there is an interaction between the highlighted medication and another medication which has been prescribed for the patient, and/or the patient is allergic to the medication, a pop-up will appear giving the following information:
Patient Allergy -- with a description of the medication which the patient is allergic to. The significance is always a level 1 for a patient-specific-medication allergy.
Drug/Drug interactions - a list of the medications which interact with one another if any. The following information is given:
- Conflicts with - the medication with which the selected medication interferes will be identified here.
- Description - the nature of the conflict with the identified here.
- Start Date
- Stop Date
- Effect - a code is given here with three letters. This can be ignored as the full description of the effect is given as indicated below.
- Level - levels 1 to 3 are given. Level 1 and 2 are very important and should rarely be ignored if ever.
If you click on the information which is displayed in this window, the nature of the interaction appears at the bottom of this window with both the effect and the level being described in detail.
Also, the button entitled Monograph will be activated so that you can print a document which will give more detail about the interaction between the two medications.
There are three levels of interaction which are noted by NextGen. They and their description and significance are:
- Level 3 -- Possibly significant - conservative measures are recommended until more known (little clinical date exists)
- Level 2 - Significant - assess risk to patient and take action as needed
- Level 1 - Most significant - action to reduce adverse effect of interaction is usually required.
Remember, Level 1 cautions should not be ignored and should rarely, if ever, be overridden.
- Education - this button launches a monograph on the medication which is highlighted. This gives enough information to help a patient but is not the complete prescribing information for a medication and should not be relied upon by the provider who is unfamiliar with the particular drug.
- Dosing Range - this button launches a pop-up with describes the name and dose of the drug being prescribed. The age range for use of the medication, along with the following information is given:
- Minimum dose quantity
- Minimum dose units
- Maximum dose quantity
- Maximum dose units
- Note - this is a "read only" function which displays the note which was created at the time of the original prescription if any. (see below)
Selecting Medications and the Prescribing and Sig Code Function of NextGen
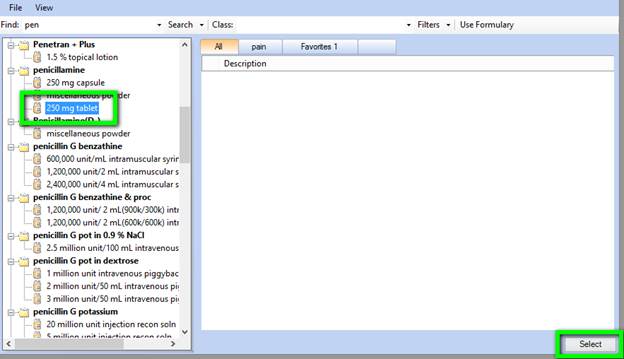
Prescribe New - When the "Prescribe New" button is clicked, a window opens which has the following on it:
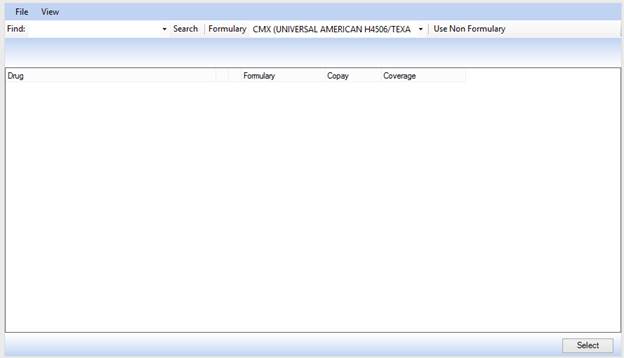
- By clicking in the window above next to “Find:” you will be able to type in the first few letters of the name of the medication which you wish to add.
- After typing in the first few letters of the medications name, click "Search."
The medications with that string of letters in the beginning of its name will be displayed.
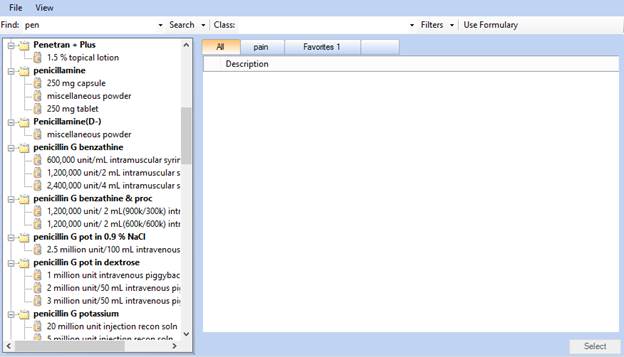
- Once a list of medications appears, you will double click on the one you wish to select or highlight it and click the "Select" button.
The second column contains:
- Start - the date on which the prescription was issued. The current date is automatically selected by the system for a new or renewal medication.
- Stop - the stop date, if designated, for when the medication should be discontinued. A stop date can be added by clicking the button to the right of the Stop date window and adding the appropriate date via the calendar which appears.
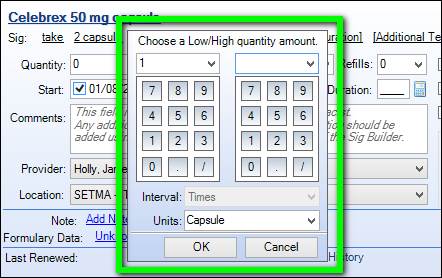
- Quantity - the number of pills, tablets, capsules, suppositories, etc., which were authorized to be issued to the patient. The number of pills, etc., can be designated by clicking the button to the right of the quantity window and using the number pad which appears.
- Refills - the number of refills which are authorized if any. The button beside this window triggers a number pad which allows the number of refills to be added. Remember, for most medications, to determine how many pills you have given, you must multiple by quantity by the number of refills + 1, i.e., if you give 90 pills and 3 refills you have prescribed 90 x 4 or 360 pills.
If you have not used a medication before or if you have giving new and unique instructions, you will need to use the SIG code builder to create a new SIG code. Here are the steps to do this.
- First, by clicking “Add Sig” below right of the medication name, you will be asked to choose the administration method for the medication.
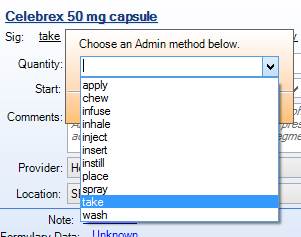
- Once you select the administration method, a default sig will appear.
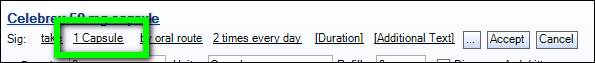
- The default sig will be broken into pieces, separated by spaces. You may click on each piece to edit it as shown below. In this example, by clicking on “2 capsule” you are prompted to enter a new quantity and units which here was changed to “1 capsule.”
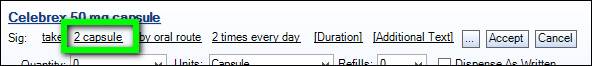
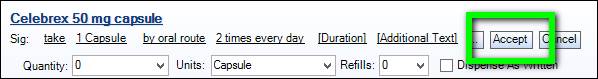
- Once you have edited all of the pieces of the SIG that you need to change, you click “Accept” to finalize the changes. The new SIG that you entered will be the SIG used for this medication.
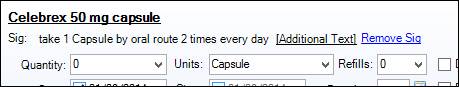
- The final SIG will be displayed. If you need to add additional text or start over, you may click the “Additional Text” to add information or “Remove SIG” to start over.
General Principles of use of the Medication Module and functions which extend from it.
- The Nursing staff must review the patient’s medications as a part of their check in, EVERY visit on EVERY patient. There is no exception to this.
- The patient must be given an Rx Sheet -- which contains an accurate and updated list of the patient's medications.
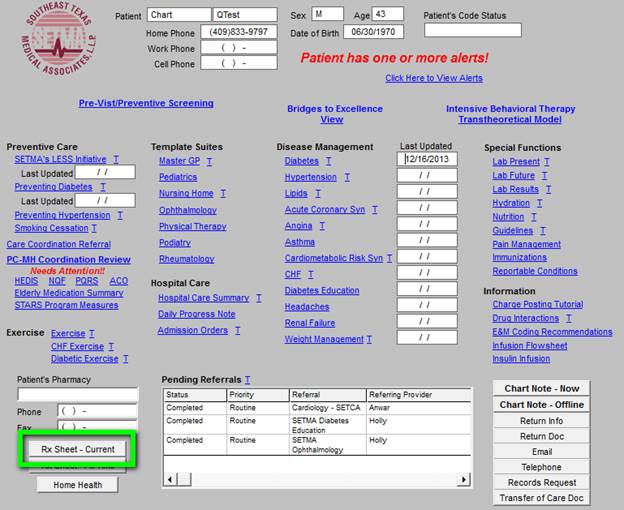
To generate an Rx Sheet, go to the Plan Template or to AAA Home and click on the button entitled "Rx Sheet - Current" at the bottom left of the screen. An accurate list of the patient's current list of medications with name, dose, sig code in Latin and English will be automatically printed. This should be done with every patient, every time they are seen.
- If the description Sig code is in "qd," "po" or other Latin language, the description must be changed to "my mouth," "once a day," etc.
- This function particularly means inactivating medications which are no longer being taken.
- As part of his/her evaluation every provider needs to document on every encounter that the medications have been reviewed AND the medications must be reviewed. Old, discontinued and inactive medications need to be marked as such.
- Imprecise and indefinite Sig Codes such as "As Directed" are NEVER permissible.
- Many Coumadin orders on patients have an "As Directed" sig code. What does that mean?
- Sig codes must be precise and accurate, particularly for Insulin, Lanoxin, Potassium, Coumadin and other medications which have a narrow window between therapeutic and toxic doses.
- Don't forget, the description must be in English.
- Also, a new Federal regulation requires that Sig codes in the hospital be in English, not Latin, i.e., the old code of "1 po qd," is not acceptable. The directions must state "one by mouth once every other day."
Until you have modified the Sig codes you most often use, you will have to, rather laboriously, place the correct English translation of the Sig code in the "Description window" on the Medication template. This now prints on the prescription form, on the chart note, on the Rx Sheet and on all disease management tools patient follow-up documents.
- Those who are completing H&Ps for hospital admissions must NOT put any chart note on a patient's chart until the sig codes have been updated and until all inactive medications have been eliminated.
- This is particularly true if some of the outpatient meds are not to be continued in the hospital.
- Remember, the meds in the patient's record will appear on the hospital order set.
- Once a correct chart note with all currently prescribed and active medications is generated, the medication list must be modified again before the hospital order set is generated, i.e., if the patient is on Coumadin as an outpatient, that fact and the correct English language Sig Code needs to appear on the admission History and Physical Examination.
- However, if the patient is not to continue the Coumadin in the hospital, once the H&P is generated, the Coumadin must be inactivated so that it does not appear on the Hospital order set.
- All descriptions for medications must have an English language description in the Sig before the hospital order set is printed.
|