|
Sections of this note
February 17, 2014
Steven M. Berkowitz, MD
1632 Resaca Blvd.
Austin, Texas 78738
steve@smbhealthconsulting.com
Dear Dr. Berkowitz:
Two members of the Governance Board of Southeast Texas Medical Associates (SETMA, LLP, www.jameslhollymd.com) and two of my partners, Dr. Syed Anwar and Dr. Alan Leifeste, attended the Executive Committee retreat for Baptist Hospital of Southeast Texas last weekend. They both gave me a positive report of your presentation and of how pleased they were that they have participated in preparing SETMA for the future. They shared with me that they came away from the retreat with a commitment to finding new and innovative ways of strengthening our partnership with Baptist. The last section of this note is entitled: How Can Healthcare Providers and a Hospital Collaborate to meet the needs of both. It identifies ways in which SETMA believes we do and can collaborate with Baptist effectively. The following link is to The SETMA Model of Care and is integral to everything which is said below: http://jameslhollymd.com/the-setma-way/setma-model-of-care-pc-mh-healthcare-innovation-the-future-of-healthcare.
One the realities my partners identified from the conference is the hospital’s need to increase its market share in the face of DRGs and the pressure of multiple new responsibilities on the part of healthcare providers. The financial pressure this puts on the hospitals balance sheet is real and is unlikely to change. After introducing you to SETMA, I would like to identify ways in which, I believe, SETMA has, can and will continue to support the hospital while facing these new realities. In May, 2000, I made a presentation at the TEPR conference in San Francisco (Toward Electronic Patient Records). The entire presentation can be see at: http://jameslhollymd.com/Your-Life-Your-Health/TEPR-Modified-as-delivered-at-May-2000-conference. This was only three years after SETMA had discovered that the only way we were going to succeed in the emerging healthcare payment model was to learn faster the anyone else. Derived from Peter Senge’s The Fifth Discipline, SETMA learned from Shell Oil, who said, “the only sustainable completive edge is the ability to learn faster than your competitor.”
Part of that learning is adopting new “mental models.” At that time, healthcare providers had been accustomed to being paid $52 for a laboratory test and under the new system, they were being paid $15. Longing for the old reality, their “mental model” of healthcare had them declaring, “We are losing $37 on each test performed. The reality however was that that test only cost the provider $6 to perform. They in fact were making $9 on each test they performed, but they longed for the more “profitable” days rather facing the new reality which was not going to change. The crucial change was to change the mental model from “we are losing money,” to a model that we are making a narrower margin of profit but over all our cost of healthcare delivery is going down.
In that paper, the foundational ideas of “Realities, Responsibilities and Rights” stated:
“Managed Care and the Computerized Patient Record: Realities, Rights & Responsibilities
“Managed Care is the free-market's response to the realities of the healthcare industry. The first reality is that there is no possibility of healthcare financing and management ever returning to the Laissez-faire style practiced up until twenty years ago. Someone is going to control and manage healthcare. The only real question is, ‘Who?’ The financing of healthcare will never return to a system where the medical decision making process takes place in isolation and independent from the question of ‘Who is going to pay for the services?’
“Second, because of the expense of technology and of increasing access to healthcare by a larger population, it is possible for healthcare alone to bankrupt the United States government. Unchecked, the cost of healthcare delivery can prevent the balancing of the Federal budget. The financing of healthcare will never return to a system where the medical decision making process takes place in isolation and independent from the questions of, "How much is a service worth and how much is society willing to pay for it?"
“Third, this means there are limited resources to continue to provide the excellent healthcare, which the citizens of this country presently receive. Someone has to allocate those resources. Who? The financing of healthcare will never return to a system where the medical decision making process takes place in isolation and independent from the question of, ‘What is society's responsibility to its most vulnerable citizens as far as access to affordable healthcare is concerned?’
“Fourth, the government has assumed, by law, the responsibility of providing healthcare to a certain segment of our population, and the government is not going to surrender that responsibility. The facts of this reality are explained by the AAPCC - the Actual Average Per Capita Cost. This is a calculated figure based on HCFA (Health Care Finance Administration) payments for healthcare in the United States. It is calculated on a county-by-county basis for every county in America.
“In the private sector, the principle is the same. While there is no Trust Fund, private companies have budgets and must meet them. Managed care allows industry to budget its healthcare costs by transferring the "risk" to another company. In order to remain competitive, private industry must control healthcare ‘risk.’
“The second relevant issue is ‘responsibility.’
“Each ‘player’ in healthcare delivery today is in an unspoken partnership, which has actual and implied responsibilities.
- Payers (managed-care companies),
- Providers (physicians and other deliverers of health services) and the
- Patients (insured).
“Each ‘player’ has its peculiar responsibilities. The payers, of course, have responsibility for operating within the ‘realities of the AAPCC and/or contract, and for making sure that access to healthcare is maintained. Balancing these responsibilities is a function of the core values and integrity of the managed-care company and of HCFA regulations.
“Providers are responsible for providing outstanding care. In managed care, healthcare is more directed toward preventative healthcare than to treating a problem, which has already developed. Physician must be aware of the differences in cost for care. The reality is that care obtained at one place, which is equal to the quality of care obtained at another, can be three times as expensive. To conserve the healthcare resources for the benefit of everyone, the physician's responsibility is now, not only to assure quality, but cost-effectiveness as well.
“The patient has responsibilities in the managed-care system as well. In order to get the expanded benefits and cost decrease of managed-care, the patient is responsible for utilizing physicians who have contracted with the managed-care company and who are committed to complying with utilization management guidelines, pre-certification of procedures and review of care. The patient also has a responsibility to avoid habits, which cause increased health problems when and where possible, and to cooperate in obtaining preventive care, which can decrease the cost of maintaining health before serious and costly problems develop.
”The Third Relevant Issue is Rights:
“Within these ‘realities’ and ‘responsibilities,’ what are the patients' and providers' rights? The patient has the ‘right’ to excellent healthcare and to access to needed care. However, the rights of the patient must be balanced with the rights of the managed-care company and with the rights of the healthcare providers who provide care. Likewise, the rights of these latter two groups must be balanced against and with the rights of the patient. The patient has the ‘right’ to choose any PCP (Primary Care Provider) who is in the contracted network of the managed-care company and/or for the IPA (Independent Physician Association). And, the patient has the right to go to any specialist who has agreed to cooperate with the managed-care company.
“But, the patient's right to choose his physician cannot interfere with the right of the managed-care company to manage the ‘risk,’ which it has assumed. The patient has the right to request that their favorite physician contract with the managed-care company. But, the physician has the right to refuse. And, the managed-care company has the right to expect the patients and providers to comply with the utilization management guidelines and standards required to manage effectively the ‘risk’ the company has assumed.
“Providers have rights also. Most physicians have resorted to demanding their right to lead health care management. The new realities result in that demand being rejected. If providers wish to exert influence over the delivery of healthcare, they will have to accept their responsibilities and collaborate with payers and patients.”
Before identifying a rational and responsible response for hospitals and their healthcare-provider partners, to the new realities we face, which response will position us to have the right to lead healthcare, I would like to introduce you to SETMA. SETMA has become a PC-MH:
- The National Committee for Quality Assurance (NCQA -- http://www.ncqa.org/Programs/Recognition/PatientCenteredMedicalHomePCMH.aspx) and has received the highest designation, Tier III, for 2010-2013 and 2013-2016.
Medical Home News - Spreading Medical Home Concepts Beyond Primary Care
- The Accreditation Association of Ambulatory Health Care ((AAAHC -- http://www.aaahc.org/accreditation/primary-care-medical-home/) and has received the highest designation by AAAHC for 2010-2011, 2011-2014.
Medical Home News - Keep Calm and Become a Medical Home
- URAC (Known only as URAC -- https://www.urac.org/accreditation-and-measurement/accreditation-programs/all-programs/patient-centered-medical-home-achievement/) and has received the highest designation as PCMH Certification with Electronic Health Records (2014-2017). Both AAAHC and URAC included multiple-day, on-site visits.
Medical Home News - The URAC PCMH Practice Achievement Program
- March 3-5, 2014, SETMA will be surveyed by the Joint Commission for ambulatory care and patient-centered medical home -- http://www.jointcommission.org/accreditation/pchi.aspx.
Medical Home News - The Joint Commission Primary Care Medical Home Certification Program
If we are successful in the Joint Commission survey, SETMA will be the only practice in the United States and for that matter in the world which will simultaneously possess recognition and/or accreditation by all four organizations which evaluate practices for medical home. Even with this remarkable achievement, we continue to learn about medical home and about how to serve our patients better with this remarkable method of healthcare delivery.
SETMA has senior medical students and primary care residents spend a month with SETMA learning the ideals and methods of PC-MH. The following link is to the syllabus which is given to each participant: http://jameslhollymd.com/senior-medical-student-externship/SETMAs-MS4-Patient-Center-Medical-Home-Selective-Syllabus. The following link is to “The Stories and The Ideal of PC-MH”: http://jameslhollymd.com/medical-home which supplements the syllabus.
In May, 1999, SETMA began transforming the care SETMA’s patients receive by defining ten principles on the basis of which our use of electronic health records (EHR) would be built. That month, SETMA published a booklet entitled, More Than a Transcription Service: Revolutionizing the Practice of Medicine: And Meeting the Challenge of Managed Care With Electronic Medical Records (EMR) which Evolves into Electronic Patient Management. This booklet was SETMA’s declaration of our intent of transformation healthcare delivery with electronic health records (EHR). Before the federal concept of “meaningful use” of EHR was published, SETMA was about the process of “using the EHR meaningfully.”
Based on Peter Senge’s “systems thinking,” (see Designing an EMR on the Basis of Peter Senge's The Fifth Disciple by James L. Holly, M.D.), these principles stated that SETMA would:
- Pursue electronic patient management rather than electronic health records, leveraging the power of electronics to improve individual and population health.
- Bring to bear upon every patient encounter that which is known rather than what an individual provider knows.
- Make it easier to do it right than not do it at all.
- Continually challenge providers to improve their performance.
- Easily infuse new knowledge and decision-making tools throughout an organization.
- Promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement (PCPI) Data Sets. (Other measure sets have been added since then)
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
Ten years later on February 16, 2009, with the tools which had been developed in the interim, SETMA began the formal process of transforming patient care into a Medical Home model. In 2009, 2010, 2011, SETMA published three series of articles which described and defined medical home and which documented our progress toward being a medical home. (see 2011 Medical Home Series Two).
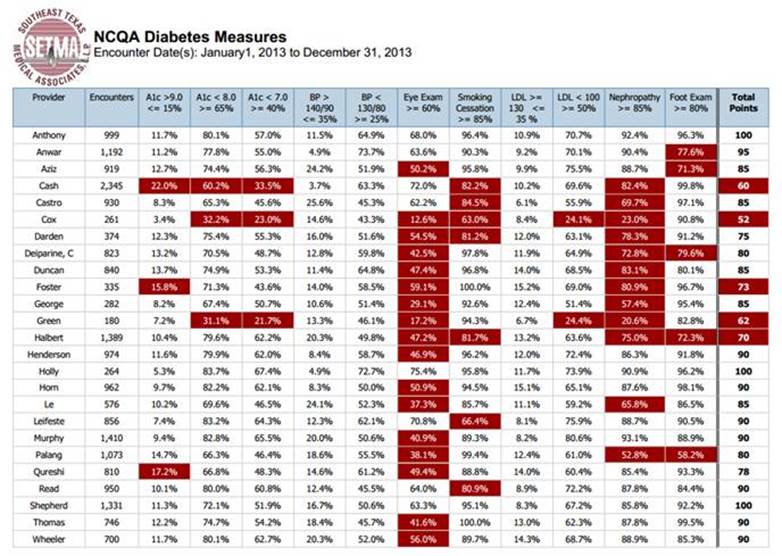
The following link describes SETMA’s public reporting project which began in 2009: http://jameslhollymd.com/Public-Reporting/pdfs/public-reporting.pdf. Since that beginning, each quarter, SETMA has updated our provider performance by provider name for over 300 quality metrics. All five years of reporting by quality metric type can be reviewed at: http://jameslhollymd.com/public-reporting/public-reports-by-type. The following is an example of what our pubic reporting looks like. The provider name is in the far left-hand column. The measure and discriminator is across the top. All that is in red needs improvement; all that is in black meets standards. It takes SETMA 25 seconds to produce this report. You will notice that the nephropathy evaluation requires an 85% performance. There are providers who are at 83.1% but their results still appear in rad as it requires improvement.
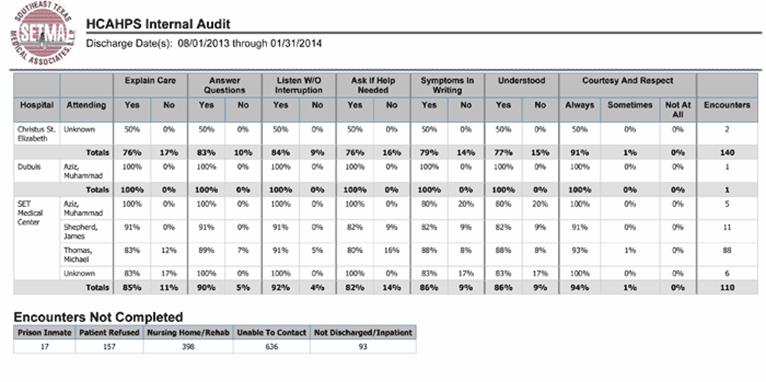
SETMA has done internal patient-satisfaction survey’s for 19 years. But, we always knew these were inadequate to assess the dynamic of patient-centered, medical home care. The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS, hospital setting) and the Consumer Assessment of Healthcare Providers and Systems (CAHPS, ambulatory setting) had always seemed daunting to healthcare providers. In July, 2013, SETMA had its monthly review of our quality performance in the hospital and one of the metrics is HCAHPS performance. At that time, I asked for the details on HCAPHS. Starting on July 15, 2013, SETMA launched a tracking tool in our EHR whereby HCAHPS was added to SETMA’s Care Coaching Call completed by SETMA’s Care Coordination Department. By July 30, 2013, we were completing our own HCAHPS survey. While it did not replace the hospital’s vendor produced data, it gave SETMA a quality improvement method so that we could measure our performance ( Hospital Consumer Assessment Of Healthcare Providers and Systems (HCAHPS)).
SETMA’s In-House HCAHPS Internal Audit for August 1, 2013 through January 31, 2014
This process revealed to me the value of HCAHPS and CAHPS PC-MH in measure the patient-centeredness of our care. In August, 2013, we contracted with an NCQA certified vendor to complete quarterly surveys. The following links shows the public report SETMA did on our first quarter CAHPS survey: NCQA's New Distinction in Patient Experience Reporting. The following was reported in a Southeast Texas newspaper.
The Completed CAPHS Survey for the 4th Quarter of 2013
This graph is the Expanded Executive Summary of SETMA’s first quarter of our gathering of the Consumer Assessment Healthcare Providers and Services measurement of patient satisfaction. The first column is the CAHPS PCMH Benchmark from 2012 CAHPS Data. The other five columns are the results of the CAHPS survey for each of SETMA’s five clinics: SETMA 1 on Calder; SETMA 2 on College; the Mark Wilson Clinic on Dowlen; and our Mid County and Orange Clinics.
The “Noteworthy Findings” of the Expanded Executive Summary of the CAHPS survey are that SETMA’s “results are not significantly different in any of the categories“ from the Benchmarks. This means that SETMA is doing well, however, not as well as we would like. In our January 21st Provider Training Session, we will review each of the below “composite ratings” and discussion ways in which we can improve. We expect that while we are doing “OK,” that in coming quarters, we will see significant improvement. That is the goal.
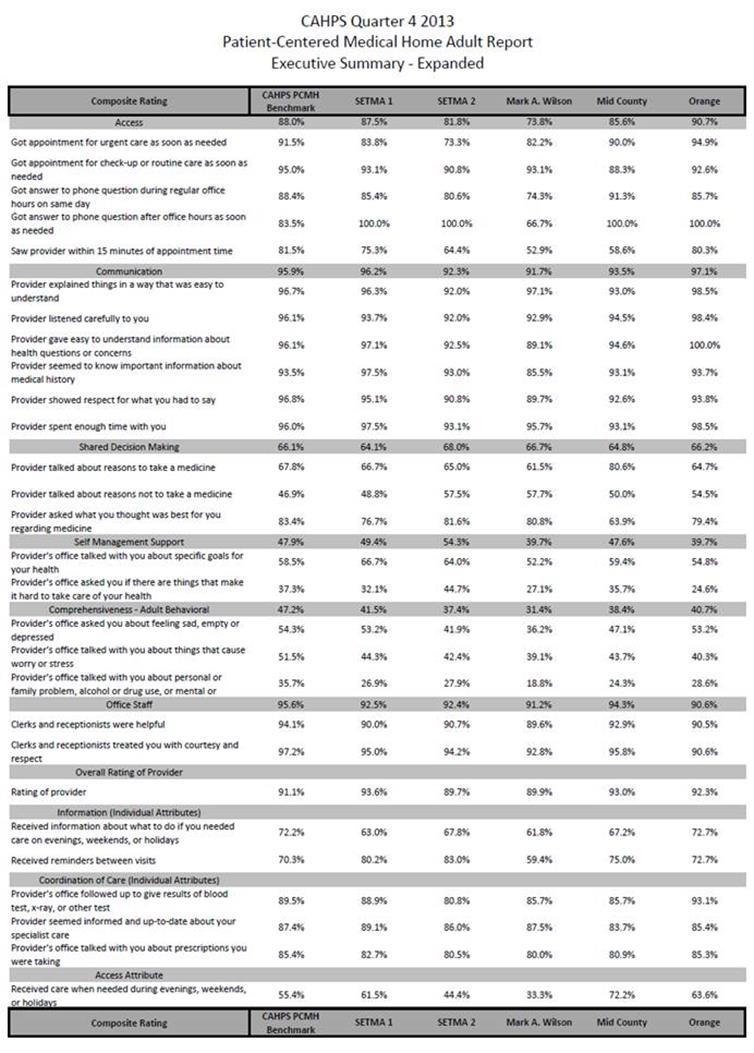
As more of SETMA’s patients participate in the CAHPS surveys and as SETMA’s providers and staff study the results, we will improve the care we deliver. Patient satisfaction is a key part of the transformation of healthcare. These surveys are providing SETMA will opportunities to improve our patient-centric care.
These are also safe guards against abuse and/or misuse of the patient-provider relationship are in place at SETMA by:
- Our Care Coordination Department’s completion of the Hospital Consumer Assessment of Healthcare Providers and Services (HCAHPS) on every patient who leaves the hospital. An explanation of this program is made on SEMTA’s website for review by our patients and community at Hospital Consumer Assessment Of Healthcare Providers and Systems (HCAHPS).
- SETMA’s employment of an independent, NCQA-endorsed agency for the quarterly completion of the Consumer Assessment of Healthcare Providers and Systems (CAHPS). An explanation of this program is made on SETMA’s website for review by our patients and community at Consumer Assessment of Health Care Provider and Systems.
The following link is to the tutorial for SETMA’s Hospital Care Summary and Post Hospital plan of Care and Treatment Plan:
http://jameslhollymd.com/epm-tools/hospital-care-summary-and-post-hospital-plan-of-care-and-treatment-plan-tutorial.
In September, 2010, SETMA changed the name of the “discharge summary” to the new name above. Longer, but much more functional, this name identified this transition of care tool as an imperative part of our hospital collaboration. Since 2009, SETMA has discharged over 21,000 patients from the hospital. 98.7% of the time, the transition of care document has been completed at the time the patient leaves the hospital.
Patient Engagement and Activation Documents
With all documents created in the care of a patient whether:
- Ambulatory disease management plan of care or treatment plan
http://jameslhollymd.com/epm-tools/Medical-Home-Plan-of-Care-and-Treatment-Plan
- Automated Team Patient Engagement and Activation Document
- Ambulatory care summary of care document
- Hospital Admission Plan of Care and Treatment Plan
Hospital Admission Plan of Care
- Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan
Example of SETMA's Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan. (De-identified)
the key is to engage and activate the patient in their own care.
Nomenclature Can Confuse Function
While the traditional “discharge summary” should have been the most important document created during a patient’s hospital stay, it historically came to be nothing but a document created for an administrative and billing function for the hospital and attending physician. It has long cease to being a dynamic document for the improvement of patient management. The “discharge summary” rarely provided continuity of care value, or transitions of care information, such as diagnoses, reconciled medication list, or follow-up instructions. In reality, the “discharge summary” was often completed days or weeks after the discharge and was a perfunctory task which was only completed when hospital staff privileges were threatened or payment was delayed.
The “discharge summary” should have always been a transition-of-care document which not only summarized the patient’s care during the hospitalization but guided the patient’s post-hospital care with a plan of care and treatment plan. In this way, the document would have been a vehicle for patient engagement and activation.
Changing the Name to Clarify the Function
In September, 2010, SETMA representatives as an invited participate attended a National Quality Forum conference on Transitions of Care. (NQF - Summary of Dr. Holly's Comments - September 2nd, 2010) During that conference, SETMA realized that the name “discharge summary” needed to be changed. It was thought that a name change would clarify and focus the intent of this critical document. The name was changed to “Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan.” The purpose and content of the new document was defined as:
- Follow-up instructions and plans - appointments with all healthcare providers who participated in the patient’s inpatient care. These appointments should be made before the patient leaves the hospital and the following information given to the patient and/or family or other principle care giver: time and date of appointment, name, address and telephone number of the provider or providers involved and the reason for the appointment.
- Referrals - appointments with new healthcare providers who have not been involved in the patient’s care but who will participate in care post-hospital. An example might be an oncologist who will treat the patient’s newly diagnosed prostate cancer but who did not see the patient in the hospital encounter. The same information as in the “follow-up” should be given to the patient in writing.
- Procedures - any testing or examinations which are to be done after the hospital should be scheduled before the patient leaves the hospital and all contact information included in the “Post Hospital Plan of Care and Treatment Plan.”
- Testing which is not resulted at discharge - a definite plan must be established prior to discharge for the reporting to and discussing with the patient any test results which have not complete at the time of discharge.
- Reconciled Medication List - the most common cause for preventive readmissions is medication errors. An accurately reconciled medication lists which is clearly communicated to the patient with assurance that the patient can and has obtained their medication is a critical part of a transition of care document.
- Hospital Care Coaching Call - This call, which lasts 12-30 minutes, is scheduled the day following discharge from the hospital. It provides a valuable bridge between inpatient and ambulatory care. In January, 2013, CMS published Transitions of Care Management Codes with which to pay primary care providers for the tasks they perform in transition care. One element required for billing one of these codes is the provider having made a telephone contact with the patient within forty-eight hours of the patient’s discharge from the hospital. The following link explains the Transition of Care Management Code requirement: Transitions of Care Management Coding (TCM Code) Tutorial
The Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan should acknowledgment that a follow-up telephone call has been scheduled for the day following discharge which call will include at least the addressing of the following information:
- An internal review and audit of the Hospital Consumer Assessment of Healthcare Provider and Systems.
- Review of reconciled medication list.
- Review of follow-up care and referrals.
- Patient’s care and understanding of that care.
- Patient’s engagement and activation in their care.
Discharge Summary versus Hospital Care Summary - Post Hospital Plan of Care and Treatment Plan
The significant differences between these two documents are:
- The Hospital Care Summary MUST BE completed at the time the patient is discharged from the hospital because it is not an administrative tool or simply a means where by a charge can be made. It is THE critical transition of care and continuity of care document linking the inpatient care with the ambulatory care.
From 2008 - 2013, SETMA has discharged over 20,000 patients from the hospital. 98.7% of the time the Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan has been completed at the time the patient leaves the hospital. Prior to 2003, before SETMA recognized the critical value of this transition of care document, we were routinely thirty days behind in the completion of the discharge summary.
When SETMA’s CEO, took over responsibility for leading SETMA’s inpatient work, he asked the question, “How far behind are you with discharge summaries?” When the answer was 30 days, he asked, “Are you ever more than 30-days behind, or are you ever less than 30-days behind?” The answer to both was, “No.” The staff was then asked, “If you are never more than 30-days behind and if you are never less than 30-days behind, what does that tell you?” When no answer was given, the CEO asked, “If you once get caught up, where would you stay?” The staff realized that if they got caught up, as they had stayed 30-days behind, always; they would stay caught up, always.
- Because the Hospital Care Summary is being completed at the time of the patient’s discharge, the document serves as a patient engagement and activation tool. It allows the patient to know what they need to do, when and where they are to do it and why they needed to do it. Because this document is completed at the time the patient leaves the hospital, the Summary contributes to active, reconciled medication lists.
- Because the document is completed in the ambulatory EMR which is also used in the clinic, it meant that the provider seeing the patient in the clinic would have a complete explanation of what was done to and for the patient in the hospital. The reconciled medication list done on admission to the hospital, on discharge from the hospital, at the time of the care coaching call and at the follow-up visit in the clinic is the same in all four.
- In order to manage transitions of care and to audit the process, SETMA created the Inpatient Medical Record Census (IMRC). This is an electronic documentation of when and where a patient is admitted, when the history and physician is completed, when the Hospital Care Summary and Post Hospital Plan of Care is completed and questions posted by SETMA’s Central Business Office about hospital charges.
This link is to a presentation I made to the Massachusetts Medical Society on the power of Analytics in primary care: The Importance of Data Analytics in Physician Practice. Quality in healthcare remains an elusive quest from the standpoints of definition, determination and demonstration. In quality metric design, whether process or outcomes, the piece which is most often missing is a combination of tracking and auditing. Join us as we learn how clinicians at Southeast Texas Medical Associates, LLP, a multi-specialty practice in Beaumont, Texas, are using business intelligence and analytics for clinical performance measurement, auditing of care practices, and improvement in patient outcomes.
The new competencies which are going to be required for effective and successful population management are going to involve what IBM calls an “Analytics Quotient”. (See the IBM Paper entitled, Transforming healthcare delivery with analytics.) ’Information’ is inherently static while ‘learning’ is dynamic and generative (creative). In The Fifth Discipline, Peter Senge, said: ‘Learning is only distantly related to taking in more information.’ Classically, taking in more information has been the foundation of medical education. Traditional CME has perpetuated the idea that ‘learning; is simply accomplished by ‘learning more facts.’ Analytics transform knowledge into an agent for change. In reality, without analytics, we will neither know where we are, where we are going, or how to sustain the effort to get there.
For transformation to take place through knowledge, we must be prepared to ask the right questions, courageously accept the answers and to require ourselves to change. Healthcare transformation, which will produce continuous performance improvement, results from internalized ideals, which create vision and passion, both of which produce and sustain ‘creative tension’ and ‘generative thinking.’ Transformation is not the result of pressure and it is not frustrated by obstacles. In fact, the more difficult a problem is, the more power is created by the process of transformation in order to overcome the problem. The greatest frustration to transformation is the unwillingness or the inability to face current reality.
Often, the first time healthcare provides see audits of their performance, they say, ‘That can’t be right!’ ‘Through analytics“ tracking data, auditing performance, statistical analysis of results “ we learn the truth. For that truth to impact our performance, we must believe it. Through acknowledging truth, privately and publicly, we empower sustainable change, making analytics a critical aspect of healthcare transformation.
While an Electronic Health Record (EHR) has tremendous capacity to capture data, that is only part of the solution. The ultimate goal must be to improve patient care and patient health, and to decrease cost, not just to capture and store information! Business Intelligence (BI) statistical analytics are like coordinates to the destination of optimal health at manageable cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and population data.”
Healthcare providers generally have an high IQ but most also have a very low AQ. Population management cannot be done without analytics.
This is the link to SETMA’s 57-page report to the Robert Wood Johnson Foundation’s research project where 30 exemplar practices were selected from across America to study work force innovations: The Primary Care Team: Learning from Effective Ambulatory Practices (PCT-LEAP): Performance Measures Worksheet - Robert Wood Johnson Foundation. SETMA’s philosophy of quality metrics is discussed at length in this document. SETMA is also involved with the American Board of Family Medicine in a research project.
The reality is that DRG’s, bundle payments, transitioning from a volume based to a value based system. This transition will put pressure upon all of us and that pressure will increase. I believe that SETMA is well positioned to meet the challenges of the future:
- The March, 2013, Commonwealth Fund white paper entitled, “Paying for Value: Replacing Medicare’s Sustainable Growth Rate Formula with Incentives to Improve Care,.” supports that judgment. SETMA providers reviewed this document in our April, 2013 Provider training session. That review showed that SETMA is currently doing everything that the Commonwealth Fund paper recommended for the future of healthcare payment. (See: Provider Payment Reform: Incentives to Improve Care)
- The U.S. House Ways & Means & Senate Finance Committee Staff’s October 30, 2013 Discussionentitled, “DraftSustainable Growth Rate Repeal & Medicare Physician Payment Reform” also supports that judgment. SETMA studied this draft in our November 19, 2013 Provider Training session. That can be reviewed at: Discussion Draft: Sustainable Growth Rate Repeal & Medicare Physician Payment Reform.
- SETMA’s medical record documentation is designed to maximize the hospital’s DRG value through documenting all relevant co-morbidities even though that is counter-intuitive when we share global risk for those patients.
- This same documentation assists the hospital in establish and appropriate and valid Case Mix Index which also increases the hospital’s revenue.
- Our aggressive management of patients and our spending of $1,300,000 a year of our own money to have staff in the hospital around the clock enables us to control our length of stays which also maximizes the value of the DRG to the hospital.
- Our Care Transitions and Care Coordination program and our Care Coaching calls the day after the hospital discharge decrease the readmissions which decreases hospital penalties which started in October, 2013.
- Our monthly meetings with the hospital administration and our review of our performance including lab and procedure cost, consultations, core measures performance, HCAHPS scores, etc., improves the value of our patients to the hospital. As I have asked and you have indicated whether or not SETMA’s contribution to the hospital’s bottom line, we are pleased to know that our partnership is a positive to your bottom line.
- Our participating in your indigent, uninsured and unassigned patient admissions (12 days a month) and our management of these patients in the same way we do our private patients helps you minimize your losses from the uncompensated care of our communities neediest.
- SETMA’s aggressive efforts to:
- Direct our private patients to Baptist while respecting the patient’s right to choose their hospital,
- our collaboration with at least two-free standing emergency rooms to direct their admissions to Baptist,
- our efforts to attract specialist to Baptist and
- to, again within the respect for patient choice, direct procedures and surgeries to Baptist, and
- our opposition to the new hospital owned by specialist, are all part of our support of Baptist.
Sincerely yours,
James (Larry) Holly, M.D.
C.E.O. SETMA
www.jameslhollymd.com
Adjunct Professor
Family & Community Medicine
University of Texas Health Science Center
San Antonio School of Medicine
Clinical Associate Professor
Department of Internal Medicine
School of Medicine
Texas A&M Health Science Center
|