|
June 15, 2017
Mara McDermott
Vice President of Federal Affairs
CAPG, the Voice of Accountable Physician Groups
1501 M Street NW Suite 640
Washington, DC 20005
Dear Mara:
This follow-up to our telephone discussion yesterday will hopefully allow for these concepts to be incorporated into our ongoing efforts to move MACRA and MIPS forward by including Medicare Advantage (MA) as a Alternative Payment Model (APM). Both CAPG and SETMA (Southeast Texas Medical Associate, LLP) are committed to the MA program in which SETMA has been working for nineteen years. (Both in MA and its predecessors)
We both believe that MA should be given standing as an APM of care in that it possesses all three elements required for an APM, which are:
- Emphasis upon and proved results in improving the quality (Q) and safety of healthcare and the improvement of outcomes of care.
- Improvement in the value (V) of Medicare and Medicaid by matching improved quality with decreased cost (C) to increase value, i.e., Q/C = V.
- Assumption of significant risk. In this case, MA out performs all other APM as MA assumes full and total risk.
The barrier to CMS and HHS designating MA as an APM is obviously that CMS and HHS do not see a benefit for their organizations for the including of MA in the MACRA/MIPS program in that they cannot identify new savings. Unlike other APM, CMS and HHS have administratively created additional savings for themselves by decreasing MA reimbursement by 4% a year for 7 years to decrease their cost by 28%. In addition, our IPA alone has a $1,700,000 tax for the Affordable Care Act which further creates savings for CMS and HHS. Both of these moves have created tremendous pressure on practices like SETMA to remain solvent while participating in MA.
In order to promote our position, the discussion should be enlarged to include the following deficiencies in MACRA and MIPS:
- The reality is that with MACRA and MIPS, a bonus is paid to one, only if a penalty is assessed to another. This make healthcare a “zero sum game” where for there to be a winner, there must be a loser. I object to that. I would like it to be the case where the system is designed to where everyone can be a winner.
- I would like to find the people who are in the lower, left hand quadrant of the scatter graph created by CMS’ Quality Resource and Utilization Report (QRUR). These practices have been determined to have a low quality and a high cost. I suspect these are not bad people. I would like to have the opportunity to work with them to see them improve their quality and decrease their cost.
In fact, I would recommend that all practices which fall into this quadrant be entered into CMS’ Transforming Clinical Practice Initiative (TCPI) in order to help them improve. Of course, this would mean that the goal of MACRA and MIPS would have to be changed to where everyone could be a winner rather than depending upon encouraging one group by the discouraging of another.
- It often seems as if those who provide care to the most vulnerable and the neediest of our citizens, those who are most socially responsible, are in fact the ones being punished by CMS and HHS. Those who refuse to care for Medicare or Medicaid are free, it seems, to make a fortune without interference from anyone. That does not seem like a plan which will work in the long run.
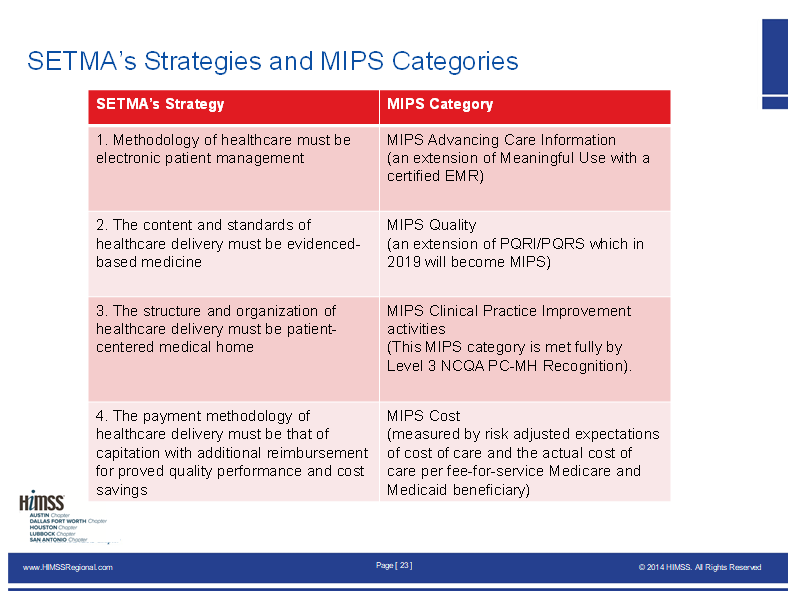
SETMA’s comments about MACRA and MIPS are made in the context of the following relationships between SETMA’s history and MIPS:
- On October 6, 2016, SETMA discovered that the four categories defined by MIPS in 2015 correlate with the four strategies SETMA defined in 2000-2005 for the transformation of our practice.
- Early in our development, SETMA came to believe that the key to the future of healthcare transformation was an internalized ideal and a personal passion for excellence, rather than reform which comes from external pressure and regulations.
- Transformation is self-sustaining, generative and creative. In this context, SETMA believes that efforts to transform healthcare may fail unless SETMA’s four strategies described below are employed.
SETMA’s transformative efforts are dependent upon the following four standards which mirror the four categories of MIPS:
Furthermore, the most difficult aspects of the MACRA and MIPS program are:
- There is not an absolute standard against which healthcare providers will be measured.
- Provider evaluation will always be a judgment made two years after the fact, i.e., you will practice and perform in 2017, in 2018 you performance will be aggregated , but it will be 2019 before you know where you stand.
- The biggest problem with this moving target is that you have to assume that everyone's results mean the same performance. That is not necessarily the case.
- It is possible that if everyone begins to perform at a high standard that the distribution would be very narrow.
- The possibility exists that a person could be performing at a 95% level and still be a standard deviation below the mean which could result in a penalty for a performance which everyone would consider excellent.
- Larger organizations and/or duplicitous organizations (the two are not synonymous) can find or use methods which meet the standard without achieving the excellence of care implied by the measurement.
- Organizations may focus on intentionally meeting a few metrics which could result in a high performance on an artificial metric without a significant improvement in care or outcomes. SETMA addressed this by making the fulfillment of quality metrics “incidental” to excellent care rather their being the “intention” of our model of care.
The most fundamental problem with MACRA and MIPS is that their design is flawed. At the core of SETMA’s four strategies is the belief that one or two quality metrics will have little impact upon the processes or the outcomes of healthcare delivery, and that they will do little to reflect quality outcomes in healthcare delivery. Even the six metrics required by MIPS in 2019 will not necessarily and causatively improve healthcare outcomes.
In the CMS mandatory Physician Quality Reporting System (PQRS), which in 2011 replaced the voluntary Physicians Quality Reporting Initiative (PQRI) healthcare providers are required to report on nine quality metrics of the providers’ choice, but this requirement will be reduced to six quality metrics under MIPS in 2019. SETMA argues that this is a minimalist approach to providers quality reporting and is unlikely to change healthcare outcomes or quality.
SETMA currently tracks over 200 quality metrics on each patient seen and for the past nine years, we have publicly reported by provider name on our performance on these metrics at www.jameslhollymd.com. However, this does not tell the whole story. SETMA employs two definitions in our use of quality metrics in our transformative approach to healthcare:
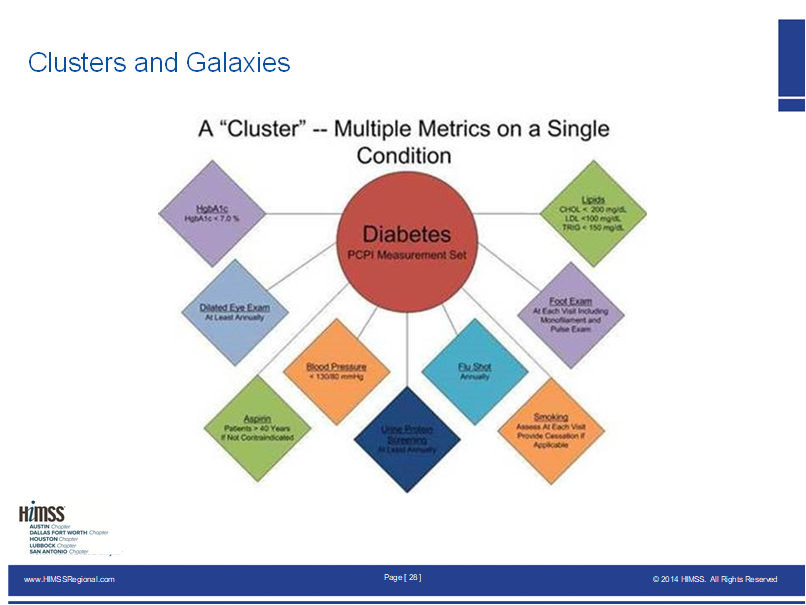
- A “cluster” is seven or more quality metrics tracked for a single condition, i.e., diabetes, hypertension, etc.
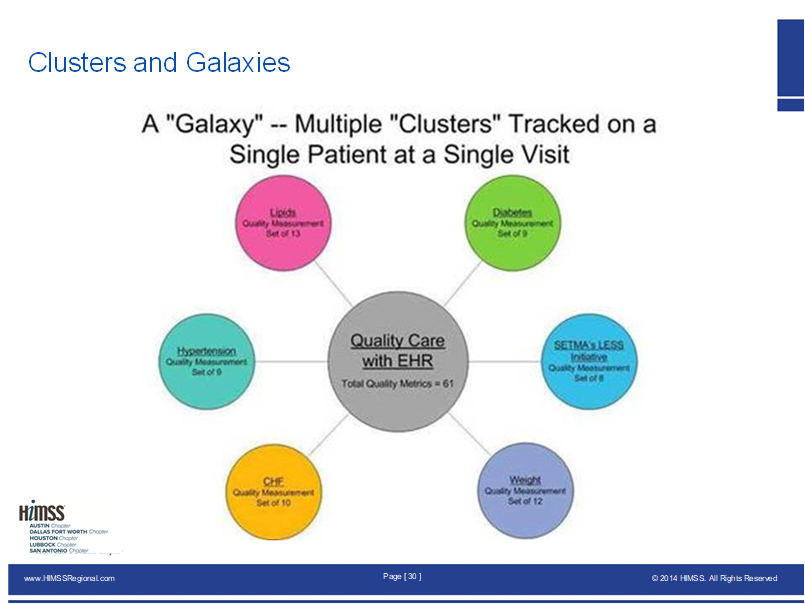
- A “galaxy” which is multiple clusters tracked in the care of the same patient, i.e., diabetes, hypertension, lipids, CHF, etc.
SETMA believes that fulfilling a single metric or a few quality metrics on a single condition does not change outcomes, but fulfilling “clusters” and particularly “galaxies” of metrics, which are measurable by the provider at the point-of-care and where provider performance is publicly reported, can and will change outcomes.
In SETMA’s model, a single patient, at a single visit, for a single condition, will have eight or more quality metrics fulfilled, which WILL change the outcome of that patient’s treatment.
But the “real” leverage comes when multiple “clusters” of quality metrics are measured in the care of a single patient who has multiple chronic conditions. The following illustrates a “galaxy” of quality metrics. A single patient, at a single visit, with multiple “clusters” involving multiple chronic conditions thus having 60 or more quality metrics fulfilled in his/her care, which WILL change the quality of outcomes and which will result in the improvement of the patient’s health. And, because of the improvement in care and health, the cost of that patient’s care will inevitably decrease as well. Remember that foundational to this concept is that the fulfillment of quality metrics is incidental to excellent care rather than being the intention of that care.
For 2015 PQRS, SETMA was required to report on 9 PQRS measures. In 2017, MIPS requires us to report on six measures.
From those measures a Quality and Cost score will be calculated to determine performance for MACRA and MIPS incentive payments. These calculations are contained in the Quality Resource and Utilization Report (QRUR).
In 2016, SETMA received from CMS, our QRUR for performance in 2014 which was analyzed by CMS in 2015. In 2017, provider performance is being reporting to CMS. It will be analyzed in 2018 and payments for 2019 will be based on the results. We do not believe that the design of MACRA and MIPS will improve the quality of care; it will only establish an artificial and invalid definition of quality which will be substituted for “real” change in healthcare transformation and outcomes.
As anticipated by SETMA, MACRA and MIPS can change the future of healthcare but not in its current form.
I look forward to further discussions about these issues.
Sincerely yours,
James (Larry) Holly, M.D.
C.E.O. SETMA
www.jameslhollymd.com
Adjunct Professor
Family & Community Medicine
University of Texas Health San Antonio
The Joe R. and Teresa Lozano Long School of Medicine
Clinical Associate Professor
Department of Internal Medicine
School of Medicine
Texas A&M Health Science Center
|