With all documents created in the care of a patient whether:
- Ambulatory disease management plan of care or treatment plan http://jameslhollymd.com/epm-tools/Medical-Home-Plan-of-Care-and-Treatment-Plan
- Automated Team Patient Engagement and Activation Document
- Ambulatory care summary of care document
- Hospital Admission Plan of Care and Treatment Plan Hospital Admission Plan of Care
- Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan Example of SETMA's Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan. (De-identified)
the key is to engage and activate the patient in their own care.
While the traditional “discharge summary” should have been the most important document created during a patient’s hospital stay, it historically came to be nothing but a document created for an administrative and billing function for the hospital and attending physician. It has long cease to being a dynamic document for the improvement of patient management. The “discharge summary” rarely provided continuity of care value, or transitions of care information, such as diagnoses, reconciled medication list, or follow-up instructions. In reality, the “discharge summary” was often completed days or weeks after the discharge and was a perfunctory task which was only completed when hospital staff privileges were threatened or payment was delayed.
The “discharge summary” should have always been a transition-of-care document which not only summarized the patient’s care during the hospitalization but guided the patient’s post-hospital care with a plan of care and treatment plan. In this way, the document would have been a vehicle for patient engagement and activation.
In September, 2010, SETMA representatives as an invited participate attended a National Quality Forum conference on Transitions of Care. (http://jameslhollymd.com/Letters/nqf-summary-of-dr-hollys-comments-sept-2-2010) During that conference, SETMA realized that the name “discharge summary” needed to be changed. It was thought that a name change would clarify and focus the intent of this critical document. The name was changed to “Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan.” The purpose and content of the new document was defined as:
- Follow-up instructions and plans - appointments with all healthcare providers who participated in the patient’s inpatient care. These appointments should be made before the patient leaves the hospital and the following information given to the patient and/or family or other principle care giver: time and date of appointment, name, address and telephone number of the provider or providers involved and the reason for the appointment.
- Referrals - appointments with new healthcare providers who have not been involved in the patient’s care but who will participate in care post-hospital. An example might be an oncologist who will treat the patient’s newly diagnosed prostate cancer but who did not see the patient in the hospital encounter. The same information as in the “follow-up” should be given to the patient in writing.
- Procedures - any testing or examinations which are to be done after the hospital should be scheduled before the patient leaves the hospital and all contact information included in the “Post Hospital Plan of Care and Treatment Plan.”
- Testing which is not resulted at discharge - a definite plan must be established prior to discharge for the reporting to and discussing with the patient any test results which have not complete at the time of discharge.
- Reconciled Medication List - the most common cause for preventive readmissions is medication errors. An accurately reconciled medication lists which is clearly communicated to the patient with assurance that the patient can and has obtained their medication is a critical part of a transition of care document.
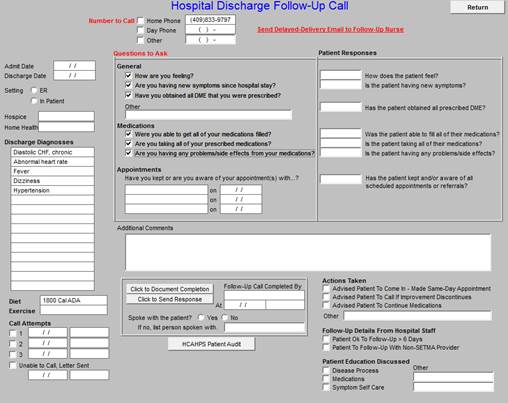
- Hospital Care Coaching Call - This call, which lasts 12-30 minutes, is scheduled the day following discharge from the hospital. It provides a valuable bridge between inpatient and ambulatory care. In January, 2013, CMS published Transitions of Care Management Codes with which to pay primary care providers for the tasks they perform in transition care. One element required for billing one of these codes is the provider having made a telephone contact with the patient within forty-eight hours of the patient’s discharge from the hospital. The following link explains the Transition of Care Management Code requirement: http://jameslhollymd.com/epm-tools/transition-of-care-management-code-tutorial
The Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan should acknowledgment that a follow-up telephone call has been scheduled for the day following discharge which call will include at least the addressing of the following information:
- An internal review and audit of the Hospital Consumer Assessment of Healthcare Provider and Systems.
- Review of reconciled medication list.
- Review of follow-up care and referrals.
- Patient’s care and understanding of that care.
- Patient’s engagement and activation in their care.
The significant differences between these two documents are:
- The Hospital Care Summary MUST BE completed at the time the patient is discharged from the hospital because it is not an administrative tool or simply a means where by a charge can be made. It is THE critical transition of care and continuity of care document linking the inpatient care with the ambulatory care.
From 2008 - 2013, SETMA has discharged over 20,000 patients from the hospital. 98.7% of the time the Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan has been completed at the time the patient leaves the hospital. Prior to 2003, before SETMA recognized the critical value of this transition of care document, we were routinely thirty days behind in the completion of the discharge summary.
When SETMA’s CEO, took over responsibility for leading SETMA’s inpatient work, he asked the question, “How far behind are you with discharge summaries?” When the answer was 30 days, he asked, “Are you ever more than 30-days behind, or are you ever less than 30-days behind?” The answer to both was, “No.” The staff was then asked, “If you are never more than 30-days behind and if you are never less than 30-days behind, what does that tell you?” When no answer was given, the CEO asked, “If you once get caught up, where would you stay?” The staff realized that if they got caught up, as they had stayed 30-days behind, always; they would stay caught up, always.
- Because the Hospital Care Summary is being completed at the time of the patient’s discharge, the document serves as a patient engagement and activation tool. It allows the patient to know what they need to do, when and where they are to do it and why they needed to do it. Because this document is completed at the time the patient leaves the hospital, the Summary contributes to active, reconciled medication lists.
- Because the document is completed in the ambulatory EMR which is also used in the clinic, it meant that the provider seeing the patient in the clinic would have a complete explanation of what was done to and for the patient in the hospital. The reconciled medication list done on admission to the hospital, on discharge from the hospital, at the time of the care coaching call and at the follow-up visit in the clinic is the same in all four.
- In order to manage transitions of care and to audit the process, SETMA created the Inpatient Medical Record Census (IMRC). This is an electronic documentation of when and where a patient is admitted, when the history and physician is completed, when the Hospital Care Summary and Post Hospital Plan of Care is completed and questions posted by SETMA’s Central Business Office about hospital charges.
Hospital Care Summary And Post Hospital Plan of Care and Treatment Plan Tutorial
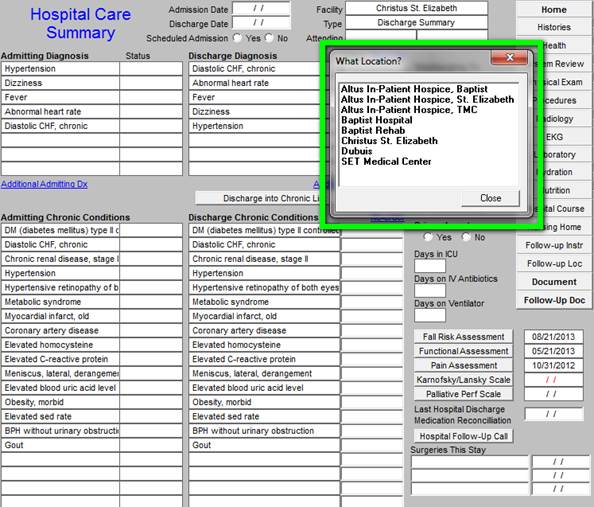
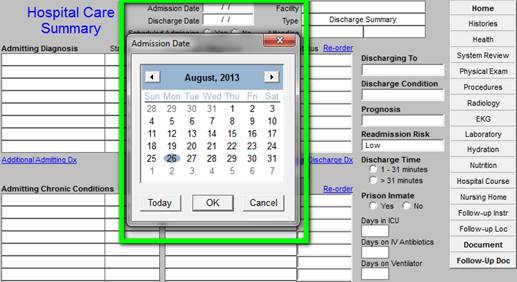
As the Hospital Care Summary is first accessed, a pop up will display to allow you to select a hospital location where the care was given. See below outline in Green.
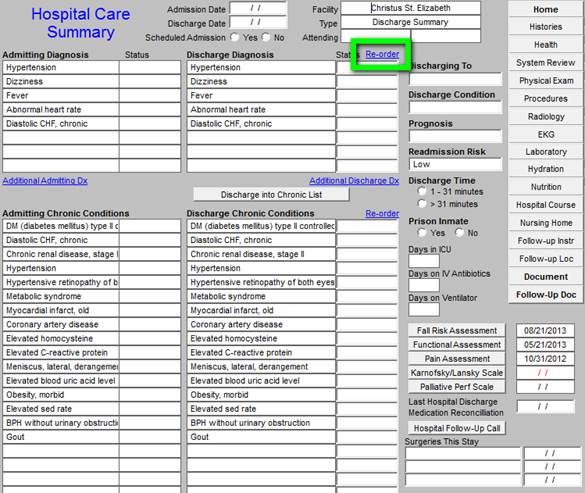
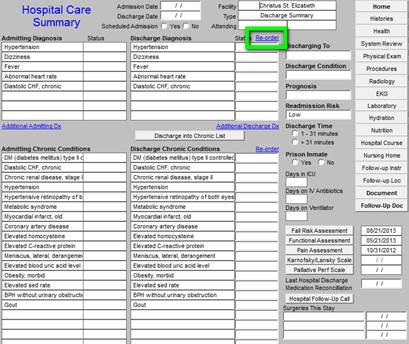
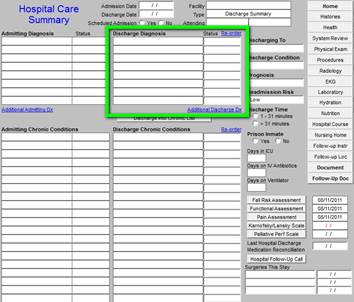
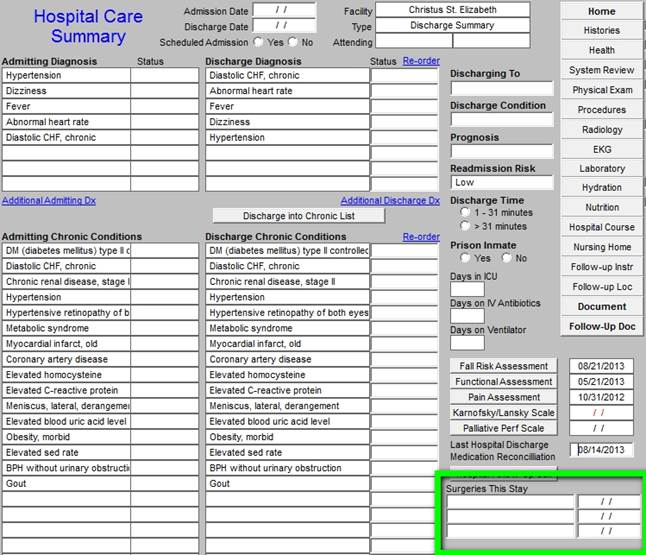
You will notice that the Hospital Care Summary Master Template shows the admission diagnoses and the discharge diagnoses. The order and the content of the discharge diagnoses can be changed. See below the button entitled “re-order” which is outlined in “green.”
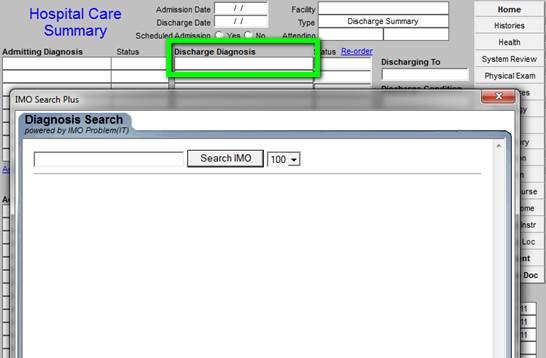
You can change the Discharge Diagnoses and/or their status, but the admission diagnoses cannot be changed. However, if you do not go through the steps descried below (see Page 40), this functionality will not work properly.
To change the discharges diagnoses, you click in the boxes under Discharge Diagnosis. When that is done, the list of ICD-9 Codes in the IMO software package will appear. You can then select new diagnoses which were discovered during the hospitalization.
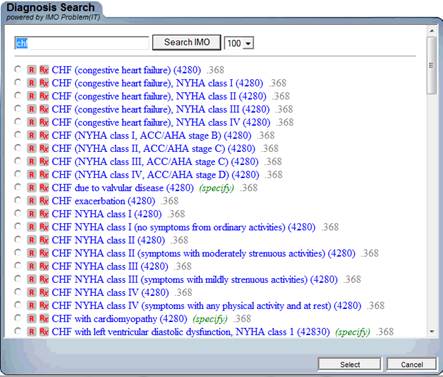
When an abbreviation or the first several letter of a diagnosis’ name is typed in the box next to “Search IMO” above, the list of relevant ICD-9 codes will appear. The box to the left of the desired diagnosis is checked and then the button entitled “select” is depressed.
Because the admission diagnoses will often be different from the discharge diagnoses and because the principle diagnosis which resulted in the hospitalization should be listed first, and because the co-morbidities which resulted in the hospital admission should be listed next, there is a “re-order” button which allows the provider to easily changed the order in which the diagnoses are listed. The following is a link to the full explanation of how to “re-order” a diagnoses list: The ability to re-order the Chronic Problem List with the most important diagnoses at the top.
When you click the “re-order” button, the following template will appear.
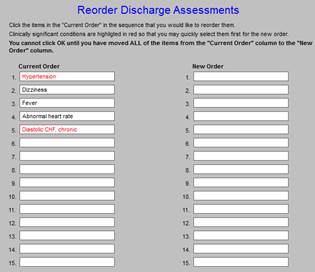
By clicking each of the diagnoses in the new order in which you wish for them to appear, they will appear in the right hand column as they will appear on the Hospital Care Summary Discharge Assessment.
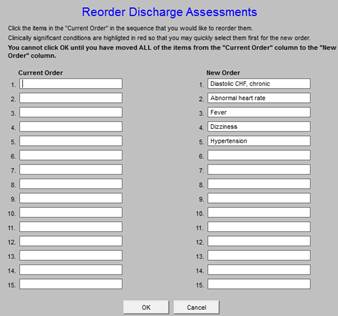
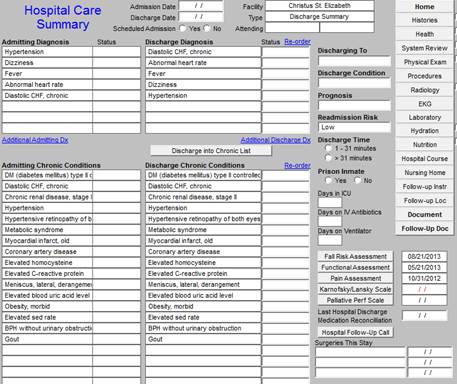
When the “OK” button is clicked, the re-ordered Acute Discharge list will appear as below.
- Admission Date -- this date must be manually entered into the template. It is imperative that the dates be correct on the hospital care summary.
- Discharge Date - this date must be manually entered into the template. It is imperative that the dates be correct on the hospital care summary.
Down the left hand column (see the green outlined box) are listed the Admitting Diagnoses and the patient’s chronic conditions. These cannot be changed on the discharge summary.
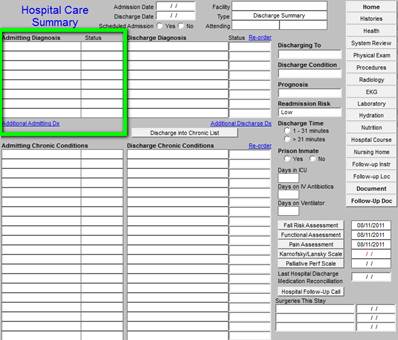
Next to this are the Discharge Diagnoses and the patient’s chronic conditions. These can be changed. In this way, the admission diagnoses will reflect the clinician’s impression on admission and the discharge diagnoses will reflect the clinician’s conclusions after the patient’s hospital evaluation and treatment are completed.
The Column next to the discharge diagnose has the following parts:
- Discharge to - there is a pop-up with the options: deceased or stable. At the following link, it is shown that there are eight different places to where the patient can be discharged. http://jameslhollymd.com/your-life-your-health/patient-centered-medical-home-and-care-transitions-part-i
- Discharge Condition -- there is a pop-up with the options: Good, Poor, and Terminal.
- Prognosis
- Readmission Risk - this is the assessment of the risk of the patient being readmitted. Currently, the formulae SETMA uses to calculate readmission probability is:
- Admitted 2 or more times in the last year = high risk
- Admitted 1 times in the last year = medium risk
- Admitted 0 times in the last year = low risk
- Discharge Time - 1-31 minutes -- >31 minutes
- Prison Inmate - yes or no
- Days in ICU
- Days on IV Antibiotics
- Days on Ventilator
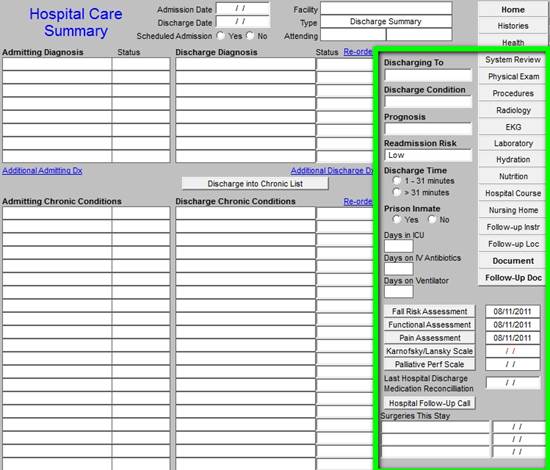
The next assessment which is critical in this transition of care document is the Fall Risk Assessment. Because patients leaving the hospital are often in a weakened or frail condition, they have an increased susceptibility to falls. The complete of the fall risk assessment is critical to patient safety and to the reduction of preventable readmissions.
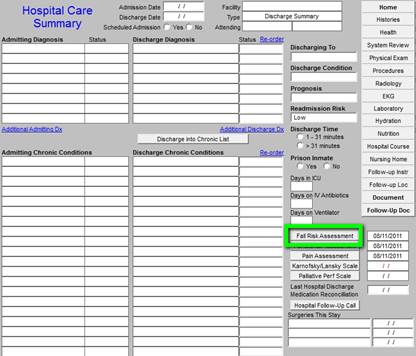
When depressed the Fall Risk Assessment button deploys the following template:
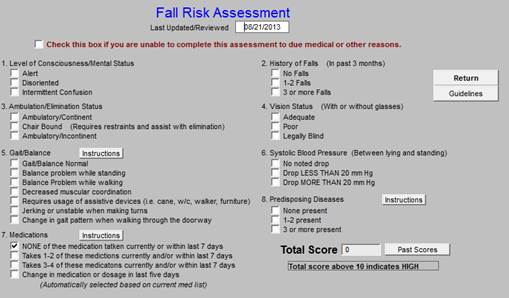
When complete the assessment will identify the potential for falls and will allow the provider to give a proactive plan to decrease fall risk.
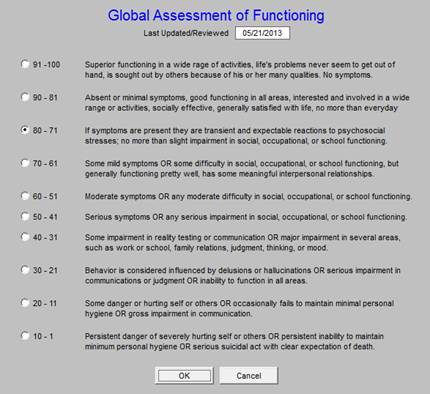
The next button is the Functional Assessment which is key to transitions of care planning for patient safety and decreasing readmissions.
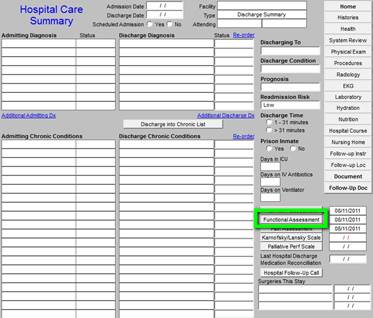
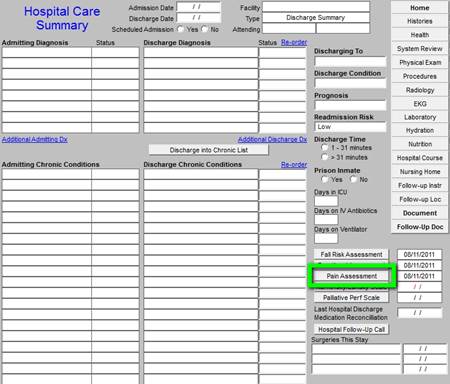
If a patient is sent home with unaddressed pain concerns, they will often return to the emergency room and be readmitted. The depression of the Pain Assessment button deploys a tool which allows the provider to document the patient’s pain status at discharge and encourages the addressing of pain before discharge.

The following link discusses the questionnaires and tools in greater detail and discloses their evidence-based source. http://jameslhollymd.com/epm-tools/Patient-Centered-Medical-Home-Annual-Questionaires.
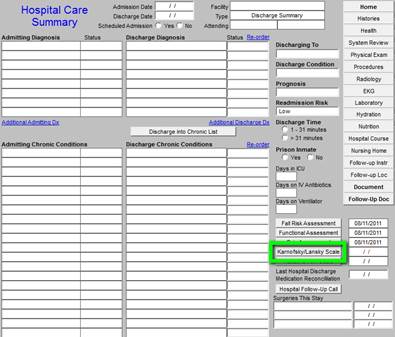
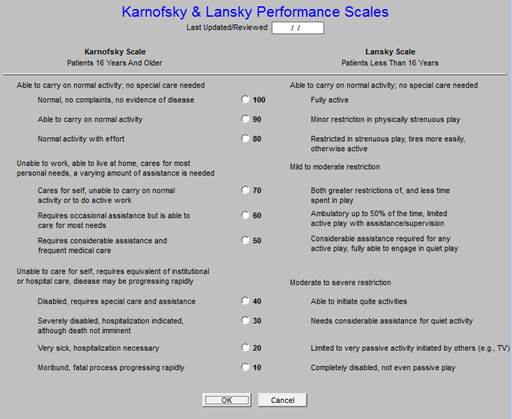
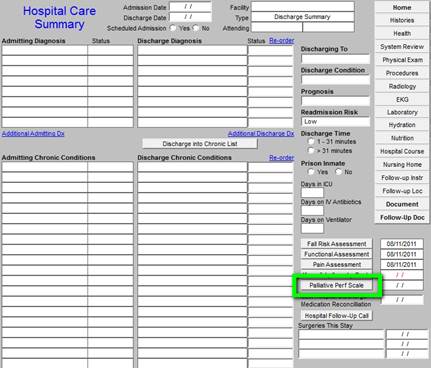
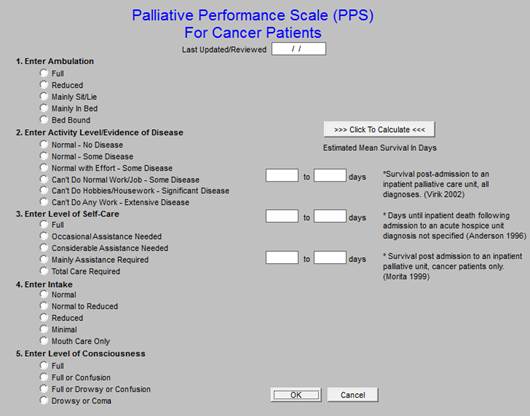
The following two buttons deploy questionnaires which are helpful in assessing of patients who are eligible for hospice or palatine care. One of the most effective ways of helping patients remain at home is by referring them to hospice when appropriate. These tools help in that process.
Most recent reconciliation is documented for the audit. This link is to an article which address medication reconciliation: http://jameslhollymd.com/Your-Life-Your-Health/Medical-Home-Series-Two-Part-XIV-Medication-Reconciliation
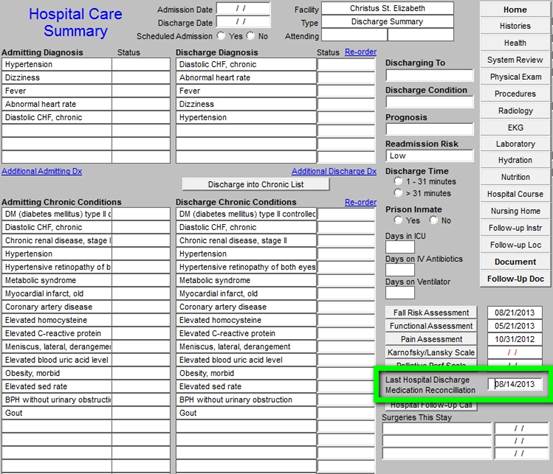
The next documentation is the Post Hospital Care Coaching Follow-up call. When the button outlined in green below is depressed the follow-up call template is opened so that the call can be scheduled. The following link is to an article about hospital and clinic follow-up calls: http://jameslhollymd.com/epm-tools/Tutorial-Hospital-Follow-up-Call
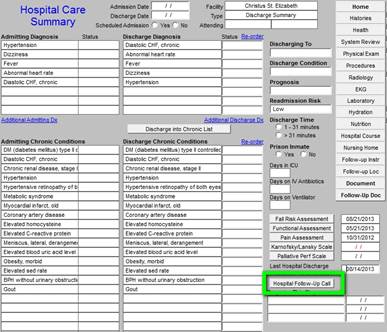
When this button is depressed, the following template is opened.
Finally, the last element in this column is a listing of the surgeries done in this admission.
The Care Transition Audit is SETMA’s adaptation of the Physician Consortium for Performance Improvement Data Set for Transitions of Care. SETMA has been auditing this data set since it was first published in June, 2009. The following is a link to a tutorial on this material: http://jameslhollymd.com/epm-tools/Tutorial-Care-Transition. SETMA has publicly reported by provider name on SETMA’s performance on this data set since 2009. The following is a link to the 2013 results of this audit. http://jameslhollymd.com/public-reporting/reports/2013/SETMA.com-2013-Care-Transition-Audit.pdf The following is a link to a series of articles on Care Transitions: http://jameslhollymd.com/your-life-your-health/care-transitions.
The button outlined in green below deploys the Care Transition audit on each patient discharged from the hospital.

The following is what is deployed with the Care Transitions button is depressed:
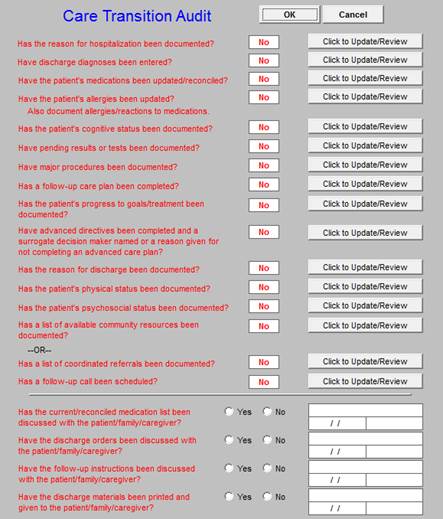
When the Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan has been completed, any incomplete elements of the audit will be in red. Any element in red can be completed by depressing the button “click to update/review.” Depressing the button will take the provider to the place in the chart where that element should be completed.
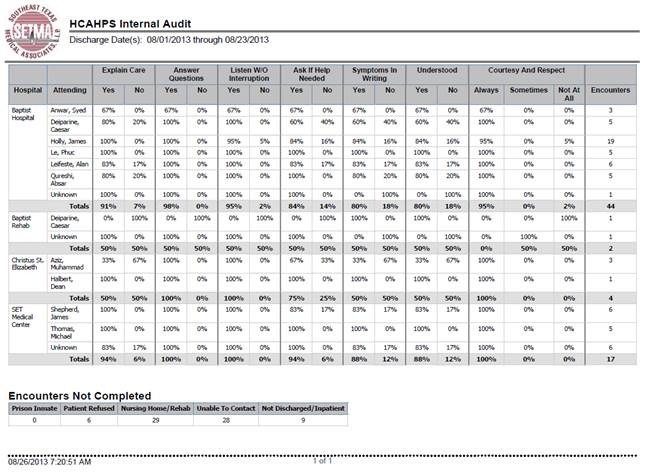
This is an assessment of patient satisfaction with t he care they received in the hospital. There are elements which relate to healthcare providers and elements which related to the hospital. In order for SETMA providers to improve their performance on these measures, they have been deployed in the EMR. In the Care Coaching Call after being discharged from the hospital, these questions are included. Further more a COGNOS audit has been created. In January, 2014, SETMA is going to begin publicly reporting these results by provider name.
The following is a link to a complete tutorial on HCAHPS: http://jameslhollymd.com/epm-tools/SETMAs-Internal-HCAHPS-Survey-Tutorial. When the button entitled “Post Hospital Patient Audit” outlined in green below is deployed, the HCAHPS template appears.
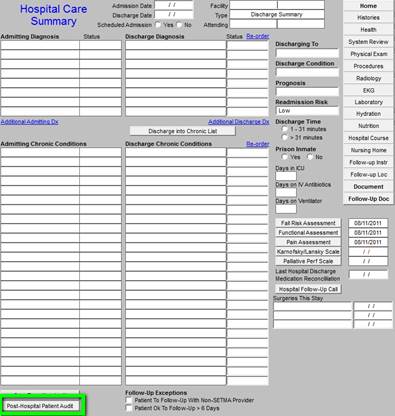
The following are the questions which are asked by SETMA Department of Care Coordination during the Care Coaching call the day after discharge from the hospital.
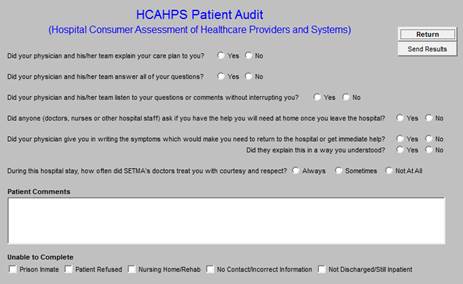
Once a month, SETMA completes the HCAHPS Internal Survey audit and distributes the following report to all SETMA Providers. In January, 2014, this audit will be displayed publicly on SETMA’s website.
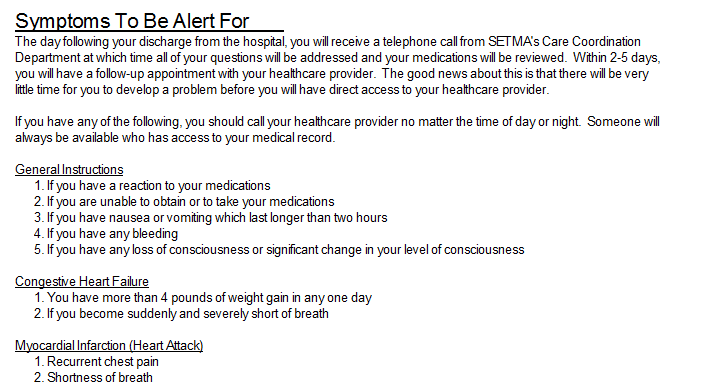
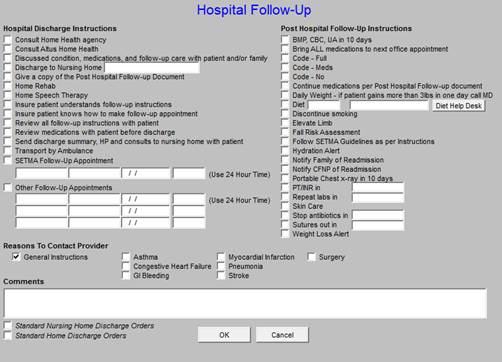
On the “Follow-up” page in this tutorial (page number _____), one of the most difficult of the HCAHPS’ survey is addressed. Below outlined in green are eight sets of “Reasons to Contact Provider.” This is given to the patient, in the Hospital Care Summary and Post Hospital Plan of Care document. It tells the patient in simple terms what symptoms should cause them to seek immediate attention either from their healthcare provider or by returning to the hospital.
When this document is being completed, the “General” symptoms is automatically completed for all patients and the specific condition such as pneumonia, CHF, etc., are completed for patients who have those conditions.

The following are examples of what will appear on the Hospital Care Summary and Post Hospital Plan of Care and Treatment plan which will meet and exceed the questions in the HCAHPS survey.
On the right hand side of the Master Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan Template, there are 15 navigation buttons on the Hospital Care Summary Template.
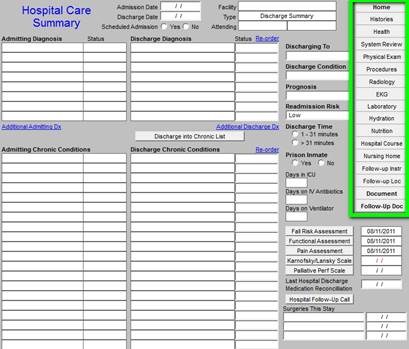
Six of the first seven buttons launched templates which are identical to templates on the Master GP Templates, they are:
- Histories
- Health
- System Review
- Physical Exam
- Radiology
- EKG
The fifth button entitled Procedures launches a template which enables the documentation of the procedures and studies done in the hospital.
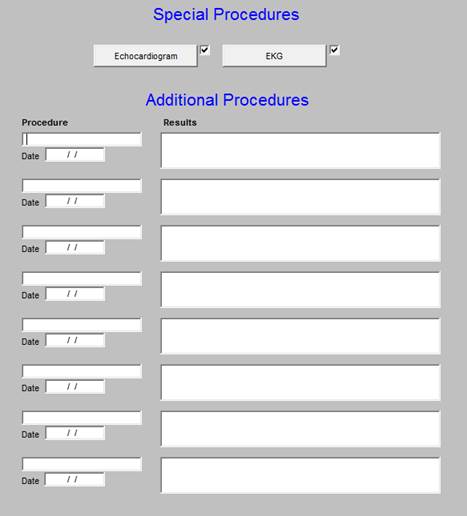
By clicking in the box entitled Procedure, you will see the pop-up as below.
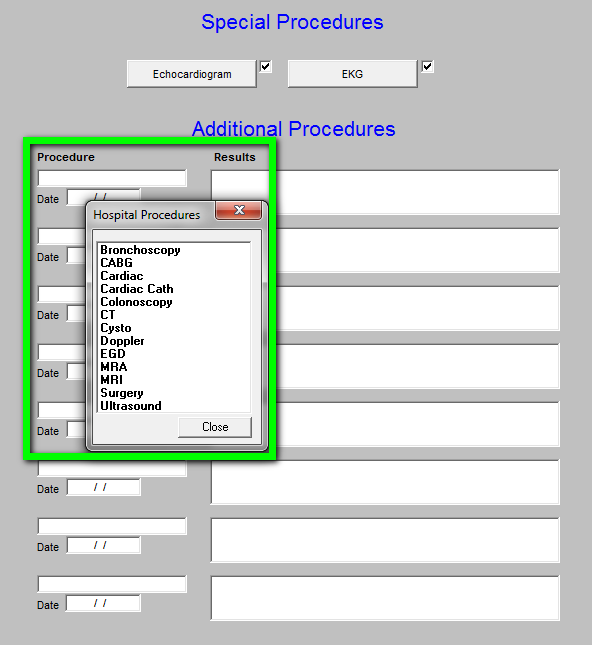
At the top of this template which is entitled Special Procedures are two buttons, which launch pop-ups with which to document special studies:
Echocardiogram
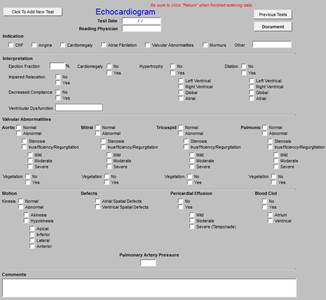
Electrocardiogram

One of the significant advances in quality and cost of healthcare is our ability to document laboratory values done in the hospital. The following tool allows those values to be entered into our EMR such those lab values interact with all quality metrics. This prevents us from having to repeat the testing done in hospital.
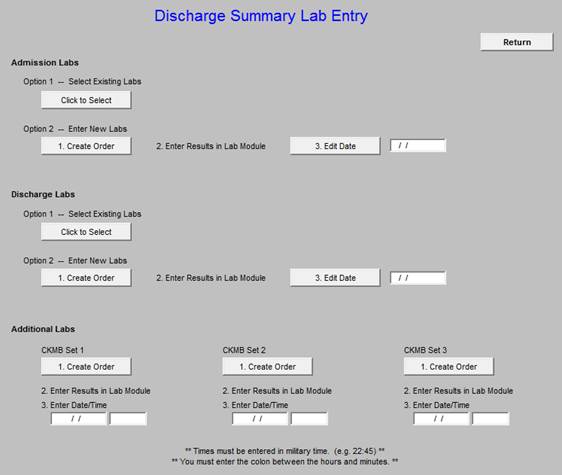
This allows the documentation of:
| Arterial Blood Gases | CBC |
| CMP | CPK/Troponins |
| Cultures | Drug Levels |
| UA | PT/INR |
| Lipids | Hemoglobin A1c |
| |
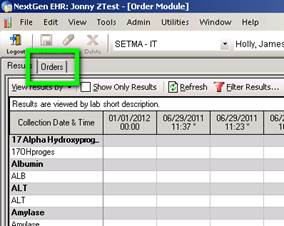
Just off to the right of the screen (scroll over) on the discharge summary, you will see a button named “New Lab Entry.” Click it and it will take you to this screen.
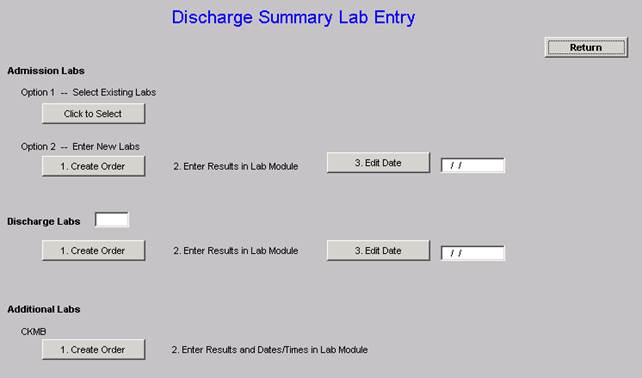
Under Admission Labs, Option 1 you can select labs that were previously entered using this method rather than re-entering the same set twice. For example, it would let you pick an old discharge set as the new admission set. However, since this only works with labs that have been entered this new way, you probably won’t be using it for a little while until we accumulate some of these.
Admission Labs, Option 2 and Discharge Labs work the same way. Click the Create Order button and it will take you to the lab module. When you get there, click Orders.
Next, find the order that you want to enter results for. If you are doing it for an admission, it will be “ZHospAdmit” and for a discharge it would be “ZHospDisch.” Select the correct order, the click the “Results (new results entry)” section and then the “New Results Entry” tab. Now, enter the results in the results column next to each descriptor. When you are done, click “Save” (there will be a few second freeze) and close the lab module.
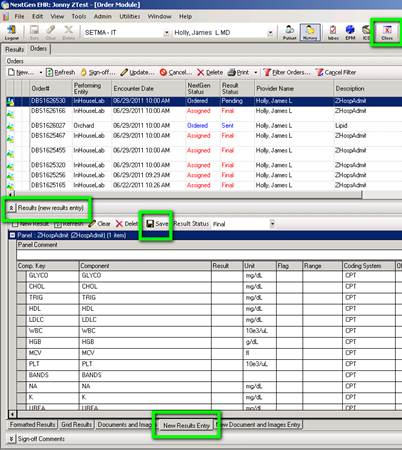
You will then return to the previous screen. Click the “3. Edit Date” button. You will get a calendar and you should select the date you want each of the results you just entered to have. When you select the date and click ok, it will update all of them with the date you selected.
The CKMB section operates the same way€¦except you have to enter the date/time manually when you enter the result. Just do everything else like you normally would.
The next two navigation buttons are:
- Hydration - for instructions on using this template see this LINK
- Nutrition - for instructions on using this template see this LINK The next Navigation button is Hospital
Course

This allows for detail to be documented about the patient’s hospital course and condition on discharge.
This opens a template which allows for specific instructions to be given for a patient who is being transferred back to the nursing home.
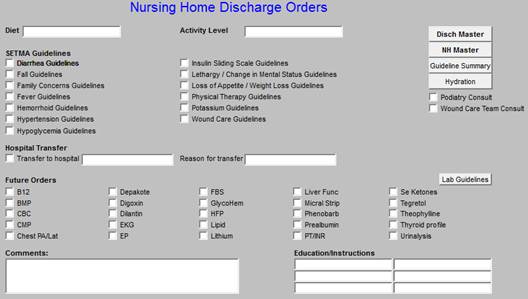
This is a list of instructions to the nursing home or family about follow-up. If the patient is going home the Standard Home Discharge Order buttons should be activated:
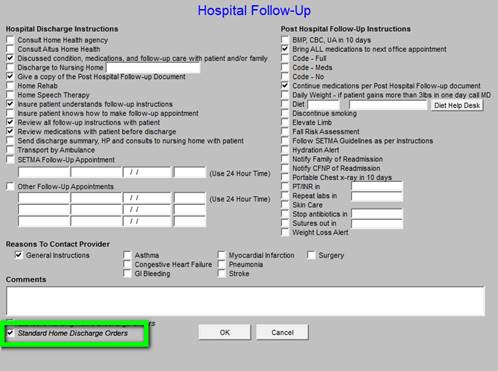
If going to the NH, Standard Nursing Home Discharge Orders should be activated.
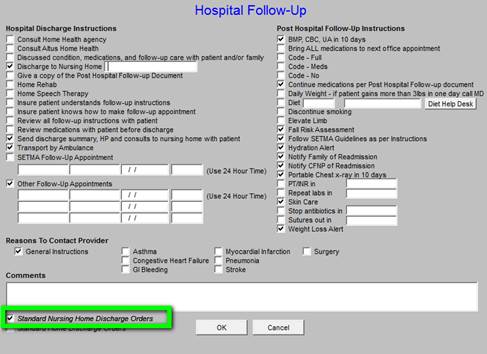
In either case, once the default orders are reviewed, other pertinent issues like “when to stop antibiotics,” “when sutures are to be removed,” etc., should be activated.

This launches a template with the names, addresses and telephone contact information for a number of clinics which are able to care for patients without insurance.
Document - this creates the Hospital Care Summary document for placing on the chart and for sending to the Nursing Home with the patient.
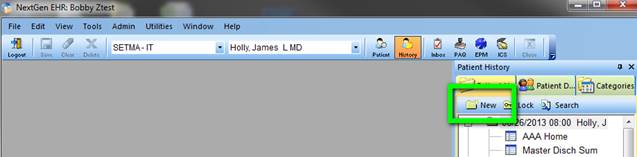
1. Open a visit for the date of discharge.
If you complete the hospital care summary discharge summary on the day you discharge the patient from the hospital, as you should, you do this simply by clicking on NEW on the Main Tool Bar.
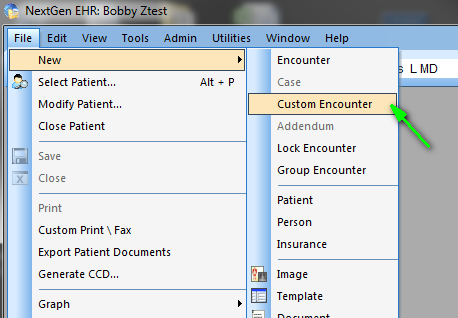
If you are completing a delinquent hospital care summary, you must create a Custom Visit so that the hospital care summary is filed on the date of discharge, even though it has been created on a different date, which date of document creation will be noted on the record.
You do this by going to the Left Top of the screen and clicking on FILE. You then click on NEW and then on CUSTOM VISIT.
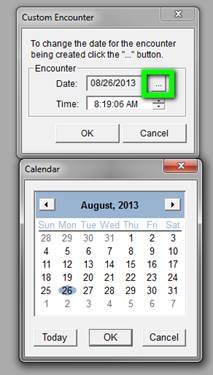
At this point, a Pop-Up entitled Custom Visit appears.
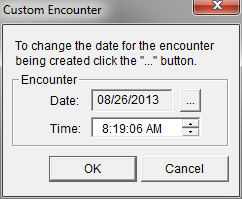
Beside the date on this Pop-up, there is a Button with three dots on it. If you click on that button, a calendar comes up which allows you to change the date to the date of the patient’s actual discharge. Once the date is correct, you click the OK button to the right top of the Pop Up. This creates a visit with the correct date.
2. At this point, your New Visit has nothing in it. In order to make the Hospital Care Summary work, you must follow these steps:
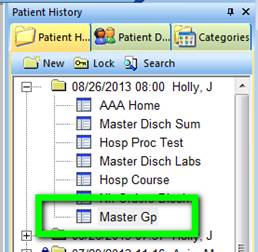
At the bottom of the Main Tool Bar, you will click on the top left icon which is the Template Icon. You will then select Master GP.
Double click on Master GP, or highlight it and the click on the OK button at the bottom of the Pop Up.
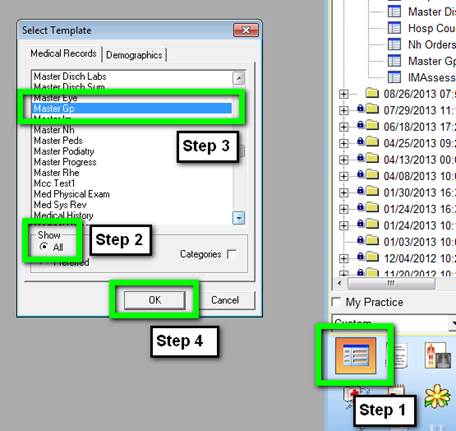
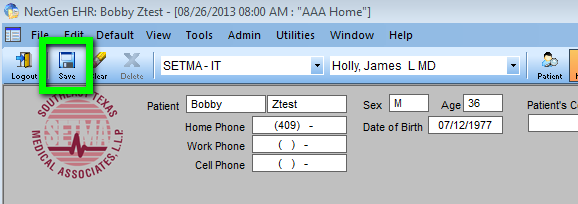
On the Top Tool Bar, the second icon is SAVE. You will click on this icon to save your change.
You will notice that Master GP now appears below the date of your custom visit, or your new visit at the right of your screen on the Main Tool Bar.
3. At this point, you will go back to the patient’s date of admission and find the Assessment under the date of admission.
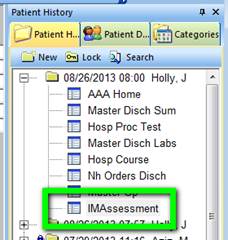
You will highlight Assessment by clicking on it. You will then hold the left mouse key down and DRAG the assessment up to your current visit - either a new visit if you are doing the discharge summary on time, or a custom visit if you are completing a delinquent hospital care summary.
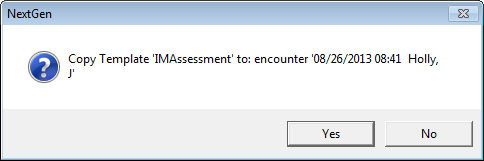
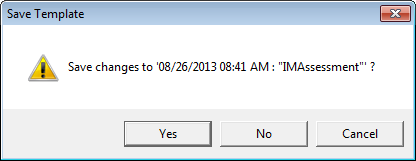
Once you have successfully dropped this assessment on the date of the new visit or the custom visit, a pop up will appear which asks you if you want to COPY and SAVE the assessment to this visit. You click yes.
You will notice now that your new or custom visit has both the Master GP and the Assessment listed under it.
At this point, go back to the Main Tool Bar and click on the top left hand icon for Templates. You will select the Master Hospital Care Summary one of three ways: You can return to AAA Home and select it.
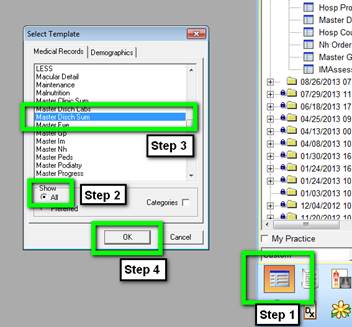
If the Master Hospital Care Summary has been placed in your preferences list, as the Master GP has, you will simply double click on Master Hospital Care Summary.
- The Post Hospital Plan of Care and Treatment Plan: Patient Engagement and Activation Document The following is a link to an example of this document: http://jameslhollymd.com/Presentations/pdfs/Post-Hospital-Plan-of-Care-and-Treatment-Plan.pdf
- The Post Hospital Plan of Care and Treatment Plan. This is link to a sample document: http://jameslhollymd.com/Presentations/pdfs/Example-of-SETMAs-Hospital-Care-Summary-and-Post-Hospital-Plan-of-Care-and-Treatment-Plan.pdf
To remind us of the constant need for change in healthcare transformation, we have archived a copy of the “old” version of our “discharge summary” tutorial. If you contrast the two, the progress we have made is remarkable, but more remarkable is the anticipation of the changes we will make over the next five years. The patient engagement and activation made possible by the functions detailed in this tutorial remind us of the constant change we will experience in the future. Sometimes the change is at lightening speed hardly leaving time for us to catch our breath. At other times the rate of change slows and allows us to incorporate all of the new ideas into our work flow. The key to the changes seen in this new tutorial is our clear understanding now of what it means for patients to be engaged, to be activated and to participate in shared decision making. Because this was the focus of our August, 2013 Provider training meeting, the following details the content of that session. We hope that it helps all who read this to incorporate these ideas into their practices and professional lives.
Today, August 20, 2013, we have our monthly provider training meeting. We close our offices for half a day. The subjects we will address today are:
- HCAHPS - reviewed as a patient-centric approach in in-patient care. link to the develop process of this audit and project - began July 15th Completed July 30th -- http://jameslhollymd.com/letters/
- CAHPS - we will review the questions which our CAHPS vendor will use.
- “Have You Really Addressed Your Patient’s Concerns,” Carlos Roberto Jaen - a Patient-Centered Office Visit - How? The following is the link to the power point for this part of the meeting today: http://jameslhollymd.com/Presentations/What-is-patient-centered-communication
- “Patient Engagement” Health Affairs, February 14, 2013 - How to promote patient engagement - http://jameslhollymd.com/Presentations/SETMA-8-20-13-Provider-Training-Health-Affairs-2-14-13-Patient-Engagement
- Health Affairs, Health Gaps, August 15, 2013. - SETMA has eliminated ethnic disparities in hypertension and diabetes - this is a broader view http://jameslhollymd.com/Presentations/SETMA-8-20-13-Provider-Training-Health-Affairs-8-15-13-Health-Gap.
- SETMA’s Automated Team, the logical extension of Clinical Decision Support, Patient Engagement, Activation and Shared Decision Making. The following is the link to our Automatic Team Tutorial: http://jameslhollymd.com/epm-tools/Automated-Team-Tutorial-for-the-EMR-Automated-Team-Function
|