|
Increasingly, health plans and particularly Federal programs are requiring evidence of quality performance with reimbursement tied to that evidence. In 2007, the Institute for Healthcare Improvement (IHI) enunciated The Triple Aim for the future of healthcare which is: improved health, improved care, lower cost. The IHI identified “integrators” of health as the organizations which would move healthcare in the direction and to the destination, we need to go. Three of those “integrators” are:
- Medicare Advantage
- Medical Home
- Accountable Care Organizations
Each of those “integrators” have a defined set of quality measures which are required in order to participate and in order to receive the maximum reimbursement.
- Medicare Advantage - Stars Program - 53 Quality Metrics
- Medical Home - National Quality Forum endorsed measures - 10 required by NCQA
- Accountable Care Organizations - 33 define quality metrics
There is significant overlap to these requirements. Because SETMA reports on numerous quality measures and groups of measures - NCQA, PCPI, AQA, HEDIS, NQF, Guidelines Advantage, Core Measures (Hospital), Bridges to Excellence, PQRS, Joslin, SETMA Developed Measurement SETS and STARS, ACO measurements - we are preparing a spreadsheet which will show how many measurement sets each metric appears in. The ideal will be for a single measurement set be developed. The only limitation to that ideal is there are legitimate cases where a metric is relevant to one entity and not to another.
SETMA’s deployment of the STARs measures is to insure that the Golden Triangle Physicians Alliance (GTPA), a qualified Independent Physician Association (IPA), achieves a 5-Star rating. Because the provider-performance-dependent metrics are HEDIS measures and because SETMA has been tracking and auditing HEDIS performance for five years, the Stars program is nothing new to us. In fact, SETMA’s HEDIS results, by provider name, are reported on our website at www.jameslhollymd.com under Public Reporting.
We do believe that the specific attention to the Stars subset of HEDIS measures will enable us to know more precisely where our performance falls short and to address improvement strategies. Always remember, any information required to determine if the patient is eligible for a metric and any determination if they are adherent is automatically aggregated.
(The following excerpt is from a “Data Brief” is from the Medicare Advantage Plan Star Ratings supported by the Henry Kaiser Family Foundation.)
For several years, the Centers for Medicare and Medicaid Services (CMS) has posted quality ratings of Medicare Advantage plans to provide Medicare beneficiaries with additional information about plans offered in their area. All Medicare Advantage plans are rated on a 1 to 5 star scale, with 1 star representing poor performance, 3 stars representing average performance, and 5 stars representing excellent performance. The quality scores for Medicare Advantage plans in 2011 are based on 53 performance measures that are derived from plan and beneficiary information collected in three surveys - HEDIS, CAHPS, and HOS - and administrative data. For example, the performance measures include whether the plans’ enrollees received the appropriate screening tests, the number of complaints CMS received about the plan, and how enrollees rated the communication skills of the plans’ physicians. CMS assigns quality ratings at the contract level, rather than for each individual plan. This means that every Medicare Advantage plan covered under the same contract receives the same quality rating (and most contracts cover multiple plans).
In 2012, Medicare Advantage plans will begin to receive bonus payments based on quality ratings. These payments were initially established in the 2010 health reform law that provides for bonus payments to plans that receive 4 or more stars and to unrated plans beginning in 2012. In addition to the bonus payments established by the health reform law, CMS will also be launching a 3-year demonstration to begin in 2012 that increases the size of bonuses for these plans, and also provides bonuses to plans rated as average (receiving 3 or 3.5 stars), using the same 1 to 5 star scale. The demonstration, according to CMS, aims to encourage “plans to improve performance at various star rating levels” and to test “whether providing scaled bonuses will lead to more rapid and larger year-to-year quality improvements in Medicare Advantage program quality scores,” compared to the bonus structure under the health reform law. Proponents say the demonstration will encourage plans at various star ratings to improve or maintain their quality ratings, while others question the appropriateness of providing bonuses to plans with average ratings, and the costs associated with the demonstration.
Star Ratings. CMS rates Medicare Advantage plans on a scale of one to five stars, with five stars representing the highest quality. The CMS defines the star ratings in the following manner:
5 Stars |
Excellent Performance |
4 Stars |
Above Average Performance |
3 Stars |
Average Performance |
2 Stars |
Below Average Performance |
1 Star |
Poor Performance |
All Health Maintenance Organizations (HMOs), Point of Service (POS) plans, local Preferred Provider Organizations (PPOs), regional PPOs, and Private Fee-for-Service (PFFS) plans are eligible for bonus payments, and are rated by CMS unless they are too new or have too few enrollees. The star ratings are derived from four sources of data: 1) CMS administrative data on plan quality and member satisfaction; 2) the Consumer Assessment of Healthcare Providers and Systems (CAHPS®); 3) the Healthcare Effectiveness Data and Information Set (HEDIS®); and 4) the Health Outcomes Survey (HOS). CMS groups the individual quality measures for the 2011 stars into the following nine domains:
| Domain |
Number of Measures |
Staying healthy: screenings, tests, and vaccines |
13 |
Managing chronic (long term) conditions |
10 |
Drug plan customer service |
7 |
Ratings of health plan responsiveness and care |
6 |
Health plan member complaints, appeals |
4 |
Drug pricing and patient safety |
4 |
Health plan telephone customer service |
3 |
Drug plan member complaints, members who choose to leave, and Medicare audit findings |
3 |
Member experience with drug plan |
3 |
SETMA’s Tutorial for Using the EMR’s STARs Deployment
As with all of SETMA’s tracking of quality metrics, one patient at a time, their fulfillment is aggregated incidental to care. The object of patient care is not the fulfillment of quality metrics; it is “better care, better health and lower cost.” But, like a Global Positioning System (GPS), quality metrics can tell you where you are, where you want to go and how to get there. But, also like a GPS, the object of the trip is not simply to know the points along the way. The object is to safely, securely and successfully to reach the goal.
SETMA’s STARS deployment can be found on the AAA Home template by clicking on the button entitled “STARS Program Measures,” which is outlined in green below.
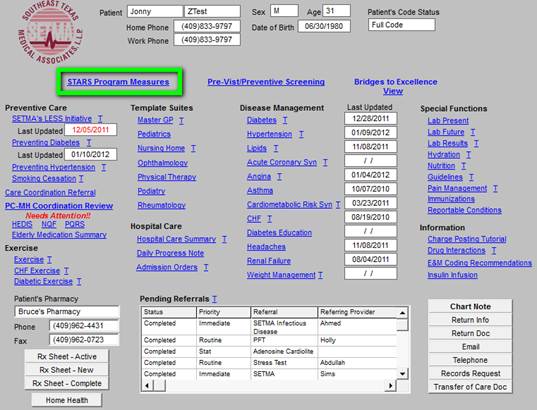
The button outlined in green above launches the Medical Advantage 2012 STARS Program template as seen below. The legend reminds SETMA’s providers that all measures which apply to the current patient and that have been met are in black; all which apply and have not been met are in red and all that do not apply are in gray.

|