|
September 26, 2010
Mr. Fred W. Heldenfels IV
President, Heldenfels Enterprises, Inc.
5700 IH-35 S
San Marcos Texas 78666
Dear Mr. Heldenfels:
This letter is in regard to your role as Chairmanship of the Texas Higher Education Coordinating Board. In that I am not a Board Member and do not have the opportunity to testify before your Board, I trust that you will review this letter in regard to your consideration of several University of Texas Doctor of Nurse Practitioner Degree Programs.
I am a practicing physician and a graduate of the University Of Texas Health Science Center at San Antonio School of Medicine, class of 1973. I am the CEO, of a moderate sized multi-specialty clinic, Southeast Texas Medical Associates, LLP (www.jameslhollymd.com, SETMA). I have practiced in Beaumont for thirty-six years. SETMA was formed in 1996 and in 1997, employed the first of more than twenty nurse practitioners. In the Addendum A to this letter, I have given you some facts about SETMA which may allow you to evaluate my qualifications for commenting on this subject.
SETMA has employed two providers who have the Doctor of Nurse Practitioner (DPN) degrees. One of these worked with SETMA for the entire three years of his doctoral program through the University of Texas Health Science Center at Houston School of Nursing. He also served as the Chief Medical Officer, Office of Evidenced-Based Medicine, in SETMA. This experience has given me an excellent introduction to the content and intent of the DNP program.
My personal healthcare provider and my wife’s personal healthcare provider are both Nurse Practitioners. In no way does this disparage my physician colleagues who are outstanding and greatly respected, but it does indicate the confidence which I have in the clinical acumen and expertise of my NP and DNP colleagues. This experience has led my wife and me to endow a Distinguished Professorship at the San Antonio Health Science Center which is multi-disciplinary and interdepartmental between Pediatrics, Doctor of Nurse Practitioner, Internal Medicine and Family Medicine. The Professorship is to promote the patient-centered medical home model of healthcare delivery.
Increasingly, the practice of medicine needs the special skills and training of DNPs who are deeply immersed in statistical analysis, population-healthcare management and coordination and patient-centric nature of the “new” medicine. The DNP program provides a technical expertise and a perspective which perfect supplements the physician role in the future of medicine.
Most physicians have not had the opportunities which I have in order to appreciate the value of the nurse practitioners role and now the doctor of nurse practitioner role. In an article for my weekly column for October 21.m 2009 entitled, Re-Evaluating the Value of Members of the Healthcare Team, I said:
“It is easily recognized in this emerging paradigm that all of the schools in the academic healthcare center are actively involved in patient care and in the training of those who will be healthcare providers. Yet, it seems that the farther and farther a person advances in biomedical education, the obvious union of their disciplines at their foundations seems to be lost and the more isolated from the whole these ‘specialists’ and ‘experts” become.
“This even creates problems within the various disciplines as egocentrism isolates one medical specialty from another. It is as a result of the need for the integration of healthcare disciplines at the delivery level, that the imperative becomes obvious for the restructuring of the training of the members of this healthcare team.
“And, the first change must come in the relationships between the leaders of the training programs who educate and mentor future healthcare scientist, teachers, caregivers and researchers. The educational leaders must model this integration for their disparate student bodies and that modeling will require the investment of the most precious and rare resource: time.”
I would implore you and your Board to look favorably upon accredited Schools of Nursing proposing to offer Doctor of Nurse Practitioners programs. If it should ever be judged by you as worthy of your time, I would be pleased to present additional information to you, or to your Board in writing, or in person, as you desire.
Thank you your kind attention to this information and to the two addenda. Please distribute a copy of this letter and the Addenda to other members of the Board.
Sincerely Yours,
James L. Holly, MD
CEO, SETMA, LLP
www.jameslhollymd.com
Addendum A - Introduction to SETMA
Addendum B - SETMA’s Model of Care
Addendum A
SETMA has multiple designations and awards which have given us a unique perspective upon the future of healthcare as to substance, .
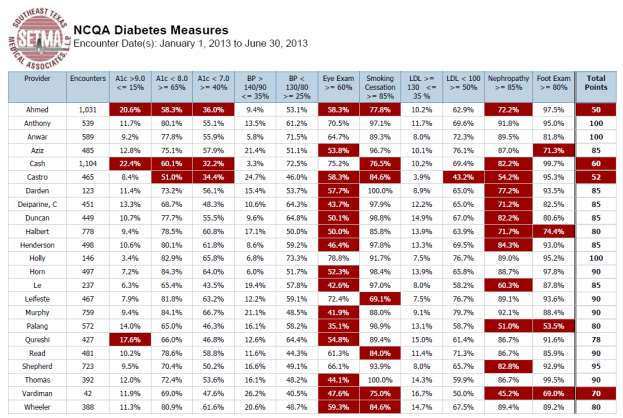
- National Committee for Quality Assurance both Tier III Patient-Centered Medical Home and NCQA Diabetes Recognition Program.
- Joslin Diabetes Center Affiliate - SETMA is the only multi-specialty affiliate of Joslin. All providers, physicians Certified Family Nurse Practitioners and DNPs have been awarded Joslin Certified Primary Care Providers after study, testing, interviews and participation in seminars.
- Accreditation Association of Ambulatory Health Care accreditation for Ambulatory Care and for Medical Home.
- Three agencies of Health and Human Services have extended special recognition to SETMA:
- Office of National Coordinator named SETMA as one of 30 exemplary practices for clinical decision support.
- Agency for Healthcare Research and Quality published SETMA’s LESS Initiative on its Innovation Exchange.
- Centers For Medicare and Medicaid included SETMA in a quality, cost and coordination of care research project in which SETMA outperformed all others on quality and equaled the best in cost control for 2007-2010.
In our fourteen year history in using electronic health records (EHR), we have developed an understanding of the future of health care as to:
- The Substance - Evidenced-based medicine and comprehensive health promotion
- The Method - Electronic Patient Management
- The Dynamic - Patient-Centered Medical Home
- The Funding - Capitation and payment for Quality
Founded on these four domains, SETMA’s Model of Care includes the following:
- Personal Performance Tracking-- One patient at a time
- Auditing of Performance-- By panel or population
- Analysis of Provider Performance -- Statistical Analysis
- Public Reporting by Provider Name -- At www.jameslhollymd.com
- Quality Assessment and Performance Improvement
At www.jameslhollymd.com, the following articles written by SETMA can be found (number of articles is in parentheses):
- Tutorials on all Electronic-Patient-Management tools including Diabetes, Diabetes. Prevention, Hypertension Prevention and others (67)
- Diabetes (25)
- Smoking Cessation (15)
- Exercise (40)
- Weight Reduction (33)
- Cardiovascular Disease Risk Factors (22)
- LESS Initiative (66)
- Medical Home (46)
- Healthcare Reform and Public Policy (24)
- Many more
Addendum B
The Future of Healthcare Innovation and Change: SETMA’s Model of Care Patient-Centered Medical Home
By James L. Holly CEO, SETMA, LLP www.jameslhollymd.com
There are at least three hundred models of care described in the medical literature. Each one was defined to improve care of patients while focusing on a particular aspect or method of care. As healthcare policy and plans have defined new goals for our healthcare system, they have suggested even newer models of care. The Institute for Healthcare Improvement (IHI) defined the Triple Aim in 2007. The goals of improving patients’ experience of care, improving community health and decreasing healthcare cost have led to and provided increased incentive for new structures of healthcare delivery, chief among those has been patient-centered medical home.
As SETMA has worked both to qualify and to function as a patient-centered medical home (PC-MH), we defined a model of care which is different from previously published ones. With this October, 2013, update of The Future of Healthcare, Innovation and Change, SETMA’s Model of Care, patient-Centered Medical Home, SETMA has qualified as an NCQA Tier III PC-MH (2010-3016) and as an AAAHC medical home (2010-2014). In October we will submit application to URAC and in February, 2014 to Joint Commission for accreditation as a PC-MH.
As this iteration of our Model of Care description is prepared in October, 2013, we believe that in the last three to six months, we have begun to understand and to function as a “real” medical home. Terms like “shared decision making”, “patient activation”, “patient engagement”, “patient-centered conversation”, “care coordination”, “coordinated care”, and “care transitions” are more than vocabulary with definitions. They are real to us, in experience, and form the dynamic of what was initially a structure of PC-MH.
Hospital Consumer Assessment of Healthcare Provider and Systems (HCAHPS) and ambulatory Consumer Assessment of Healthcare Provider and Systems (CAHPS) are now part of our measurement of patient-centeredness in our practice. Increasingly, we think, we understand PC-MH principles and practice. Remarkably, patients have been overheard making statements like, “Have you been to SETMA recently? Something has changed.” That change has been that SETMA has learned the dynamic of PC-MH.
Transformation
SETMA believes that the key to the future of healthcare is an internalized ideal and a personal passion for excellence rather than reform which comes from external pressure. Transformation is self-sustaining, generative and creative. In this context, SETMA believes that efforts to transform healthcare may fail unless four strategies are employed, upon which SETMA depends in its transformative efforts:
- The methodology of healthcare must be electronic patient management.
- The content and standards of healthcare delivery must be evidenced-based medicine.
- The structure and organization of healthcare delivery must be patient-centered medical home.
- The payment methodology of healthcare delivery must be that of capitation with additional reimbursement for proved quality performance and cost savings.
At the core of these four principles is SETMA"s belief and practice that one or two quality metrics will have little impact upon the processes and outcomes of healthcare delivery and, they do little to reflect quality outcomes in healthcare delivery. In the Centers for Medicare and Medicaid Services (CMS) Physician Quality Reporting System (PQRS), healthcare providers are required to report on at least three quality metrics. This is a minimalist approach to providers quality reporting and is unlikely to change healthcare outcomes or quality. PQRS allows for the reporting of additional metrics and SETMA reports on 28 PQRS measures.
SETMA employs two definitions in our transformative approach to healthcare:
- A “cluster” is seven or more quality metrics for a single condition, i.e., diabetes, hypertension, etc.
- A “galaxy” is multiple clusters for the same patient, i.e., diabetes, hypertension, lipids, CHF, etc.
SETMA believes that fulfilling a single or a few quality metrics does not change outcomes, but fulfilling “clusters” and “galaxies” of metrics, which are measurable at the point-of-care, can and will change outcomes. The following illustrates the principle of a “cluster” of quality metrics. A single patient, at a single visit, for a single condition, will have eight or more quality metrics fulfilled for a condition, which WILL change the outcome of that patient’s treatment.
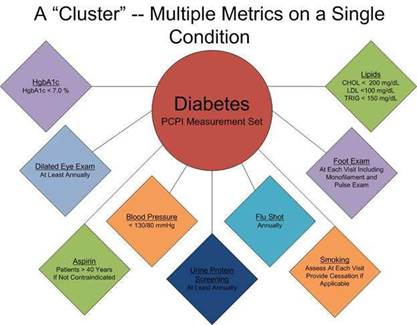
The following illustrates a “galaxy” of quality metrics. A single patient, at a single visit, may multiple “clusters” surrounding multiple chronic conditions thus having 60 or more quality metrics fulfilled in his/her care, which WILL change the quality of outcomes and will result in the improvement of the patient’s health. And, because of the improvement in care and health, the cost of that patient’s care will decrease as well.

SETMA"s model of care is based on these four principles and the concepts of “clusters” and “galaxies” of quality metrics. Foundational to this concept is that the fulfillment of quality metrics is incidental to excellent care rather than being the intention of that care.
Quality Metrics Philosophy
SETMA's approach to quality metrics and public reporting is driven by these assumptions:
- Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care.
- Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare“Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there.
- The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, butthe guide posts to that destination are given by the analysis of patient and patient- population data.
- There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- The collection of quality metrics should be incidental to the care patients are receiving and should not be the object of care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
The Limitations of Quality Metrics
The New York Times Magazine of May 2, 2010, published an article entitled, "The Data-Driven Life," which asked the question, "Technology has made it feasible not only to measure our most basic habits but also to evaluate them. Does measuring what we eat or how much we sleep or how often we do the dishes change how we think about ourselves?" Further, the article asked, "What happens when technology can calculate and analyze every quotidian thing that happened to you today?" Does this remind you of Einstein's admonition, "Not everything that can be counted counts, and not everything that counts can be counted?"
Technology must never blind us to the human. Bioethicist, Onora O'Neill, commented about our technological obsession with measuring things. In doing so, she echoes the Einstein dictum that not everything that is counted counts. She said, "In theory again the new culture of accountability and audit makes professionals and institutions more accountable for good performance. This is manifest in the rhetoric of improvement and rising standards, of efficiency gains and best practices, of respect for patients and pupils and employees. But beneath this admirable rhetoric the real focus is on performance indicators chosen for ease of measurement and control rather than because they measure accurately what the quality of performance is."
Technology Can Deal with Disease but Cannot Produce Health
In our quest for excellence, we must not be seduced by technology with its numbers and tables. This is particularly the case in healthcare. In the future of medicine, the tension - not a conflict but a dynamic balance - must be properly maintained between humanity and technology. Technology can contribute to the solving of many of our disease problems but ultimately cannot solve the "health problems" we face. The entire focus and energy of "health home" is to rediscover the trusting bond between patient and provider. In the "health home," technology becomes a tool to be used and not an end to be pursued. The outcomes of technology alone are not as satisfying as those where trust and technology are properly balanced in healthcare delivery.
Our grandchildren's generation will experience healthcare methods and possibilities which seem like science fiction to us today. Yet, that technology risks decreasing the value of our lives, if we do not in the midst of technology retain our humanity. As we celebrate science, we must not fail to embrace the minister, the ethicist, the humanist, the theologian, indeed the ones who remind us that being the bionic man or women will not make us more human, but it seriously risks causing us to being dehumanized. And in doing so, we may just find the right balance between technology and trust and thereby find the solution to the cost of healthcare.
It is in this context that SETMA whole-heartedly embraces technology and science, while retaining the sense of person in our daily responsibilities of caring for persons. Quality metrics have made us better healthcare providers. The public reporting of our performance of those metrics has made us better clinician/scientist. But what makes us better healthcare providers is our caring for people.
Team Approach to Healthcare Delivery
The ideal setting in which to deliver and to receive healthcare is one in which all healthcare providers value the participation by all other members of the healthcare-delivery team. In fact, that is the imperative of Medical Home. Without an active team with team-consciousness and team-collegiality, Medical Home is just a name which is imposed upon the current means of caring for the needs of others. And, as we have seen in the past, the lack of a team approach at every level and in every department of medicine creates inefficiency, increased cost, potential for errors and it actually eviscerates the potential strength of the healthcare system.
Why is this? Typically, it is because healthcare providers in one discipline are trained in isolation from healthcare providers of a different discipline. Or, they are in the same buildings and often are seeing the same patients but they rarely interact. Even their medical record documentation is often done in compartmentalized paper records, which are rarely reviewed by anyone but members of their own discipline. This is where the first benefit of technology can help resolve some of this dysfunction. Electronic health records (EHR), or electronic medical records (EMR) help because everyone uses a common data base which is being built by every other member of the team regardless of discipline. While the use of EMR is not universal in academic medical centers, the growth of its use will enable the design and function of records to be more interactive between the various schools of the academic center.
And, why is that important? Principally, because more and more healthcare professionals are discovering that while their training often isolates them from other healthcare professionals, the science of their disciplines is crying for integration and communication. For instance, there was a time when physicians rarely gave much attention to the dental care of their patients, unless they had the most egregious deterioration of teeth. Today, however, in a growing number of clinical situations, such as the care of diabetes, physicians are inquiring as to whether the patient is receiving routine dental care as evidence-based medicine is indicating that the control of disease and the well-being of patients with diabetes is improved by routine dental care. Also, as the science of medicine is proving that more and more heart disease may have an infectious component, or even causation, the avoidance of gingivitis and periodontal disease have become of concern to physicians as well as dentist.
The SETMA Model of Care
- The tracking by each provider on each patient of the provider’s performance on preventive care, screening care and quality standards for acute and chronic care. SETMA"s design is such that tracking occurs simultaneously with the performing of these services by the entire healthcare team, including the personal provider, nurse, clerk, management, etc.
- The auditing of performance on the same standards either of the entire practice, of each individual clinic, and of each provider on a population, or of a panel of patients. SETMA believes that this is the piece missing from most healthcare programs.
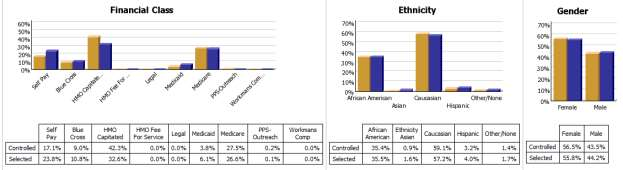
- The statistical analyzing of the above audit-performance in order to measure improvement by practice, by clinic or by provider. This includes analysis for ethnic disparities, and other discriminators such as age, gender, payer class, socio-economic groupings, education, frequency of visit, frequency of testing, etc. This allows SETMA to look for leverage points through which SETMA can improve the care we provide.
- The public reporting by provider of performance on hundreds of quality measures. This places pressure on all providers to improve, and it allows patients to know what is expected of them. The disease management tool “plans of care” and the medical-home-coordination document summarizes a patient’s state of care and encourages them to ask their provider for any preventive or screening care which has not been provided. Any such services which are not completed are clearly identified for the patient. We believe this is the best way to overcome provider and patient “treatment inertia.”
- The design of Quality Assessment and Permanence Improvement (QAPI) Initiatives - this year SETMA"s initiatives involve the elimination of all ethnic diversities of care in diabetes, hypertension and dyslipidemia. Also, we have designed a program for reducing preventable readmissions to the hospital. We have completed a Business Intelligence (BI) Report which allows us to analyze our hospital care carefully.
The SETMA Model Detailed
The SETMA Model Step I -- Provider Performance Tracking
The Physician Consortium for Performance Improvement (PCPI) is an organization created by the AMA, CMS, Institute of Medicine and others to develop measurement sets for quality assessment. The intent is to allow healthcare providers to evaluate their own performance at the time they are seeing a patient. SETMA is tracking a number of these measurement sets including: Chronic Stable Angina, Congestive Heart Failure, Diabetes, Hypertension, and Chronic Renal Disease Stages IV through ESRD, Adult Weight Management, and Care Transitions. Others will be added overtime. The details of these measurement sets and SETMA"s provider performance on each can be found under Public Reporting PCPI.
In addition to Provider Performance Tracking tools, such as those produced by PCPI, the National Quality Foundation (see Public Reporting NQF), and National Committee for Quality Assurance (see Public Reporting HEDIS and/or NCQA), SETMA has designed a pre-visit quality measures screening and preventive care tool. This allows a SETMA provider and a patient to quickly and easily assess whether or not the patient has received all of the appropriate preventive health care and the appropriate screening health care which national standards establish as being needed by this patient. The following is the Pre-visit Preventive Screening tool. All measures in black apply to the current patient and are fulfilled. All measures in red apply to the current patient and have not been fulfilled and all measures in grey do not apply to the current patient. If a point of care is missing, it can be fulfilled with the single click of a single button.
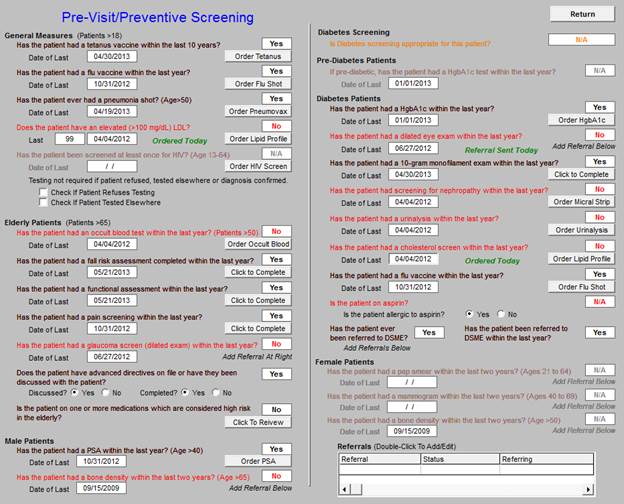
There are similar tracking tools for all of the quality metrics which SETMA providers track each day. The following is the tool for NQA measures:

The providers" compliance with these measures is color coded for quick reference. The “view” button allows the provider to quickly review the content of the metric and to review the patient’s results.
Passing the Baton
While healthcare provider performance is important for excellent care of a patient’s health, there are 8,760 hours in a year. A patient who receives an enormous amount of care in a year is in a provider’s office or under the provider’s direct care less than 60 hours a year. This makes it clear that the patient is responsible for the overwhelming amount of their own care which includes compliance with formal healthcare initiatives and with lifestyle choices which support their health.
If responsibility for a patient’s healthcare is symbolized by a baton, the healthcare provider carries the baton for .68% of the time. That is less than 1% of the time. The patient carries the baton 99.32% of the time. The coordination of the patient’s care between healthcare providers is important but the coordination of the patient’s care between the healthcare providers and the patient is imperative.
Often, it is forgotten that the member of the healthcare delivery team who carries the „baton" for the majority of the time is the patient and/or the family member who is the principal caregiver. If the „baton" is not effectively transferred to the patient or caregiver, then the patient’s care will suffer.

Firmly in the providers hand
--The baton - the care and treatment plan
Must be confidently and securely grasped by the patient, If change is to make a difference
8,760 hours a year.
The poster illustrates:
- That the healthcare-team relationship, which exists between the patient and the healthcare provider, is key to the success of the outcome of quality healthcare.
- That the plan of care and treatment plan, the “baton,” is the engine through which the knowledge and power of the healthcare team is transmitted and sustained.
- That the means of transfer of the “baton” which has been developed by the healthcare team is a coordinated effort between the provider and the patient.
- That typically the healthcare provider knows and understands the patient’s healthcare plan of care and the treatment plan, but that without its transfer to the patient, the provider’s knowledge is useless to the patient.
- That the imperative for the plan - the “baton” - is that it be transferred from the provider to the patient, if change in the life of the patient is going to make a difference in the patient’s health.
- That this transfer requires that the patient “grasps” the “baton,” i.e., that the patient accepts, receives, understands and comprehends the plan, and that the patient is equipped and empowered to carry out the plan successfully.
- That the patient knows that of the 8,760 hours in the year, he/she will be responsible for “carrying the baton,” longer and better than any other member of the healthcare team.
The genius and the promise of the Patient-Centered Medical Home are symbolized by the “baton.” Its display will continually remind the provider and will inform the patient, that to be successful, the patient’s care must be coordinated, which must result in coordinated care. In 2011, as we expand the scope of SETMA"s Department of Care Coordination, we know that coordination begins at the points of “transitions of care,” and that the work of the healthcare team - patient and provider - is that together they evaluate, define and execute that care.
The SETMA Model - Step 2 -- Auditing of Provider Performance - SETMA’s COGNOS Project
The creating of quality measures is a complex process. That is why it is important for agencies such as the Ambulatory Care Quality Alliance (AQA), the NCQA, the NQF, the Physician Quality Reporting System (PQRS) and PCPI, among others, to identify, endorse and publish quality metrics. The provider’s ability to monitor their own performance and the making of those monitoring results available to the patient is important, but it only allows the provider to know how they have performed on one patient. However, the aggregation of provider performance over his/her entire panel of patients, through an auditing tool, carries the process of designing the future of healthcare delivery a further and a critical step. The problem with most auditing results, such as HEDIS, is that it is presented to the provider 12 to 18 months after the fact. SETMA believes that “real time” immediate auditing and giving of the audit results to providers can change provider behavior and can overcome “treatment inertia.”
Auditing of provider performance allows physicians and nurse practitioners to know how they are doing in the care of all of their patients. It allows them to know how they are doing in relationship to their colleagues in their clinic or organization, and also how they are performing in relationship to similar practices and providers around the country.
As a result, SETMA has designed auditing tools through the adaptation to healthcare of IBM"s business intelligence software, COGNOS. Multiple articles on SETMA"s COGNOS Project can be found under Your Life Your Health and the icon COGNOS. Those discussions will not be repeated here but auditing is an indispensable tool for the improvement of the quality of healthcare performance and for improvement in the design of healthcare delivery.
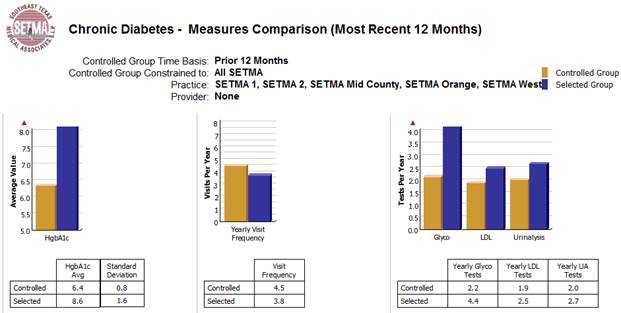
The following are a few examples of the auditing SETMA does of provider performance.

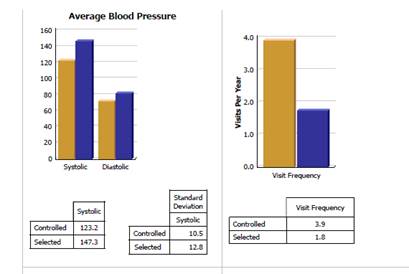
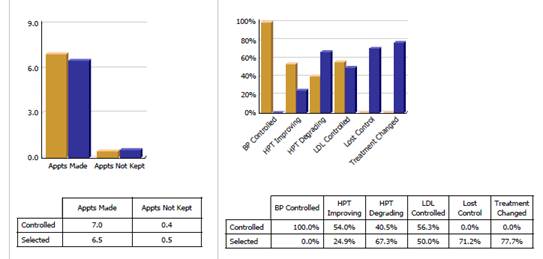
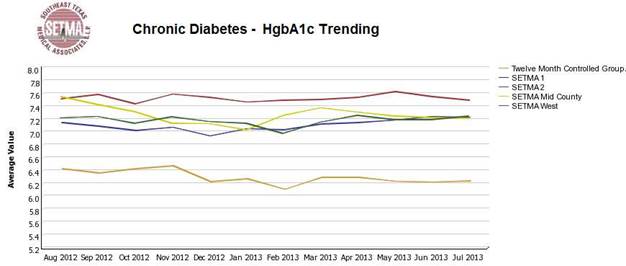
Through BI, SETMA is able to display outcomes trending which can show seasonal patterns of care and trending comparing one provider with another. It is also possible to look at differences between the care of patients who are treated to goal and those who are not. Patients can be compared as to socio-economic characteristics, ethnicity, frequency of evaluation by visits and by laboratory analysis, numbers of medication, payer class, cultural, financial and other barriers to care, gender and other differences. This analysis can suggest ways in which to modify care in order to get all patients to goal.
Using digital dashboard technology, SETMA analysis provider and practice performance in order to find patterns which can result in improved outcomes practice wide for an entire population of patients. We analyze patient populations by:
- Provider Panel
- Practice Panel
- Financial Class - payer
- Ethic Group
- Socio-economic groups
We are able to analyze if there are patterns to explain why one population or one patient is not to goal and others are. WE can look at:
- Frequency of visits
- Frequency of testing
- Number of medications
- Change in treatment
- Education or not
- Many other metrics
We are able to present over-time patient results comparing:
- Provider to practice
- Provider to provider
- Provider current to provider over time
- Trending of results to see seasonal changes, etc.
The SETMA Model - Step 3 -- Analysis of Provider Performance through Statistics
Raw data can be misleading. It can cause you to think you are doing a good job when in fact many of your patients are not receiving optimal care. For instance the tracking of your average performance in the treatment of diabetes may obscure the fact that a large percentage of your patients are not getting the care they need. Provider Performance at the point of service is important for the individual patient. Provider Performance over an entire population of patients is important also. However, until you analyze your performance data statistically, a provider will not know how well he or she is doing or how to change to improve the care they are providing.
Each of the statistical measurements which SETMA tracks, the mean, the median, the mode and the standard deviation, tells us something about our performance. And, each measurement helps us design quality improvement initiatives for the future. Of particular, and often, of little known importance is the standard deviation.
From 2000 to 2013, SETMA has shown annual improvement in the mean (the average) and the median results for the treatment of diabetes. There has never been a year when we did not improve. Yet, our standard deviations revealed that there were still significant numbers of our patients who are not being treated successfully. Even here, however, we have improved. From
2008 to 2013, SETMA experienced a 9.3% improvement in standard deviation. Some individual SETMA providers had an improvement of over 16% in their standard deviations. Our goal for 2010 is to have another annualized improvement in mean and in median, and also
to improve our standard deviation. When our standard deviations are below 1 and as they approach .5, we can be increasingly confident that all of our patients with diabetes are being treated well.
An example of a statistical analysis of SETMA"s diabetes care in regard to the elimination of ethnic disparities of care is given in the article Eliminating Ethnic Disparities in Diabetes Care Your Life Your Life Your Health The Examiner May 13, 2010.
The SETMA Model - Step 4 -- Public Reporting of Provider Performance
One of the most insidious problems in healthcare delivery is reported in the medical literature as “treatment inertia.” This is caused by the natural inclination of human beings to resist change. Often, when patients" care is not to goal, no change in treatment is made. As a result, one of the auditing elements in SETMA"s COGNOS Project is the assessment of whether a treatment change was made when a patient was not treated to goal. Overcoming “treatment inertia” requires the creating of an increased level of discomfort in the healthcare provider and in the patient so that both are more inclined to change their performance. SETMA believes that one of the ways to do this is the pubic reporting of provider performance. That is why we are publishing provider performance by provider name under Public Reporting.
The following is a report which appears on our website for 2009-2013 through September 30, 2013 in the NCQA Diabetes Recognition audit. All SETMA providers have earned NCQA recognition.
A more complete explanation of SETMA"s philosophy and intent in “public reporting” of Provider’s performance can be found in the following articles:
The SETMA Model - Step 5 -- QAPI - Quality Assessment and Performance Improvement
Quality Improvement Initiatives based on tracking, auditing, statistical analysis and public reporting of provider performance are critical to the transformation of healthcare both as to quality of care and as to cost of care.
With the above described data in hand and with the analysis of that data, it is possible to design quality initiatives for future improvement in care. Currently SETMA is designing two major quality initiatives. One is for diabetes. It is an attempt to eliminate the last vestiges of ethnic disparity in the care of diabetes. This will require the use of additional internal resources and attention but it is our intent to do so and to permanently and totally eliminate ethnic disparities. The other is in regard to decreasing avoidable readmissions to the hospital.
The details of these two initiatives can be reviewed here:
Without a systems approach to healthcare, each of these steps are impossible; certainly, the analysis and transformation of healthcare is impossible. With a systems approach, this logical and sequential process is possible and rewarding for provider and patient. This process has also set SETMA on a course for successful and excellent healthcare delivery. Our tracking, auditing, analysis, reporting and design will keep us on that course.
SETMA"s Model of Care has and is transforming our delivery of healthcare, allowing us to provide cost-effective, excellent care with high patient satisfaction. This Model of Care is evolving and will certainly change over the years as will the quality metrics which are at its core.
SETMA’s Model as a tool for Patient-Centered Medical Home
In February, 2009, SETMA undertook to use our Model of Care to become a medical home. In April 2010, we applied and in July, we were awarded Tier Three Medical Home recognition by NCQA and in 2013, we were again awarded the NCQA Tier III Medical Home recognition. In August, 2010 we were award Medical Home and Ambulatory Care accreditation by AAAHC and received the same for 2011-2014. This process is one of the most difficult things we have done. I use the word “is” because I believe that all of us who already have medical home “recognition” or “accreditation” or both are still in the process of transforming the practice of medicine by the principles, ideals and goals of medical home. The formal process took SETMA from February 16, 2009 to the date we first submitted our NCQA application on April 12, 2010. The process did not end there.
The transition was and is a true “transformation,” rather than a “reformation.” In function, the distinction between these two concepts as applied to healthcare is that “reformation” comes from pressure from the outside, while “transformation” comes from “an essential change of motivation and dynamic from the inside.” Anything can be reformed - reshaped, made to conform to an external dimension - if enough pressure is brought to bear. Unfortunately, reshaping under pressure can fracture the object being confined to a new space. And, it can do so in such a way as to permanently alter the structural integrity of that which is being reformed. Also, once the external pressure is eliminated, redirected or lessened, the object often returns to its previous shape as nothing has fundamentally changed in its nature.
Being from within, transformation results in change which is not simply reflected in shape, structure, dimension or appearance, but transformation results in a change which is part of the nature of the organization being transformed. The process itself creates a dynamic which is generative, i.e., it not only changes that which is being transformed but it creates within the object of transformation the energy, the will and the necessity of continued and constant change and improvement. Transformation is not dependent upon external pressure but is sustained by an internal drive which is energized by the evolving nature of the organization.
While this may initially appear to be excessively abstract and unwieldy, it really begins to address the methods or tools needed for reformation or for transformation. They are significantly different. The tools of reformation, particularly in healthcare administration are rules, regulations, and restrictions. Reformation is focused upon establishing limits and boundaries rather than realizing possibilities. There is nothing generative - creative - about reformation. In fact, reformation has a “lethal gene” within its structure. That gene is the natural order of an organization, industry or system"s ability and will to resist, circumvent and overcome the tools of reformation, requiring new tools, new rules, new regulations and new restrictions. This becomes a vicious cycle. While the nature of the system actually does change, where the goal was reformation, it is most often a dysfunctional change which does not produce the desired results and often makes things worse.
The tools of transformation may actually begin with the same ideals and goals as reformation, but now rather than attempting to impose the changes necessary to achieve those ideals and goals, a transformative process initiates behavioral changes which become self-sustaining, not because of rules, regulations and restrictions but because the images of the desired changes are internalized by the organization which then finds creative and novel ways of achieving those changes.
It is possible for an organization to meet rules, regulations and restrictions perfunctorily without ever experiencing the transformative power which was hoped for by those who fashioned the external pressure for change. In terms of healthcare administration, policy makers can begin reforms by restricting reimbursement for units of work, i.e., they can pay less for office visits or for procedures. While this would hopefully decrease the total cost of care, it would only do so per unit. As more people are added to the public guaranteed healthcare system, the increase in units of care will quickly outstrip any savings from the reduction of the cost of each unit. Historically, this has proved to be the case. When Medicare was instituted in 1965, projections were made about the increase in cost. In 1995, it was determined that the actual utilization was 1000% more than the projections. No one had anticipated the appetite for care and the consequent costs which would be created by a system which made access to care universal for those over 65 and which eliminated most financial barriers to the accessing of that care.
Reformation of healthcare promises to decrease the cost of care by improving preventive care, lifestyles and quality of care. This ignores the initial cost of preventive care which has a payoff almost a generation later. It ignores the fact that people still have the right, which they often exercise, to adopt unhealthy lifestyles. Even the President of the United States continues to smoke.
The currently proposed reformation of the healthcare system does nothing to address the fact that the structure of our healthcare system is built upon a “patient” coming to a healthcare provider who is expected to do something “for” the patient. The expectation by the system and by the recipient of care is that something is going to be done “to” or “for” the patient in which process the patient is passive. There is little personal responsibility on the part of the patient for their own healthcare, whether as to content, cost or appropriateness. The healthcare provider is responsible for the health of the patient.
Transformation of healthcare would result in a radical change in relationship between patient and provider. The patient would no longer be a passive recipient of care given by the healthcare system. The patient and provider would become an active team where the provider would cease to be a constable attempting to impose health upon an unwilling or unwitting patient. The collaboration between the patient and the provider would be based on the rational accessing of care. There would no longer be a CAT scan done every time the patient has a headache. There would be a history and physical examination and an appropriate accessing of imaging studies based on need and not desire.
This transformation will require a great deal more communication between patient and provider which would not only take place face-to-face, but by electronic or written means. There was a time when healthcare providers looked askance at patients who wrote down their symptoms. The medical literature called this "la maladie du petit papier" or “the malady of the small piece of paper.” Patients who came to the office with their symptoms written on a small piece of paper where thought to be neurotic. No longer is that the case. Providers can read faster than a patient can talk and a well thought out description of symptoms and history is an extremely valuable starting point for accurately recording a patient’s history. Many practices with electronic patient records are making it possible for a patient to record their chief complaint, history of present illness and review of systems, before they arrive for an office visit. This increases both the efficiency and the excellence of the medical record and is part of a transformation process in healthcare delivery.
This transformation will require patients becoming much more knowledgeable about their condition than ever before. It will be the fulfillment of Dr. Joslin’s dictum, “The person with diabetes who knows the most will live the longest.” It will require educational tools being made available to the patient in order for them to do self-study. Patients are already undertaking this responsibility as the most common use of the internet is the looking up of health information. It will require a transformative change by providers who will welcome input by the patient to their care rather seeing such input as obstructive.
This transformation will require the patient and the provider to rethink their common prejudice that technology - tests, procedures, and studies - are superior methods of maintaining health and avoiding illness than communication, vigilance and “watchful waiting.” Both provider and patient must be committed to evidence-based medicine which has a proven scientific basis for medical-decision making. This transformation will require a community of patients and providers who are committed to science. This will eliminate “provider shopping” by patients who did not get what they want from one provider so they go to another.
This transformation will require the reestablishment of the trust which once existed between provider and patient to be regained. That cannot be done by fiat. It can only be done by the transformation of healthcare into systems which we had fifty to seventy-five years ago. The patient must be absolutely confident that they are the center of care but also they must know that they are principally responsible for their own health. The provider must be an extension of the family. This is the ultimate genius behind the concept of Medical Home and it cannot be achieved by regulations, restrictions and rules.
The transformation will require patient and provider losing their fear of death and surrendering their unspoken idea that death is the ultimate failure of healthcare. Death is a part of life and, in that, it cannot forever be postponed, it must not be seen as the ultimate negative outcome of healthcare delivery. While the foundation of healthcare is that we will do no harm, recognizing the limitations of our abilities and the inevitability of death can lead us to more rational end-of- life healthcare choices.
As SETMA works with transformation and medical home, we have also finalized our affiliate relationship with Diabetes Center of Excellence which is affiliated with Harvard Medical School. In this process, I have been taken with a paragraph from the essay, Elliott P. Joslin, MD: A Centennial Portrait (Joslin Diabetes Center, 1998, p. 45), which states:
“Joslin and later his associates developed an elaborate dictation system that extended greatly beyond the polite written communication tradition expected from the Boston or urban gentleman physician of the Edwardian era. For example, each patient received a ‘report’ dictated the same day as their office appointment. These letters not only provided the patient with the laboratory figures and the essential facts of the physical exam, but more often than not included a whole range of advice that might even involve bargaining with the patients about health matters.”
The core elements of Patient-Centered Medical Home are contained in this simple paragraph:
- Providing the patient with a written plan of care and a treatment plan.
- Reporting test results to the patient in a timely fashion.
- Collaborating with the patient about their care, not only empowering and enabling patients to carry out the treatment plan and plan of care but also having the patient embrace the plan.
- And, it illustrates the essence of Patient-Centered Medical Home which is, “Thinking about the patient when he/she is not in your presence.”
It has long been my assertion that Patient-Centered Medical Home has as its goal a return to the healthcare structure of the 1940s and 50s with the benefits and capabilities of the technological advances of the 21st Century. This paragraph lets me know we must go back further than the 40s and 50s.
Dr. Joslin’s work and treatment of patients with diabetes illustrates the best of care of his day and it also illustrates the structure and methods of the future of care. Remember, from Dr. Joslin’s writing of his first paper on diabetes while a medical student in 1893, it was 100 years (1993) before the Diabetes Control and Complications Trial (DCCT) was published, which confirmed Dr. Joslin ideas about glucose control and patient education in the treatment of diabetes. As seen here, it was not only Dr. Joslin’s treatment of diabetes which was prescient but his organization and methods of his practice were also.
How is the patient’s experience different today under this model?
One of the pressing issues in relationship to any changing process is the answer to the question, “If I make a change, will it make a difference?” This is really the distinction between “coordination of care” - this is the process by which we design and execute changes and it is the responsibility of the healthcare team - and “coordinated care” - this is the result and it is measured by the patient’s “perception” of their experience
The former is the easy part; the latter is the difficult part. In process the patient experience has dramatically changed:
- The patient’s care is evaluated on the basis of over 300 quality metrics which represent multiple “clusters” of quality metrics and in any given patient visit will represent the evaluation of multiple clusters, or a galaxy of clusters, for any single patient.
- The patient receives a summary of these “clusters” and galaxies” with a recommendation to contact his/her healthcare provider to request that any metrics not completed be done.
- “Care transition” points are attended to and a “plan of care” and “treatment plan” baton is handed off to the patient so that they can participate effectively as a member and as the head of their healthcare team.
- Because of SETMA"s Department of Care Coordination, ever patient who leaves the hospital receives a follow-up call the day after discharge. This is not a fifteen second “administrative call” to fulfill a metric, but it is a twelve to thirty minute call which has substance and is an active part of the care of the patient. Selected patients seen in the clinic receive follow-up calls at any interval determined by the healthcare provider related to vulnerabilities, uncertainties or complexities of their care.
- The Joslin Diabetes Clinic Affiliate at Southeast Texas Medical Associates is built on a medical home platform. Seven Stations of Success in the care of patients with diabetes guides the patient through their clinic experience and prepares them to lead their team. Station one and station seven address the dynamic of medical home in the experience of our patients: Station one - there are 8,760 hours in the year. The patient is the leader of his/her healthcare team for all 8,760 hours.
The last thing the patient sees as he/she leaves the clinic is Station Seven for Success which is placed on the back of the entrance/exit door to the clinic. It details the “health home principles and states:
- The patient’s cerebrovascular and cardiovascular risk is assessed at every visit rather than every five years as recommended by the AAFP. In addition, both during the visit and in the “plan of care" and “treatment plan,” a section is included which is entitled “WHAT IF?” Consistent with the question, “If I make a change, will it make a difference?,” this section shows the patient how his/her risk will change if a number of individual elements or a combination of multiple elements used to calculate the risk is changed.
- Four years ago, the SETMA partners founded The SETMA Foundation. In the past fifteen months, the SETMA partners have given $1,000,000 to the foundation and we just received our first non-SETMA contribution of $150,000. This money is used to pay for the care of our patients who cannot afford it. None of the money can profit SETMA.
At the foundation of quality healthcare, there is an emotional bond - a trust bond -between the healthcare provider and the patient. It is possible to fulfill all quality metrics without this bond; it is not possible to provide quality healthcare without it. That is why the patient-centered medical home (PC-MH), coupled with the fulfilling of quality metrics is the solution to the need for quality healthcare.
The genius of PC-MH is to discover the true implications of SETMA’s motto which was adopted in August, 1995, which is, “Healthcare: Where Your Health is the Only Care” It is to put the patient and their needs first. And, it is to include the patient as a member of the healthcare team. There are 8,760 hours in a year. If responsibility for a patient’s healthcare is seen as a baton then patient carries that “baton” for over 8,700 hours a year. PC-MH promotes methods for effectively “passing the baton” to the patient so that the patient’s healthcare does not suffer under the patient’s own supervision. SETMA has placed the patient’s healthcare at the center of our healthcare delivery in many ways. One way is that we developed The SETMA Foundation, through which we help provide funding for the care of our patients who cannot afford it. Our resources are meager in comparison with the need, but it is a start.
The following is one example of how PC-MH and the SETMA Foundation have worked together to produce quality healthcare. A patient came to the clinic angry, hostile and bitter and was found not to be a bad person but to be depressed because he could not work, could not afford his medication and was losing his eye sight. He left the clinic with The Foundation paying for his medications, giving him a gas card to get to our ADA certified DSME program, waiving the fees for the classes, helping him apply for disability, and getting him an appointment to an experimental program for preserving his eyesight. He returned in six weeks with something we could not prescribe. He had hope and joy. By the way, his diabetes was treated to goal for the first time in years. This is PC-MH; it is caring and it is humanitarianism. .
As the Patient-Centered Medical Home is restoring the personal aspect of healthcare, the Medicare Advantage (MA) program and/or the Accountability of Care Organizations (ACO) are modifying the „piece" payment system of healthcare. While the President has been convinced that Medicare Advantage is the problem; it is the solution. The supposed increase in the cost of Medicare Advantage is because it is being compared to traditional Medicare costs where the administrative cost of Medicare is not calculated in the formulae. There are bright examples of success with Medicare Advantage, success marked by quality outcomes and high patient satisfaction. That success also is marked by a dramatic change in the trajectory of health care cost while maintaining its quality.
The third piece to true healthcare transformation is including quality process and quality outcomes in the payment formula. There are fledgling programs such as the Physician Quality Reporting System (PQRS) where healthcare providers are being paid for the demonstration of quality outcomes rather than just for piece work. The accountability of the pubic reporting of provider performance on quality measures completes this picture. This is why SETMA has begun quarterly reporting on our website of our providers’ performance on multiple quality metrics. Included in that reporting is the examination of whether disparities of care in ethnic and socio-economic groups have been eliminated.
Quality healthcare is a complex problem. Measurable processes and outcomes are only one part of that complexity. Communication, collaboration and collegiality between healthcare provider and patient, between healthcare provider and healthcare provider, between healthcare providers and other healthcare organizations are important aspects of that complexity also. Data and information sharing within the constraints of confidentiality add another layer of complexity. All of these aspects of healthcare quality can be addressed by technology but only when that technology is balanced by humanitarianism.
|