|
James (Larry) Holly, M.D.
CEO, Southeast Texas Medical Associates (SETMA)
www.jameslhollymd.com
Adjunct Professor
Family & Community Medicine
University of Texas Health Science Center
San Antonio School of Medicine
Clinical Associate Professor
Department of Internal Medicine
School of Medicine
Texas A&M Health Science Center
December 5, 2013
Dear Ms. Tavenner and Dr. Reider:
This correspondence is an appeal from Southeast Texas Medical Associates, LLP (SETMA, www.jameslhollymd.com) in Beaumont, Texas, in regard to Meaningful Use 2 (MU2). It is founded upon SETMA’s vision for transformation of healthcare, which is the path for dynamic and sustainable change. Internalized values, a personal and collective vision and a generative passion for excellence in healthcare delivery are the fuel and energy for transformation in medicine. Reform is dependent upon external pressure, based on rules and regulations to sustain and guide change. Reform requires financial reward and/or threat of financial penalties to drive the process, while transformation is driven by a creative tension between one’s vision and one’s current reality. CMS and ONC will want to take care that attempts to improve care with reform does not adversely effect dramatic improvements through transformation.
Not being inherently creative, reform is dependent upon uniformity with all participants being required essentially to look alike; transformation will result in sustained, creative innovation, which will by its nature result in diversity. Transformation will be trail blazing with rapid innovation producing advances in healthcare improvement. Sometimes, reform will stifle creativity and transformation. To avoid this potential negative impact of well-intentioned reform, thoughtful leaders will recognize the need for innovative leaders and organizations to receive temporary exemptions from the rules and regulations which are the tools of reform. (For more on the dichotomy between reform and transformation see Healthcare Policy Issues Part III - Reforming or Transforming Healthcare.
SETMA shares CMS’ and ONC’s desire for improving the patient’s experience of care, for improving the outcomes of care, and for making those changes sustainable. We also believe in transforming healthcare through the creative use of technology and innovation. We recognize that one of the frustrations with transformation by public policy leaders is that it is, by necessity, more difficult to control and to measure. While our appeal has a broader intent than to address SETMA’s circumstances in regard to MU2, it is based on who we are, from where we have come and where we wish to go.
In this discussion, we will address:
- The different, but complementary, benefits of interoperability and Health Information Exchanges.
- The potential conflict and complexity in bringing inappropriate data and/or data generated in another setting from one EHR into another.
- The definition of MU2 of success for CMS, ONC, and healthcare providers.
- A solution for providers succeeding with MU2.
- The Automated Team, the logical extension and end-point of clinical decision support.
- The possibility and potential value of exemptions, usually temporary, to rules and regulations.
- What is the ultimate goal of electronic health records (EHR)?
- Are there other values in EHR superior to interoperability?
- Is absolute uniformity in EHR use among providers an essential good?
It is not expected that you will examine each of the links included in this letter, but they are included and annotated to give substance to our appeal. This appeal is in the context of my question to Dr. David Blumenthal when he was still the ONC Director. In a small group meeting at a HIMSS meeting, I asked him, “Have you ever considered the potential that Meaningful Use may have the pernicious effect of delaying the adoption of EHR?” His response was, “We have thought about that.” The context of my question was not opposition to Meaningful Use but my hope that it would effectively accelerate EHR adoption and advancement.
SETMA’s Health Policy and Philosophy
- As defined by Don Berwick, we believe that healthcare is a human right.
- We embrace the “moral test for government” as defined by Hubert Humphrey in 1977.
- The SETMA Foundation was formed in 2009. Annually, SETMA’s partners give $500,000 to the Foundation. These funds are used to pay for the care of patients who cannot afford care and also for support for health education for students who need assistance. These funds cannot profit or benefit SETMA.
- In 2003, we initiated a zero-co-pay for our Medicare Advantage (MA) patients to remove all financial barriers to care. We have actually demonstrated a significant difference in results between a zero-co-pay MA population and fee-for-service Medicare beneficiaries which we attribute to a barrier created by the cost of care for the FFS Medicare beneficiaries.
- We have eliminated ethnic disparities in diabetes and hypertension care. (See AHRQ - Diabetes Ethnic Disparities AHRQ letter about ethnic disparities by James L Holly, MD)
- To validate our commitment to excellence and transformation in healthcare, we have published our opinions on public health policy at Your Life Your Health - Healthcare-Reform-Public-Policy.
- In 2009, we began publishing SETMA provider performance by provider name on over 300 quality metrics at Public Reporting - Reporting by Type.
- We provide care for many uninsured and indigent patients and in March, 2014, will assume responsibility for caring for ALL indigent and uninsured patients who come to our largest hospital. This is a practical expression of items 1 and 2 above.
- Most of our providers hold adjunct or clinical academic appointments at Texas Schools of Medicine.
Who is SETMA?
- Formed in 1995 with four physicians, SETMA today is a 40-provider, multispecialty group.
- In 1996, SETMA actively participated in capitated managed care environment which grew into MA and an Accountable Care Organization.
- In March 1998, SETMA adopted EHR.
- In May 1999, SETMA’s goal morphed into the pursuit of electronic patient management (EPM).
- In May 1999, SETMA defined ten principles on the basis of which we would design our EHR, which were (see Designing an EMR on the Basis of Peter Senge's The Fifth Disciple by James L. Holly, M.D.):
- Pursue EPM rather than EHR, leveraging the power of electronics to improve individual and population health.
- Bring to bear upon every patient encounter that which is known rather than what an individual provider knows.
- Make it easier to do it right than not do it at all.
- Continually challenge providers to improve their performance.
- Easily infuse new knowledge and decision-making tools throughout an organization.
- Establish and promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement (PCPI) Data Sets.
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
- These principles led to making SETMA’s use of the EHR meaningful in pursuit of the Institute of Healthcare Improvement’s (IHI) Triple Aim. (see NextGen As A Tool For Redesigning Primary Care To Fulfill IHI’s Triple Aim)
- In 2000, we began using clinical-decision-support tools developed in-house, chronic disease management tools and analytics to improve populations health, initially for diabetes and then for other conditions. (See item 14 below)
- Our results have shown continuous improvement in mean and standard deviations and outcome measures since 2000 for diabetes. (see The Importance of Data Analytics in Physician Practice).
- In 2002, made a presentation to Joslin Diabetes Center affiliated with Harvard University, which initiated a relationship which resulted in 2010 with SETMA becoming the first multi-specialty group to be a formal Joslin Diabetes affiliate.
- In 2005, SETMA received the HIMSS Davies Award.
- In 2009, SETMA started the process to become a PC-MH. (Your Life Your Health - Medical-Home). We have received the following accreditations:
- In 2011, SETMA’s peer-reviewed Stories of Success was published by HIMSS as a Meaningful Use Case Study – Southeast Texas Medical Associates (SETMA) – 2011 Stories of Success Case Study Selection (http://www.himss.org/ResourceLibrary/ResourceDetail.aspx?ItemNumber=11398)
- In 2010, AHRQ published SETMA’s LESS Imitative (Lose weight, exercise, stop smoking) on its Innovation Exchange. (see Multispecialty Practice Uses Electronic Templates to Provide Customized Support at Every Visit, Contributing to Improved Patient Behaviors and Outcomes | AHRQ Innovations Exchange, https://innovations.ahrq.gov/profiles/multispecialty-practice-uses-electronic-templates-provide-customized-support-every-visit)
- In February 2011, SETMA was named one of Thirty Exemplary Practices for Clinical Decision Support by the U. S. Office of the ONC for HIT (February, 2011) -- "Advancing Clinical Decision Support" an intensive, multi-part project funded by the U.S. Office of the National Coordinator for Health Information Technology (ONC) to address the major barriers to achieving widespread use of clinical decision support.
- In 2012, SETMA’s CEO was named the HIMSS Physician IT Leadership Award recipient
- In 2012, the Robert Wood Johnson Foundation, selected SETMA as One of the top 30 Exemplar Ambulatory Practices SETMA Selected One of the top 30 Exemplar Ambulatory Practices
SETMA’s MU2 Dilemma
SETMA’s MU2 dilemma stems from the fact that when we began using the EHR in 1999, our vendor did not have a data base which could be used. It further results from SETMA’s adopting the ideal of EPM in May, 1999, which set us on a rapid course of healthcare transformation in which we outpaced other organizations and certainly outpaced our vendor in healthcare transformation. Now, we find ourselves in the position of using the EHR meaningfully as a transformative tool, but not being able to fulfill the requirements of healthcare reforms, which require uniformity in functionality. We either have to suspend transformation of our healthcare delivery in order to conform to the rules and regulations demanded by healthcare reform, or suffer penalties now and in the future, which penalties are likely to become more onerous in the next ten years.
After reading the MU Use Workshop Stage 3 Update (Paul Tang, Chair, Health IT Policy Committee), and seeing that almost all of the proposed elements are issues with which we have dealt with in our PC-MH, I was encouraged that if we can resolve the problems with MU2, SETMA can continue on our 19-year journey to healthcare transformation. SETMA is not only fulfilling the structural necessities of PC-MH; we have also achieved the functional and dynamic elements of PC-MH. The ONC’s MU3 is probably going to require additional interoperability functions which will be a barrier to SETMA receiving recognition for the PC-MH work we are already doing.
In this context, I offer the following observations on SETMA and MU2. On November 26, 2013, it was confirmed to SETMA that even though our EHR vendor is one of only twenty-one vendors which have met certification for MU2, because our use of that vendor’s platform is customized, we cannot use that certification to attest to SETMA’s meeting of MU2 standards. Published reviews have suggested that the practices which are going to be “hurt” the most by MU2 are the early adapters like SETMA. Remember, in March 1998, when we bought our vendor’s product, they had no knowledge base, so out of necessity we had to build our own. This is the foundation of SETMA’s request for an exemption for four years. That exemption will give us time to continue our transformation and to make the changes to our EHR which will allow us to meet MU2 and 3.
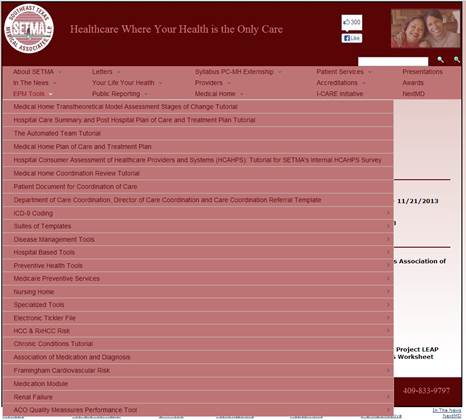
In 1999, SETMA’s vision of EHR changed from simply being a tool for documenting a patient encounter, to being a tool for leveraging the power of electronics to improve care for individuals and to improve care of panels or populations. Through all of this, SETMA rapidly and continually improved and expanded our tools for transforming care. All of those tools can be reviewed at Electronic Patient Management Tools (EPM stands for “electronic patient management”). These tools are made available to everyone and anyone without cost and even though these tools have great value, they are not copyrighted. Their purpose is to improve healthcare for anyone who wishes to use them.
“EPM Tools” Section of SETMA’s Website
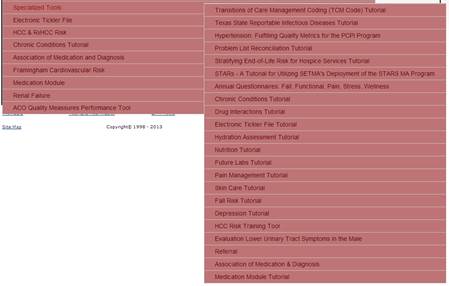
Additional “Specialized Tools” Section of SETMA’s Website
SETMA’s major obstacle posed by MU2 is interoperability. SETMA is not unaware of the value of shared data. We utilize our EHR everywhere we see patients:
- In the hospital (4 different hospitals using the same EHR database)
- In the emergency department (three different ED using the same EHR database)
- In the clinic (six different clinics using the same EHR database)
- In the nursing home (32 nursing homes using the same EHR database)
Every patient encounter, every patient activation and engagement document, every patient plan of care and treatment plan, on every patient we treat is completed in the same EHR and is simultaneous available at every point of care. Within the next six months, a practice seventy miles away will joint SETMA and other clinics, hospitals, emergency department and nursing homes will be added, with the same connectivity and shared data.
Our sub-regional Health Information Exchange expands the reach of our patient-care information to many other providers and institutions. Our Patient Web Portal makes our patients’ health information available to them. HIE is the foundation for allowing interoperability between healthcare providers and systems to exchange information about patient care. Even in their most basic form, HIEs allow for the transmission of useful data such as images and scanned reports. Even though these types of non-standardized materials may require the eye of a human for interpretation, they still provide highly useful information that can be used to improve patient care.
However, the further extension of an HIE is to use it to transmit information in a structured, standardized and codified format. Then, not only is the viewable information of the transmission useful to a healthcare provider, but it is then also coded in a format that a computer can understand and process. This then allows the power of electronics to also become part of the patient’s care. That said structured, standardized and codified documents are great enhancement to interoperability but not necessarily a requirement.
SETMA totally agrees with the goals of interoperability. However, in order not to disrupt our progress, we need a temporary exemption from MU2. The criteria for granting this exemption for SETMA and for others are discussed below. We believe that if an organization meets the criteria discussed, a four-year exemption would eliminate the disruption cause by the current deadlines and would allow the financial impact to be absorbed over a longer period of time.
Because a well designed and deployed HIE provides most of the functions of interoperability, we think our use of HIE diminishes the encumbrance our request for an exemption to MU2 has upon CMS’s and ONC’s goals. We also think that some of the exuberance for inoperability is misguided. That judgment is guided by our experience. In 1998, SETMA was prepared electronically to import a great deal of information into our newly launched EHR.
Before beginning the use of EHR to document patient encounters on Tuesday, January 26, 1999, SETMA used dictation and transcription for charting patient encounters. Therefore, in January, 1999, we had three years and six months of transcribed records. We employed a company to build an interface between Microsoft Word and our EHR vendor, so that we could place the word documents into the EHR. We thought it would give more credibility to our new tool to have 42 months of notes in the record.
The day we were prepared to “dump” the Word documents into the EHR, we stopped and asked ourselves, “When is the last time, we looked at a patient encounter note from six months or two years before in order to treat a patient?” We certainly looked at procedure results, at laboratory results and other historical data, but never at chief complaints, history of present illness, a review of systems, or a physical examination. Therefore, we made the decision, which turned out to be wise, to keep the word document file and the paper chart record according to statutory requirements, and to start the EHR record from the beginning. We extracted important diagnostic materials, allergies, medications, family, social and personal history, etc, but we did not extract the details associated with a single encounter.
Now we come to 2013 and 2014, and we find that even though SETMA has advanced the cause of electronic records and of healthcare transformation, and even though we have been awarded and recognized for excellence in every aspect of the use of EHR, we are going to be excluded from participating in a significant and important CMS and ONC initiative because we started the use of EHR too early and because we helped lead the transformation from EHR to EPM..
My purpose in writing is to offer a reasonable and appropriate solution to our dilemma and that of many other meaningful users of the EHR. That solution is:
- For CMS and ONC to recognize that the interoperability which MU2 requires is not based on excellent care but on an artificial standard. The elements of a patient encounter which have value to another provider are diagnoses, allergies, medications, past medical and surgical history, habits, demographics, and some laboratory values. This is not an exhaustive list.
- Interoperability and Health Information Exchanges have different but complementary functions. Other elements of the record than those mentioned in 1 above, i.e., chief complaint, review of systems, history of present illness and physical examination are more appropriately communicated as a document through a Health Information Exchange.
Placing these elements in structured fields presents a potential conflict as the receiving provider may find those elements in error and would have a difficult task distinguishing between the evaluation by the former provider and their own evaluation. Time would be required to document why contradictory history and physical data is in the same record. This also potentially creates a medico-legal problem if the data from anther source is not clearly documented and then is not specifically contradicted by the receiving provider.
In addition to asking HHS, CMS, HIT and ONC to rethink these issues, we have the following concerns:
- In a recent interview, Ms. Jodi Daniel, commented that ONC is determined to succeed with Meaningful Use. Here we have to define “success.” I have no financial interest in any EHR. My concern about the unintended consequences of MU2 in reducing the number of EHRs from 500+ to 21, or so, is that it unfairly punishes the healthcare providers who unwittingly purchased an EHR which is inadequate. Success, rather than driving them out of business, would seem to require giving them time to make the changes necessary to meet MU2 standards, and if they attest to the fact that they are taking the necessary steps to meet the valid interoperability steps, for CMS to delay penalties for two years, i.e., to January, 2016.
This does not compromise ONC’s mission but it does make “success” bi-directional, i.e., not only the fulfillment of ONC’s goals, but giving providers time to change. It would be difficult for me to ascribe “success” to a program which is going to punish physicians for having bought an EHR. Success would seem to dictate ONC facilitating providers who are willing to change. It is also reasonable to give vendors who are committed to meeting MU2 standards time to make the necessary changes. It is hard for me to imagine that CMS and ONC would judge themselves to be successful if that success resulted in the dissemination of an industry which was created by the attempt to meet CMS’ and ONC’s goals established four years ago.
In SETMA, we work hard to improve our performance. We close our offices for a half day each month to teach our providers, to review performance, to find leverage points for improving that performance and for making sure that we are moving forward. This link is to a summary of SETMA’s October, 2013 provider training: SETMA's Provider Training for October, 2013. Many other monthly meetings summaries are posted on our website at SETMA Presentations.
SETMA’s goal is to be successful in achieving healthcare transformation and improvement, but we would never consider it a mark of success, if we established a standard of success which drove 2/3rd’s of our providers out of SETMA, but neither would we consider it a success if we forever endured substandard performance. Success would be a positive improvement in a reasonable time frame. In whatever time frame, we would consider ourselves a failure if healthcare providers were forced to leave healthcare due to our demands.
- Here is our proposal and the content of our appeal for a temporary, four-year, exemption from MU2, interoperability requirements. For practices like SETMA who:
- Were early adapters (those who adopted EHR before 2006).
- Have demonstrated efforts and results of the use of EHR meaningfully with clinical decision support, addressing of ethnic disparities, use of analytics and the auditing of quality.
- Are participating in a Health Information Exchange.
- Have deployed a Patient Web Portal.
- Achieve Patient-Centered Medical Home of a high level from at least one agency (NCQA, AAAHC, URAC, and Joint Commission).
that they be given four years to make the changes necessary to do interoperability which is clinically meaningful and that ONC work with these practices to define what meaningful, clinical interoperability is with a logical and valid distinction between the value of an HIE and interoperability.
Conclusion
It never occurred to SETMA that we would not easily qualify for MU2. Since discovering that we will not, we have found it will cost $500,000 to $1,000,000 to make this transition and it will require us to suspend our continuous quality improvement activities for six to twenty-four months in order to focus totally upon interoperability. Perhaps nothing is more illustrative of this transformation than SETMA’s The Automated Team which is the logical conclusion to the promise of clinical decision support and which will have to be suspended in favor of ONC’s reform requirements.
Above, the attached document is SETMA’s nomination for the American Medical Informatics Association’s iHealth 2014 Provider Innovation in Informatics Pi2 Award. It gives a brief explanation of The Automated Team. The following is a link to the full explanation of The Automated TeamTutorial for the EMR Automated Team Function. The second attached file is a PDF file of this letter for your records.
Hopefully it is obvious that SETMA is moving ahead with quality improvement and practice transformation and that our request for and exemption and for more time is not out of resistance to the future, nor due to slothfulness. It is our hope that though CMS and ONC have resisted the importations of others, that you will consider this request and proposal as reasonable and rational.
We look forward to hearing from you.
James (Larry) Holly, M.D.
CEO, Southeast Texas Medical Associates (SETMA)
www.jameslhollymd.com
(409) 504-4517
Adjunct Professor
Family & Community Medicine
University of Texas Health Science Center
San Antonio School of Medicine
Clinical Associate Professor
Department of Internal Medicine
School of Medicine
Texas A&M Health Science Center
Acknowledgment is made of the significant contributions to this analysis of:
- Mr. Jon Owen, BS, SETMA’s Chief Clinical Systems Engineer
- Margaret Ross, RN, SETMA’s Director of Operations
- Dr. Laura Teveni, BS, 2013 participant in SETMA’s PC-MH Externship, and 2014 MD Candidate at the University of Texas Health Science Center San Antonio School of Medicine.
- Dr. Jerry Abraham, MPH, 2013 participant in SETMA’s PC-MH Externship, and 2014 MD Candidate at the University of Texas Health Science Center San Antonio School of Medicine.
|