|
2009 Introduction to SETMA’s Care Transition Tutorial
In June, 2009,the Physician Consortium for Performance Improvement, which in part includes the American Board of Internal Medicine Foundation, American College of Physicians, Society of Hospital Medicine and the AMA Physician Consortium, published Care Transitions: Performance Measurement Set entitled Phase I: Inpatient Discharges and Emergency Department Discharges.
Since 2003, SETMA has utilized NextGen EMR in the in-patient setting in order to complete Admission History and Physician examinations and Discharge Summaries (renamed Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan in 2010) for the patients whose care we manage. SETMA has also designed and used a Daily Progress Note in our EMR. That project was suspended until we get an interface built between the hospital and NextGen so that daily vital signs and patient-condition data, laboratory values and medications can be automatically posted to our EM. We hope that will be accomplished with the deployment of our Health Information Exchange (HIE).
After reviewing the content of the Care Transitions Measurement Set, it was apparent that with a few modifications which have been made, SETMA performs all of the elements of this set. We believe that the auditing of this performance measure by the provider at the point of service will improve that quality of care given to patients transitioning from inpatient or ER to another place of care. The following links are discussions posted on SETMA’s website about the complexities of care transitions.
SETMA's Inpatient Team Based Process Analysis: The Interaction of SETMA’s Hospital Care Team - Collegiality and "Electronic Huddles"
SETMA’s Care Coordination and Transitions of Care: Part I
A Care System for Effecting Reductions in Preventable Readmission Rates
CMMI Care Innovation Summit, Washington, D.C. January 26, 2012: Observations of an Attendee
Medical Home Series Two: Part VI Care Transitions
Patient-Centered Medical Home and Care Transitions: Part II
Patient-Centered Medical Home and Care Transitions: Part I
Reducing Preventable Readmissions to the Hospital
Concierge Medicine and the Future of Healthcare
Patient-Centered Medical Home - Care Coordination and Coordinated Care
SETMA and the National Quality Forum
The Future of Healthcare - SETMA's View
Passing the Baton: Effective Transitions in Healthcare Delivery
In addition, the method SETMA has developed to make the elements automatically interactive with the patient’s care streamlines this process and makes it easy.
This Tutorial explains SETMA’s deployment of this measurement set and how to use it. Currently, the Care Transition Data Set contains 18 elements. Fourteen or documentation elements and four are action elements. Please note that this is Phase I of the Care Transition Data Set; as this set evolves, SETMA will modify this deployment to reflect those upgrades.
The following are links to SETMA’s first 4.5 years of auditing of our use of the Care Transitions Data Set.
How to use SETMA’s Care Transition Audit
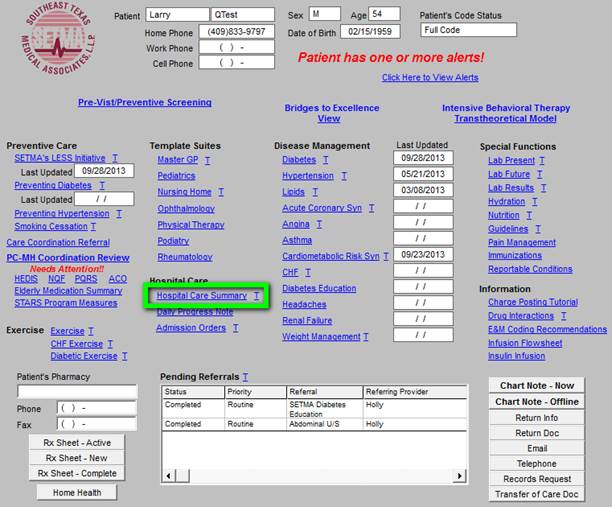
You will find the Care Transition Audit took by opening the AAA Home template

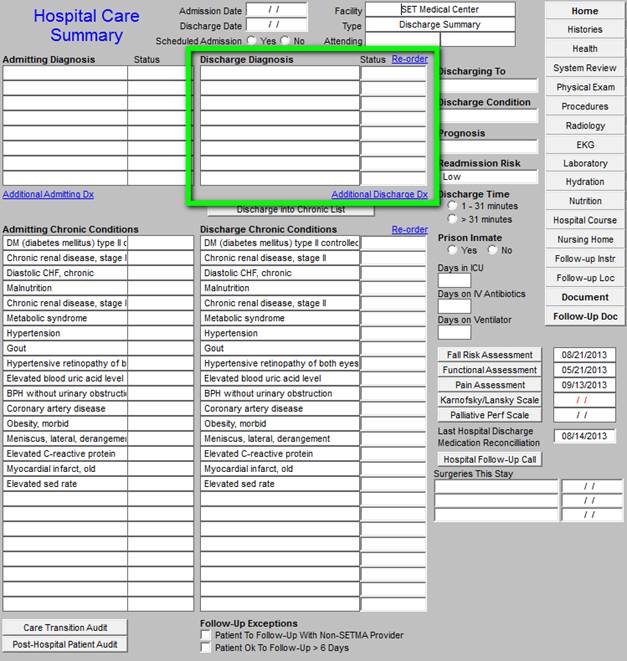
In previous iterations of this tool, the transitions audit was triggered off the Discharge Summary template. Now, however, the Discharge Summary has been renamed to Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan. The tutorial for that tool can be found at http://jameslhollymd.com/epm-tools/hospital-care-summary-and-post-hospital-plan-of-care-and-treatment-plan-tutorial. The Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan is triggered off the button entitled Hospital Care Summary which is outlined in green below.
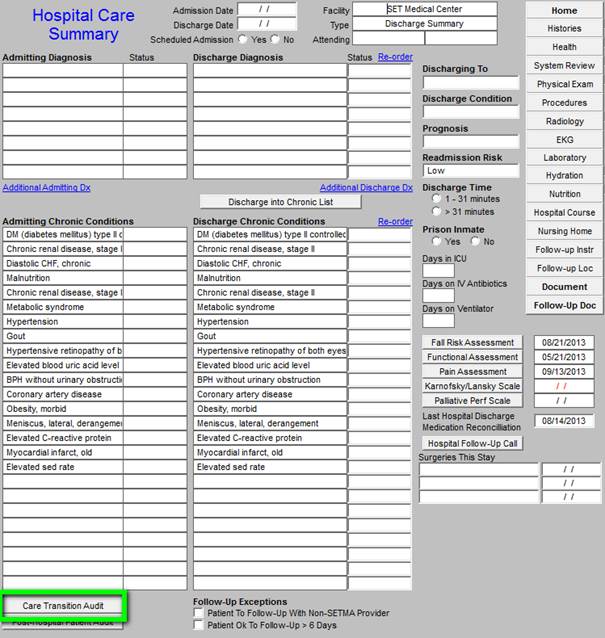
The Care Transition Audit button can be found at the bottom of the screen. Below it is outlined in green.
When that button is depressed, the following pop-up appears.

There are eighteen data points in the Care Transition Data Set. Fourteen are elements of documentation and four are actions which are to be taken. Once the discharge summary has been completed,
If the element has been met in the patient’s record, or if the action required has been taken, two things will appear:
1. The element will appear in black fonts
2. The box next to the element will contain a “Yes” which will be in black fonts.
If the documentation or action required for an element in the Care Transition has not been completed, two things will appear:
1. The element will appear in red fonts
2. The box next to the element will contain a “No” which will be in red fonts.
To the right of each of the first fourteen elements of the data set, there is a button entitled “Click to update/review.” When this button is depressed, it will automatically take you to the part of the discharge record which will allow you to document what is required but missing. In that the last four elements require an action, the documentation is completed by marking the “yes” or “no” radial button next to the element.
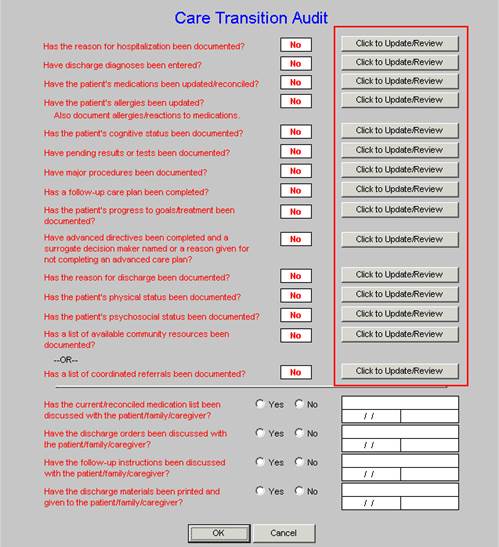
The eighteen elements are:
1. Has the reason for hospitalization been documented?”
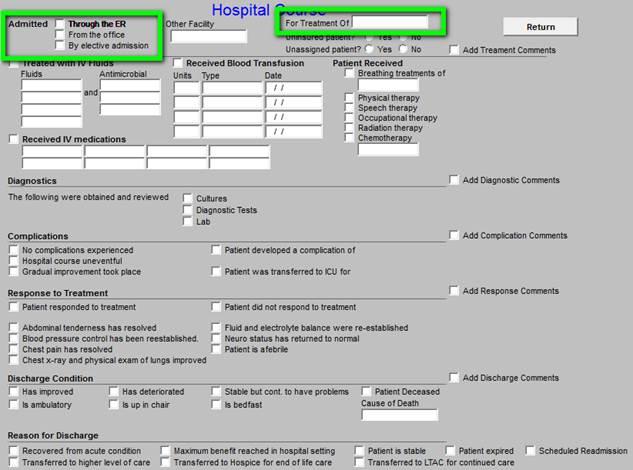
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the following template reason for hospitalization can be entered.
2. “Have Discharge Diagnoses been entered?”
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the following template where the discharge diagnoses can be entered.
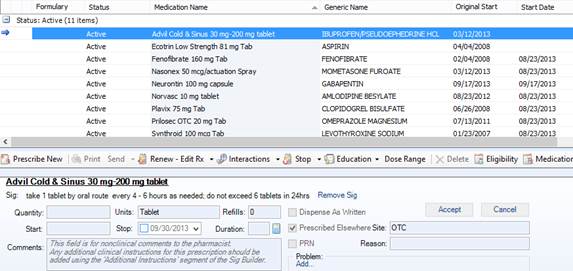
3. “Have the patient’s medications been updated/reconciled?
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the following template where the medications can be updated and/or reconciled.
During the hospitalization process, SETMA’s patients have four mediation reconciliations:
- Upon admission
- Upon discharge
- Care Coaching Call from SETMA’s Care Coordination Department the day after discharge
- Follow-up visit in clinic: within two days for high risk readmission and within five days for other others.
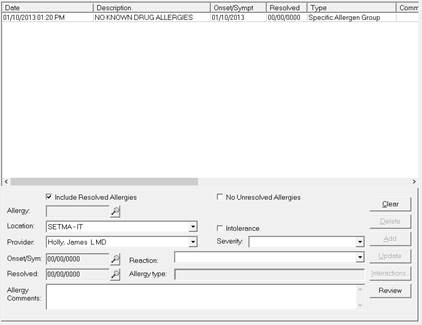
4. “Have the patient’s allergies been updated?” “Also, document allergies/reactions to medications.”
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the following template where the allergies can be reviewed, updated and where any adverse reactions which took place during the
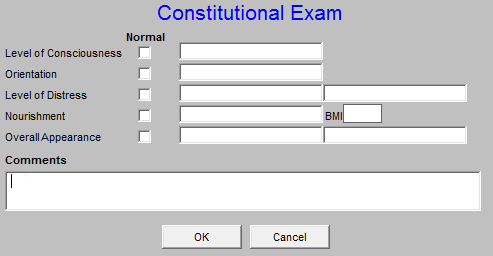
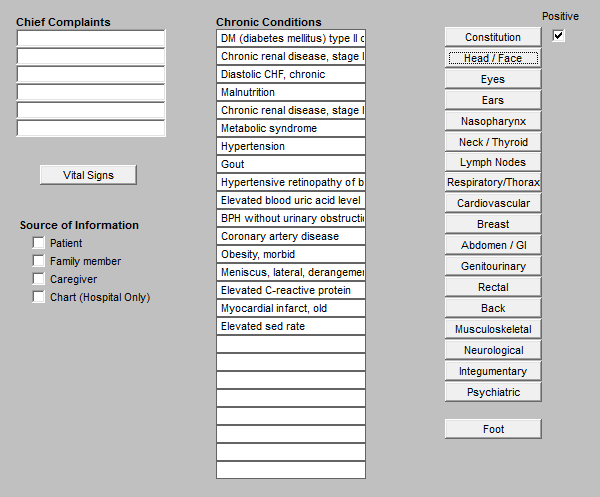
5. “Has the patient’s cognitive status been documented?”
If the box next to this element indicates that it has not been documented, in which case a red
“No” appears, depressing the “update/review” button displays the Constitutional template of the
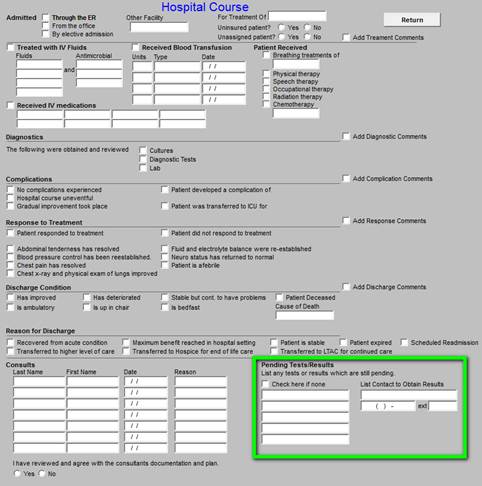
6. “Have pending results or test been documented?”
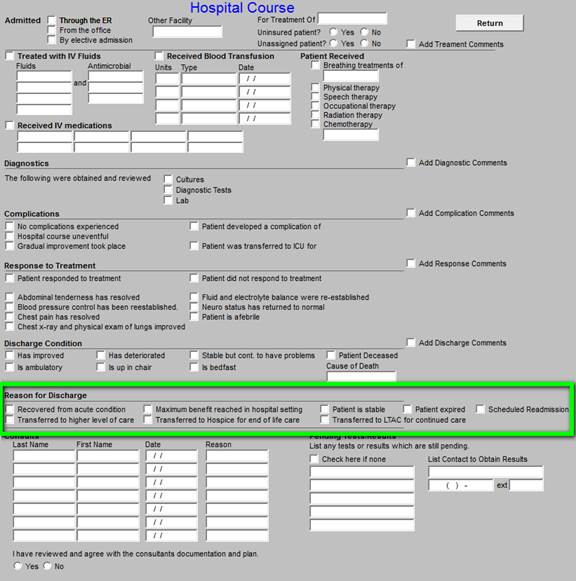
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the Hospital Course template where any pending or unreported tests can be denoted.
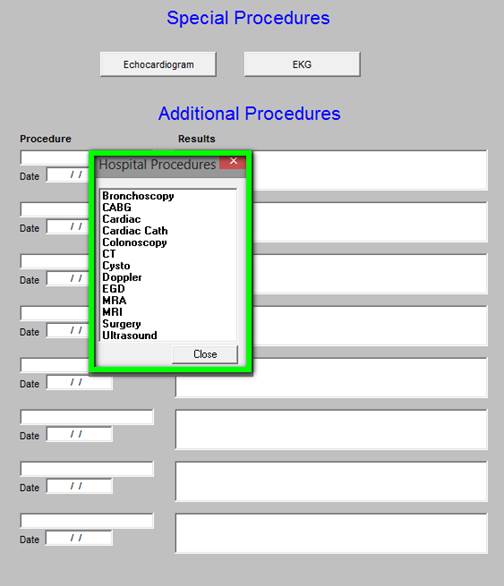
7. “Have major procedures been documented?”
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the Major Procedures template where the results can be entered.
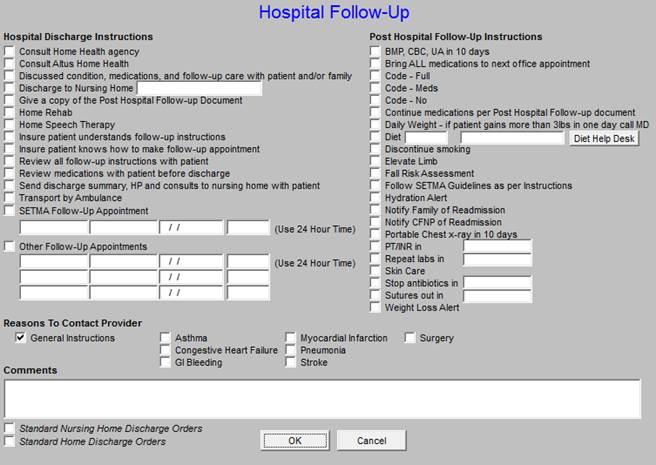
8. “Has a follow-up care plan been completed?”
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the Follow-up Plan template where the plan can be entered.
9. “Has the patient’s progress to goals/treatments been documented?”
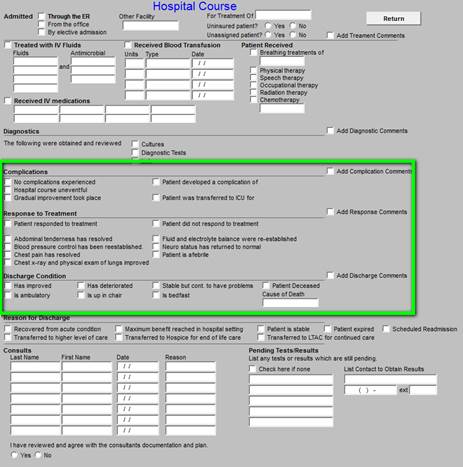
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the Hospital Course template where the progress to goals/treatments can be documented.
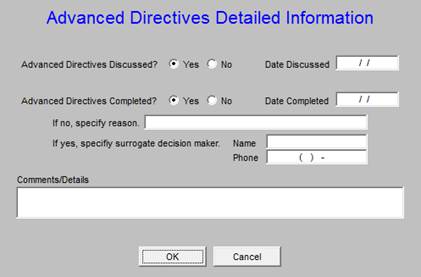
10. “Have advanced directives been completed and a surrogate decision maker selected or a reason given for not completing an advanced care plan?”
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the Advanced Directive Detail template.
11. “Has the reason for discharge been documented?”
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the Hospital Course Template where the reason for discharge can be documented in the section provided.
12. “Has the patient’s physical status been documented?”
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the Physical Examination section of the discharge summary.
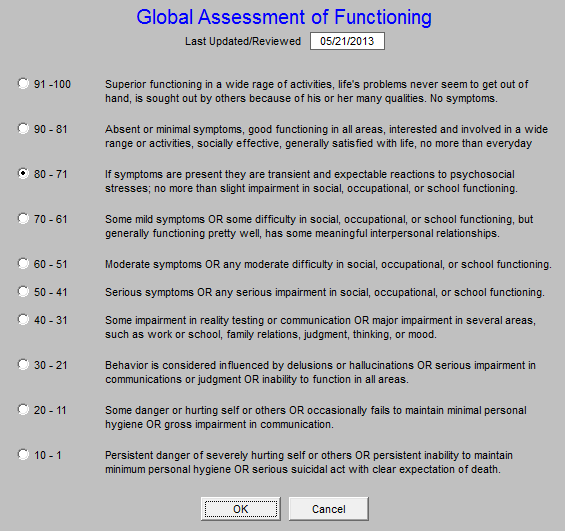
13. “Has the patient’s psychosocial condition been documented?”
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, depressing the “update/review” button displays the Functional Assessment template where the patient’s psychosocial condition can be documented.
14. “Has a list of available community resources and/or coordinated referrals been documented?”
If the box next to this element indicates that it has not been documented, in which case a red “No” appears, there are two options for fulfilling the element:
A. For those patients not being followed-up in a SETMA clinic depressing the “update/review” button displays Local Available Services template which will allow you to refer them to a local clinic.
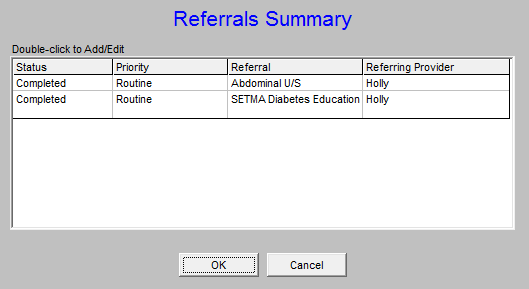
B. For those patients who are being followed by SETMA, you would simply complete any referrals which need to be done by utilizing the referral template function which is displayed on the Discharge Master

The last four elements are actions which need to be taken and simply requiring checking whether or not these four functions have taken place.
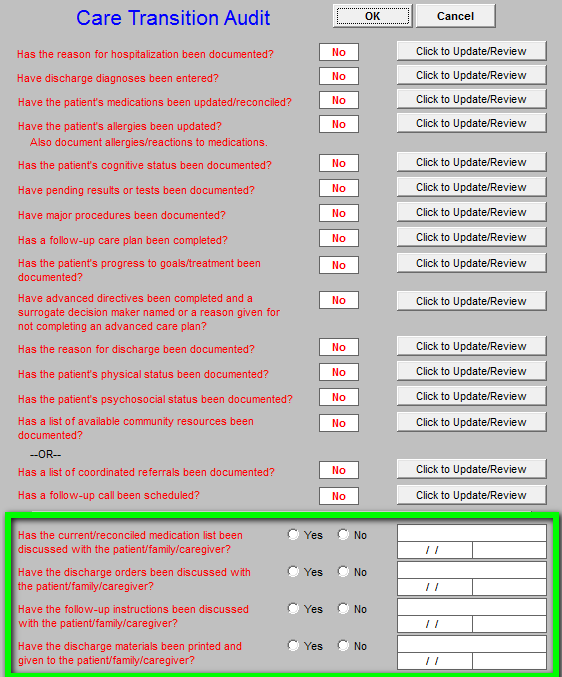
By checking each of these boxes the provider or his/her representation attests to the fact that:
- Medications have been discussed with patient.
- Discharge orders have been discussed with pateint.
- Follow-up instructions have been discussed wit the patient.
- Discharge materials have been printed and given to the patient/family/caregive.
Bewteen 2008 and 2013, SETMA has discharge 21,000 patients from the hopstial. Int hat time 98.7% of the time these tools have been given to the patient at the time they leave the hospital.
Note: In 2011, The AMA’s PCPI Department completed a research project on SETMA’s use of their Care Transitions Meawsurement Set. The conclusion of that project was the SETMA is using the set correctly and that our audit results are accurate.
|