|
Recently, the Opinion Pages of the New York Times included a brief description of the problem facing primary care physicians who are confronted by a patient who wants a narcotic pain medication. When I started practicing medicine over 40 years ago, doctors ordered urine drug screens in order to discover patients who were taking street drugs such as marijuana, heroin, etc. Today, urine drug screens are being recommended and/or required to discover patients who are NOT taking their prescription pain medication and other drugs which have a high potential for abuse.
The issue is that many patients get prescriptions filled and rather than taking the medicines as prescribed, they are not taking them at all and are selling them. Every month, the Texas Medical Board publishes the names of doctors whose licenses and/or prescribing privileges have been suspended or revoked due to inadequate record keeping in the prescribing of narcotic pain medications and/or who are over prescribing such drugs without adequate documentation of their necessity,.
Many physicians have stopped prescribing any narcotic pain medication, thinking that that solves their problem. However, in Texas and in almost every other state, medical practice acts include not only standards for when and how to prescribe narcotics but also the admonition that the under treatment of pain is as culpable as the over prescribing of narcotics and/or the over prescribing of narcotics without adequate surveillance.
The following is an excerpt from the NYT’s article about pain medication prescribing and use:
“MY patient Mr. W. wheeled himself into my office for a checkup. He’d lost a leg to diabetes and was also juggling hypertension, obesity, vascular disease and elevated cholesterol. He was an amiably cranky fellow in his mid-60s who’d used heroin in the past though had been clean for decades. As we finished up and I handed him his stack of prescriptions, he said, “Oh, by the way, Dr., I was wondering if you could prescribe me the oxycodone I use for my back. I’ve been getting it for years from my pain doctor in the Bronx, but that clinic closed,” he explained. “So now I’ve got to get it from my primary care doctor.”
...Here it was again: the dreaded pain conundrum. A patient requests a strong pain medication and the doctor has to figure out whether the request is legitimate. This is an aggravating situation on many levels. On the individual level, there are the immediate issues of trust — do I trust Mr. W.’s story, and, conversely, how will my decision affect Mr. W.’s trust in me?”
Then there is the larger issue of how we doctors treat pain in general. A 2011 report from the Institute of Medicine highlighted how poorly the medical field handles pain. Undertreating pain, we are admonished, violates the basic ethical principles of medicine. On the other hand, we are lambasted for overprescribing pain medications, enabling addicts and creating an epidemic of overdose deaths....
“Realistically, a drug addict denied will almost always find a way to get meds, but a person with real pain truly suffers. And so despite some misgivings, I gave Mr. W. a prescription for oxycodone and scheduled another visit to discuss his pain issues in more depth.”
For over ten years, SETMA has systematized pain-medication management with a tool which can be reviewed at: http://jameslhollymd.com/epm-tools/Tutorial-Pain-Management. Included in this tool is “SETMA’s refill policy” which states:
“This represents SETMA's refill policy. This policy will print on the pain management document that will be given to the patient at the end of the visit. This policy states:
“Under no circumstances will the medication be refilled:
- Prior to the renewal date at the prescribed dosage and frequency of use.
- Without the patient being seen in the office
- Without evidence of continuing need for medication
- On the weekend, evenings after hours, holidays or other times when your regular doctor is not available.
“The following reasons will not be accepted by any SETMA provider for an early refill of pain medication and/or medication with a significant potential for habituation:
- My medications were stolen.
- I only got half of the prescription filled.
- I dropped my medications into the sink, the sewer, the swimming pool or other watery body.
- I left my medication in my hotel on my trip.
- I missed my appointment.
- The neurosurgeon and/or the surgeon cancelled my appointment.
“Pain Medication Should Last - the date will automatically appear here which is a calculation of the number of pills given including refills and the maximum daily dose. This date will be the minimum time for a refill but does not indicate that the prescription should be refilled on this date. See explanation in number five below.”
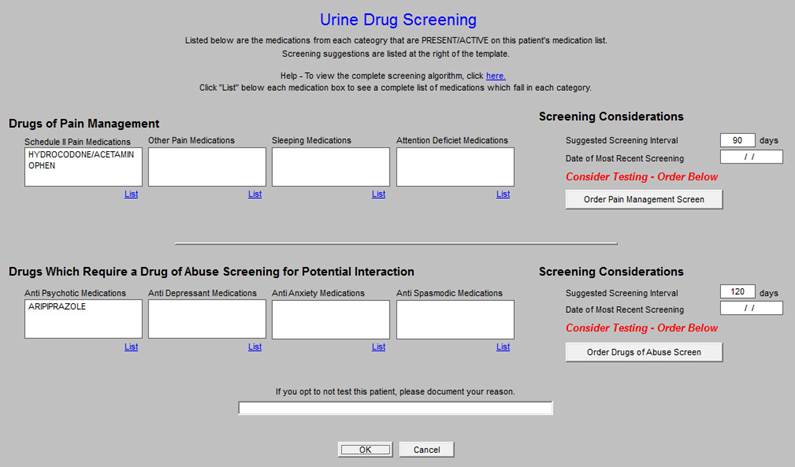
Since the development of this tool, the above described State Medical Board regulations have been strengthen and SETMA has responded to the changes by adding another tool which recommends the frequency of drug screening for “Drugs of Abuse” and/or “Drugs which require a Drug of Abuse Screening for Interaction.” The steps of action with this tool are:
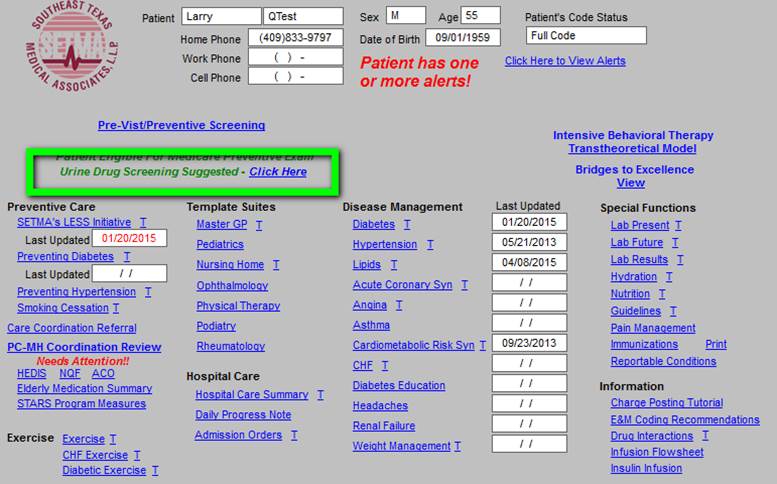
- When the patient’s electronic medical record is opened and the patient is taking drugs in either of these categories, an alert appears which states, “Urine Drug Screen Suggested.”
- Next to this suggestion is a button entitled “click here.” When this button is clicked, the following appears.
- Any drugs which have been prescribed for the patient and which should be periodically screen will appear in the appropriate box.
See the template below with the alert outlined in green. This does not mean that you must do a urine drug screen but that you should think about it and document why if you opted not to do one.
When the Urine-Drug-Screening tool is deployed, there are several reasons why a “suggested” drug screen alert might not be done, although many of those reasons are being shown to be invalid as we find that when we do the screen it proves the patient is not taking the medication.
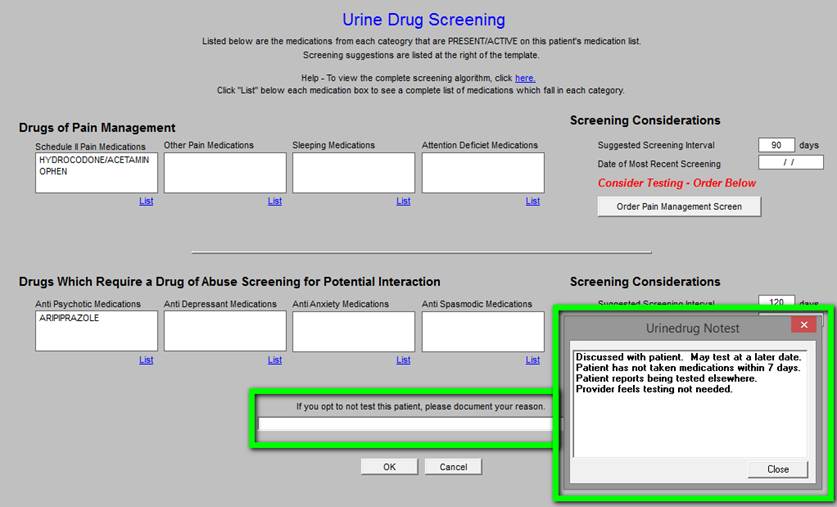
If you opt not to do a drug screen, you can document your reason for not doing by click in the space which is outlined in green below and then selecting the appropriate reason in the second box below, also outlined in green.
SETMA is committed to complying with all State Board of Medicine requirements and to making sure that we use narcotics appropriately. These tools help us do that more efficiently.
|