Table of Contents
Because renal disease is so common in the population SETMA treats and because SETMA treats so many patients with diabetes, which is the most common cause of chronic renal failure and ESRD, and because it is possible effectively to delay the progression of chronic renal disease, SETMA has incorporated the National Kidney Foundation’s (NKF) treatment guidelines into our tutorial. The following introduction provides an overview of chronic kidney disease. The importance of this material is seen when you review the education piece which is found on the Evaluation Template under the heading entitled “Kidney Structure.” It states:
“The two kidneys each contain 1.0-1.3 million independent nephrons. Possibly one-third of
the nephrons could be lost to a chronic disease process or nephrotoxicity without a noticeable
reduction in the whole-kidney glomerular filtration rate. If the remaining two-thirds of the
nephrons hypertrophied so that the single nephron filtration rate increased by 50%, the whole-
kidney glomerular filtration rate would remain the same.
“As a result, the kidney can suffer considerable damage before losing sufficient function to
modify the normal clinical indicators of renal disease, such as the serum creatinine concentration.
Approximately 50% or more of renal capacity can be lost before serum creatinine levels become
abnormal and the disease is detectable clinically:”
It is our hope that the incorporation of the knowledge and treatment strategies identified by the NKF and presented here will improve the quality of care received by patients treated by SEMTA. The following “Clinical Review” is the work of the NKD.
Chronic Renal Disease - Clinical Review
Early identification and active management of patients with renal impairment in primary care can improve outcomes. The number of patients with end stage renal disease is growing worldwide. About 20-30 patients have some degree of renal dysfunction for each patient who needs renal replacement treatment. Diabetes and hypertension are the two most common causes of end stage renal disease and are associated with a high risk of death from cardiovascular disease.
Mortality in patients with end stage renal disease remains 10-20 times higher than that in the general population. The focus in recent years has thus shifted to optimizing the care of these patients during the phase of chronic kidney disease, before the onset of end stage renal disease. This review summarizes current knowledge about the various stages of chronic renal disease, the risk factors that lead to progression of disease, and their association with common cardiovascular risk factors. It also provides strategies for intervention at an early stage of the disease process, which can readily be implemented in primary care, to improve the overall morbidity and mortality associated with chronic renal disease.
Summary Points
- Significant renal dysfunction might be present even when serum creatinine is normal or only slightly abnormal
- Renal function declines progressively once creatinine clearance falls by about 25% of normal, but symptoms are often not apparent until renal failure is advanced
- The baseline rate of urinary protein excretion is the best single predictor of disease progression
- The prevalence of common cardiovascular risk factors is high in chronic renal disease; early identification and effective control of these risk factors is important to improve outcomes
- Cardiovascular disease accounts for 40% of all deaths in chronic renal disease
- Potentially reversible causes should be sought when renal function suddenly declines
- Irreversible but modifiable complications (anemia, cardiovascular disease, metabolic bone disease, malnutrition) begin early in the course of renal failure
Chronic renal failure is defined as either kidney damage or glomerular filtration rate less than 60 ml/min for three months or more. This is invariably a progressive process that results in end stage renal disease.
Serum creatinine is commonly used to estimate creatinine clearance but is a poor predictor of glomerular filtration rate, as it may be influenced in unpredictable ways by assay techniques, endogenous and exogenous substances, renal tubular handling of creatinine, and other factors (age, sex, body weight, muscle mass, diet, drugs). Glomerular filtration rate is the "gold standard" for determining kidney function, but its measurement remains cumbersome.
For practical purposes, calculated creatinine clearance is used as a correlate of glomerular filtration rate and is commonly estimated by using the Cockcroft-Gault formula or the recently described modification of diet in renal disease equation.
Methods for Estimating Creatinine Clearance (glomerular filtration rate) in ml/min/1.73 m2
- Cockcroft-Gault formula -- Creatinine Clearance = [(140-Age) x (Weight in kg)] / [0.8 x (Serum Creatinine in mg/dL)] x (0.85 if female)
- Modification of Diet in Renal Disease Equation -- Glomerular filtration rate=186.3×(serum creatinine) 1.154×age 0.203×(0.742 if female)×(1.21 if black)
Chronic Renal Disease
Chronic renal disease is divided into five stages on the basis of renal function. Pathogenesis of progression is complex and is beyond the scope of this review. However, renal disease often progresses by "common pathway" mechanisms, irrespective of the initiating insult. In animal models, a reduction in nephron mass exposes the remaining nephrons to adaptive hemodynamic changes that sustain renal function initially but are detrimental in the long term.
Stages of Renal Dysfunction
| Stage |
Description |
Creatinine Clearance
(GFR) (mL/min/1.73m2) |
Metabolic Consequences |
| 1 |
Normal or increased GFR - people at increased risk (box 2) or with early renal damage |
>90 |
|
2 |
Early renal insufficiency |
60-89 |
Concentration of parathyroid hormone starts to rise (GFR=60-80) |
3 |
Moderate renal failure (chronic renal failure) |
30-59 |
Decrease in calcium absorption (GFR<50)
Lipoprotein activity falls
Malnutrition
Onset of left ventricular hypertrophy
Onset of anemia (erythropoietin deficiency) |
4 |
Severe renal failure (pre-end stage renal disease) |
15-29 |
Triglyceride concentrations start to rise
Hyperphosphatemia
Metabolic acidosis
Tendency to hyperkalemia |
5 |
End stage renal disease (uremia) |
<15 |
Azotemia develops |
Continuum of Renal Disease (anticlockwise model)
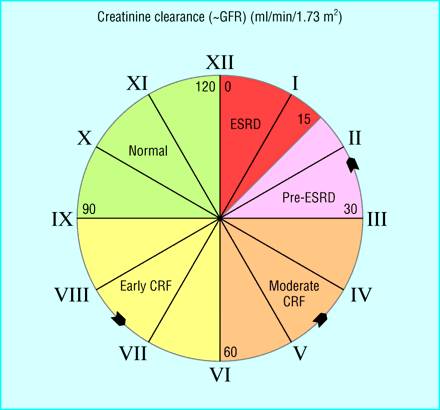
(CRF=chronic renal failure; ESRD=end stage renal disease; GFR=glomerular filtration rate)
Early Detection
Renal disease is often progressive once glomerular filtration rate falls by 25% of normal. Early detection is important to prevent further injury and progressive loss of renal function.
Patients at high risk should undergo evaluation for markers of kidney damage (albuminuria, abnormal urine sediment, elevated serum creatinine) and for renal function (estimation of glomerular filtration rate from serum creatinine) initially and at periodic intervals depending on the underlying disease process and stage of renal disease. Potentially reversible causes should be identified and effectively treated if a sudden decline in renal function is observed.
Risk Factors for Chronic Renal Disease
Risk factors (Factors that increase the risk of kidney damage)
- Age
- Diabetes*
- Hypertension*
- Family history of renal disease
- Renal transplant
Initiation factors (Factors that initiate kidney damage)
- Diabetes*
- Hypertension*
- Autoimmune diseases
- Primary glomerulopathies
- Systemic infections
- Nephrotoxic agents
Progression factors (Factors that cause progressive decline in renal function after onset of kidney damage)
- Persistent activity of underlying disease
- Persistent proteinuria
- Elevated blood pressure*
- Elevated blood glucose*
- High protein/phosphate diet
- Hyperlipidemia*
- Hyperphosphatemia
- Anemia
- Cardiovascular disease
- Smoking*
Other factors:
- elevated angiotensin II,
- hyperaldosteronism,
- increased endothelin,
- decreased nitric oxide
*Common modifiable cardiovascular risk factors
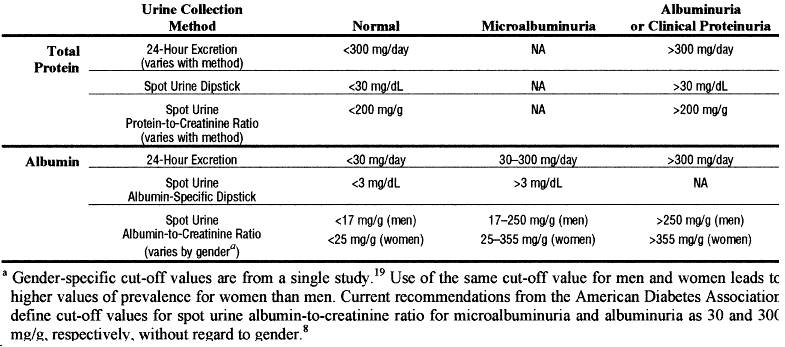
Definition of urinary albumin or protein excretion
- Normal albumin excretion: <30 mg/24 hours
- Microalbuminuria: 20-200 µg/min or 30-300 mg/24 hour or
in men urine albumin/creatinine 2.5-25 mg/mmol
in women urine albumin/creatinine 3.5-35 mg/mmol
- Macroalbuminuria (overt proteinuria): >300 mg/24 hour
- Nephrotic range proteinuria: >3 g/24 hour
Potentially reversible causes of worsening renal function
- Effective circulatory volume depletion: dehydration, heart failure, sepsis
- Obstruction: urinary tract obstruction
- Uncontrolled hypertension
- Toxic causes: nephrotoxic or radiocontrast agents
Diabetes
Diabetes is a common cause of chronic renal failure and accounts for a large part of the growth in end stage renal disease in North America. Effective control of blood glucose and blood pressure reduces the renal complications of diabetes.
Meticulous control of blood glucose has been conclusively shown to reduce the development of microalbuminuria by 35% in type 1 diabetes (diabetes control and complications trial) and in type 2 diabetes (United Kingdom prospective diabetes study). Other studies have indicated that glycemic control can reduce the progression of diabetic renal disease. Adequate control of blood pressure with a variety of antihypertensive agents, including angiotensin converting enzyme inhibitors, has been shown to delay the progression of albuminuria in both type 1 and type 2 diabetes. Recently, angiotensin receptor blockers have been shown to have renoprotective effects in both early and late nephropathy due to type 2 diabetes.
Management strategies for diabetic nephropathy (Ensure effective control of common cardiovascular risk factors for example, lipids, smoking at all times)
Initial stage (normal albumin excretion, <30 mg/24 hours):
- Optimal glycemic control (hemoglobin A1c <7%)
- Target blood pressure <130/80 mm Hg
- Monitor urinary albumin excretion
Incipient nephropathy (microalbuminuria, 30-300 mg/24 hour or 20-200 µg/min):
- Optimal glycemic control (hemoglobin A1c <7%)
- Target blood pressure <125/75 mm Hg
- Control urinary albumin excretion, irrespective of blood pressure
- Angiotensin inhibition
Overt nephropathy (albumin excretion >300):
- Optimal glycemic control (hemoglobin A1c <7%)
- Target blood pressure <125/75 mm Hg
- Control urinary protein excretion
- Angiotensin inhibition, irrespective of blood pressure
- Avoid malnutrition
- Modest protein restriction, in selected groups
Nephropathy with renal dysfunction:
- Optimal glycemic control; avoid frequent hypoglycemia
- Target blood pressure <125/75 mm Hg
- Angiotensin inhibition
- Watch for hyperkalemia
- Avoid malnutrition; consider protein and phosphate restriction
End stage renal disease:
- Renal replacement transplantation or dialysis
- Monitor for hyperkalemia
- Hold angiotensin inhibition (when glomerular filtration <15 ml/min) in selected patients
Hypertension
Hypertension is a well established cause, a common complication, and an important risk factor for progression of renal disease. Controlling hypertension is the most important intervention to slow the progression of renal disease.
Any antihypertensive agents may be appropriate, but angiotensin converting enzyme inhibitors are particularly effective in slowing progression of renal insufficiency in patients with and without diabetes by reducing the effects of angiotensin II on renal hemodynamics, local growth factors, and perhaps glomerular permselectivity. Non-dihydropyridine calcium channel blockers have also been shown to retard progression of renal insufficiency in patients with type 2 diabetes. Recently, angiotensin receptor blockers (irbesartan and losartan) have been shown to have a renoprotective effect in diabetic nephropathy, independent of reduction in blood pressure. Early detection and effective treatment of hypertension to target levels is essential. The benefit of aggressive control of blood pressure is most pronounced in patients with urinary protein excretion of >3 g/24 hours.
Target blood pressure in renal disease
- Blood pressure of <130/85 mm Hg in all patients with renal disease
- Blood pressure of <125/75 mm Hg in patients with proteinuric renal disease (urinary protein excretion 1 g/24 hours)
Proteinuria
Proteinuria, previously considered a marker of renal disease, is itself pathogenic and is the single best predictor of disease progression. Reducing urinary protein excretion slows the progressive decline in renal function in both diabetic and non-diabetic kidney disease.
Angiotensin blockade with angiotensin converting enzyme inhibitors or angiotensin receptor blockers is more effective at comparable levels of blood pressure control than conventional antihypertensive agents in reducing proteinuria, decline in glomerular filtration rate, and progression to end stage renal disease.
Intake of dietary protein
The role of dietary protein restriction in chronic renal disease remains controversial. The largest controlled study initially failed to find an effect of protein restriction, but secondary analysis based on achieved protein intake suggested that a low protein diet slowed the progression. However, early dietary review is necessary to ensure adequate energy intake, maintain optimal nutrition, and avoid malnutrition.
Dyslipidemia
Lipid abnormalities may be evident with only mild renal impairment and contribute to progression of chronic renal disease and increased cardiovascular morbidity and mortality. A meta-analysis of 13 controlled trials showed that hydroxymethyl glutaryl coenzyme A reductase inhibitors (statins) decreased proteinuria and preserved glomerular filtration rate in patients with renal disease, an effect not entirely explained by reduction in blood cholesterol.
Phosphate and parathyroid hormone
Hyperparathyroidism is one of the earliest manifestations of impaired renal function, and minor changes in bones have been found in patients with a glomerular filtration rate of 60 ml/min. Precipitation of calcium phosphate in renal tissue begins early, may influence the rate of progression of renal disease, and is closely related to hyperphosphataemia and calcium phosphate (Ca×P) product. Precipitation of calcium phosphate should be reduced by adequate fluid intake, modest dietary phosphate restriction, and administration of phosphate binders to correct serum phosphate. Dietary phosphate should be restricted before the glomerular filtration rate falls below 40 ml/min and before the development of hyperparathyroidism. The use of vitamin D supplements during chronic renal disease is controversial.
Smoking
Smoking, besides increasing the risk of cardiovascular events, is an independent risk factor for development of end stage renal disease in men with kidney disease. Smoking cessation alone may reduce the risk of disease progression by 30% in patients with type 2 diabetes.
Anemia
Anemia of chronic renal disease begins when the glomerular filtration rate falls below 30-35% of normal and is normochromic and normocytic. This is primarily caused by decreased production of erythropoietin by the failing kidney, but other potential causes should be considered. Whether anemia accelerates the progression of renal disease is controversial. However, it is independently associated with the development of left ventricular hypertrophy and other cardiovascular complications in a vicious cycle.
Perpetuating triad of chronic kidney disease, anemia, and cardiovascular disease
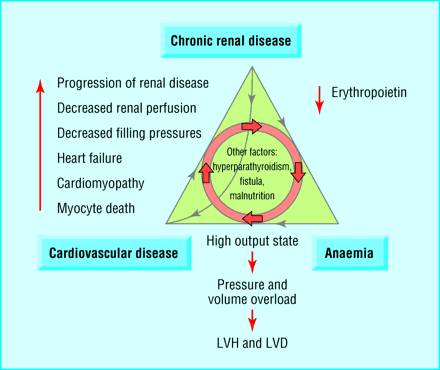
(LVH=left ventricular hypertrophy; LVD=left ventricular dilatation)
Treatment of anemia with recombinant human erythropoietin may slow progression of chronic renal disease but requires further study. Treatment of anemia results in partial regression of left ventricular hypertrophy in both patients with pre-end stage renal disease and patients receiving dialysis and has reduced the frequency of heart failure and hospitalization among patients receiving dialysis.
Both National Kidney Foundation and European best practice guidelines recommend evaluation of anemia when hemoglobin is <11 g/dl and consideration of recombinant human erythropoietin if hemoglobin is consistently <11 g/dl to maintain a target hemoglobin of >11 g/dl.
Prevention or attenuation of complications and comorbidities
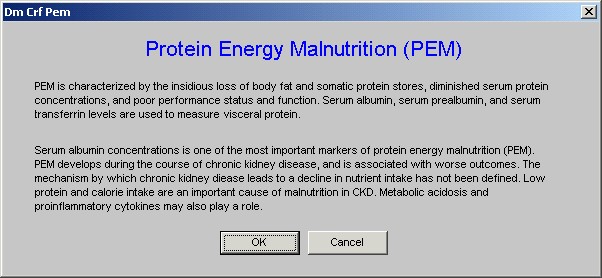
Malnutrition
The prevalence of hypoalbuminemia is high among patients beginning dialysis, is of multifactorial origin, and is associated with poor outcome. Hypoalbuminemia may be a reflection of chronic inflammation rather than of nutrition in itself. Spontaneous intake of protein begins to decrease when the glomerular filtration rate falls below 50 ml/min. Progressive decline in renal function causes decreased appetite, thereby increasing the risk of malnutrition. Hence early dietary review is important to avoid malnutrition. Adequate dialysis is also important in maintaining optimal nutrition.
Cardiovascular disease
The prevalence, incidence, and prognosis of clinical cardiovascular disease in renal failure is not known with precision, but it begins early and is independently associated with increased cardiovascular and all cause mortality. Both traditional and uremia specific risk factors (anemia, hyperphosphatemia, hyperparathyroidism) contribute to the increased prevalence of cardiovascular disease. Cardiac disease, including left ventricular structural and functional disorders, is an important and potentially treatable comorbidity of early kidney disease.
No specific recommendations exist for either primary or secondary prevention of cardiovascular disease in patients with chronic renal disease. Current practice is mostly derived from studies in patients with diabetic or non-renal disease. At present, in the absence of evidence, clinical judgment indicates effective control of modifiable and uraemia specific risk factors at an early stage of renal disease; definitive guidelines for intervention await well designed, adequately powered prospective studies.
Preparing patient for renal replacement treatment
Integrated care by the primary care physician, nephrologist, and renal team from an early stage is vital to reduce the overall morbidity and mortality associated with chronic renal disease. Practical points helpful at this stage of renal disease include
- Patients should be referred to a nephrologist before serum creatinine is 150-180 µmol/l
- Patients receiving comprehensive care by the renal team have shown slower rates of decline in renal function, greater probability of starting dialysis with higher hemoglobin, better calcium control, a permanent access, and a greater likelihood of choosing peritoneal dialysis
- Patients with progressive renal failure should be educated to save vessels of the non-dominant arm for future hemodialysis access; they should have a permanent vascular access (preferably arteriovenous fistula) created when the glomerular filtration rate falls below 25 ml/min or renal replacement treatment is anticipated within a year
- Patients starting dialysis at relatively higher levels of residual renal function (early starts) have better solute clearance, less malnutrition, better volume control, and less morbidity and mortality than patients starting at traditional low levels of renal function (late starts).
Conclusion
Chronic renal failure represents a critical period in the evolution of chronic renal disease and is associated with complications and comorbidities that begin early in the course of the disease. These conditions are initially subclinical but progress relentlessly and may eventually become symptomatic and irreversible. Early in the course of chronic renal failure, these conditions are amenable to interventions with relatively simple treatments that have the potential to prevent adverse outcomes.
Figure Three summarizes strategies for effective management of chronic renal disease. By acknowledging these facts, we have an excellent opportunity to change the paradigm of management of chronic renal failure and improve patient outcomes.
Strategies for active management of chronic renal disease
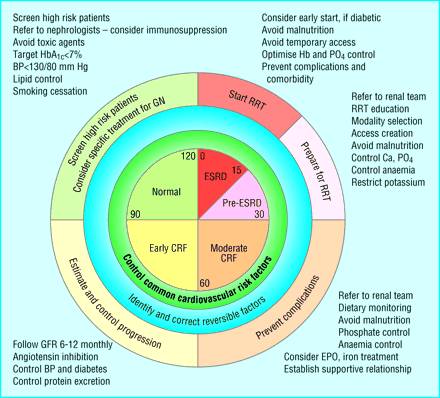
(BP=blood pressure; Ca=calcium; CRF=chronic renal failure; EPO=erythropoietin; ESRD=end stage renal disease; GN=glomerulonephritis; GFR=glomerular filtration rate; Hb=hemoglobin; PO4=phosphate; RRT=renal replacement treatment)
Comment about Cystatin C
A single blood test, cystatin C, correlates well with gold standard GFR, is sensitive for the detection of moderate chronic renal failure (4), including amongst older people (5), and circumvents the analytical problems of serum creatinine and the complexities of formulaic estimates. Given the wealth of recent published research into the use of cystatin C we were surprised not to read about it in an otherwise excellent and up to date article.
It is true that serum cystatin C concentration is a better marker that serum creatinine for detection of subtle changes in GFR, especially in the elderly. However, limited sample size, statistical methodology, lack of information on cystatin C assay calibration, and conflicting results make the available data inadequate for recommending cystatin C measurement for widespread clinical application at present.
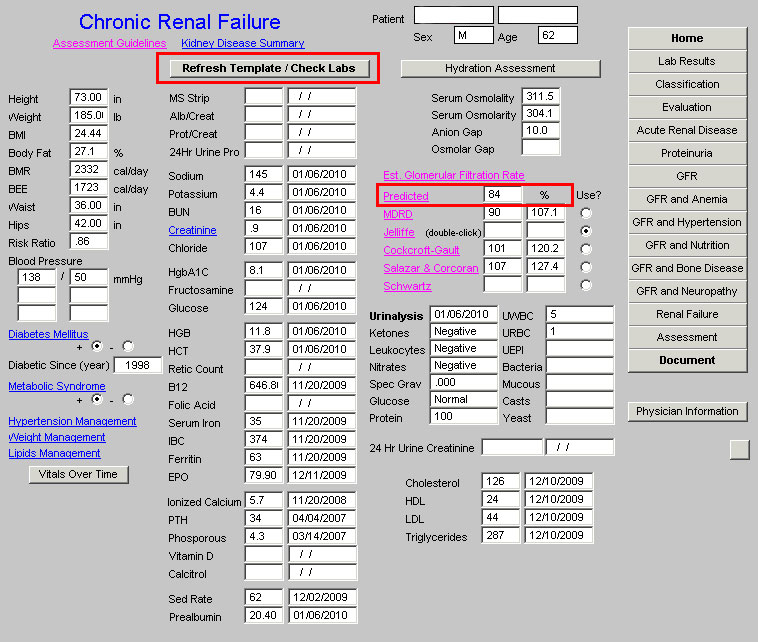
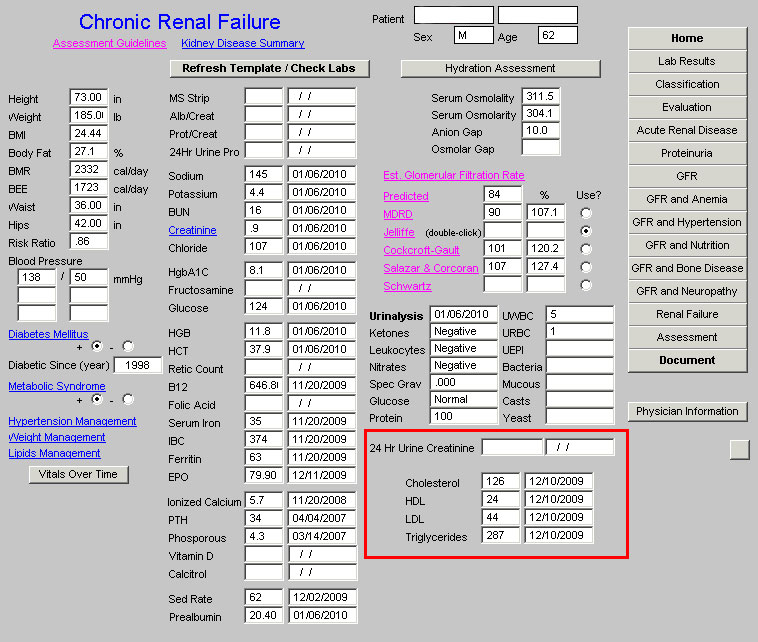
SETMA’s Chronic-Renal-Disease Disease-Management Suite of templates can be found by gong to AAA Home and clicking on Renal Failure which is outlined in red below.
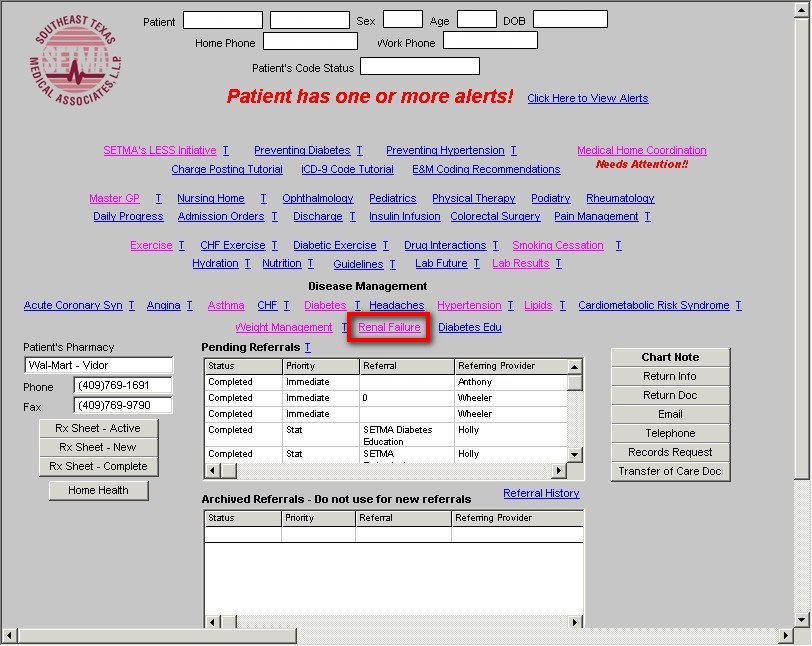
When that button is clicked the Master Renal Failure template appears.
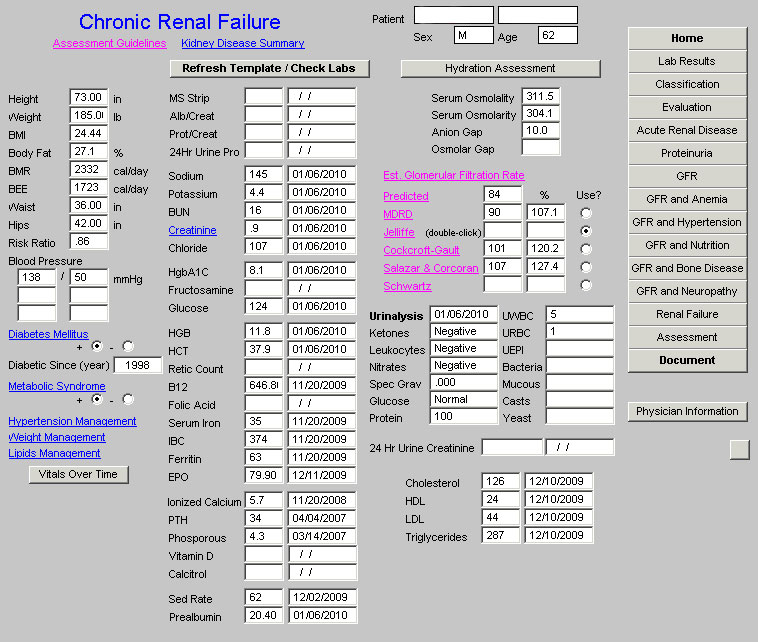
Across the top of this template, you will find the following functions
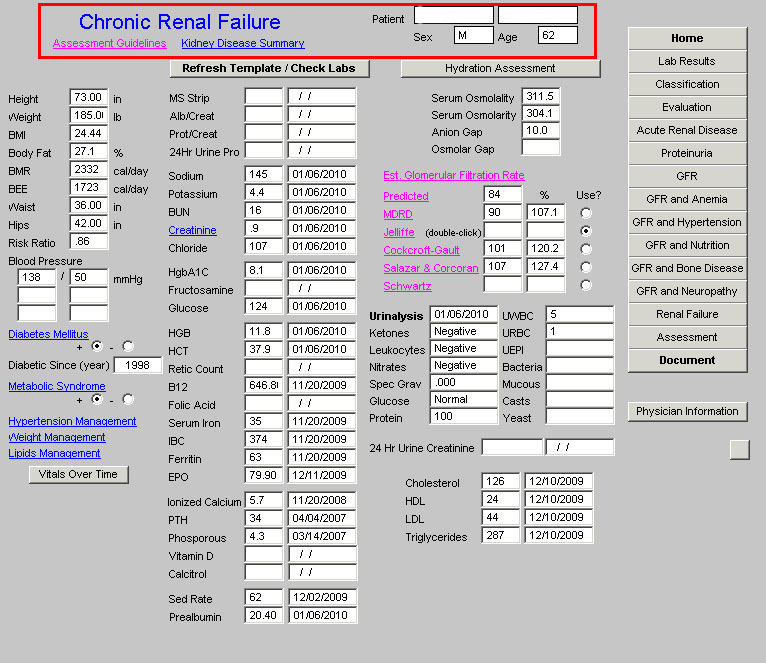
- Title: Chronic Renal Failure
- Assessment Guidelines
- Kidney Disease Summary
- Patient’s Name
- Gender
- Age
These functions are the foundation of SETMA’s Chronic Kidney Disease evaluation. When accessed the Assessment Guidelines displays the National Kidney Foundation’s Guidelines for Assessment of Kidney Function. :
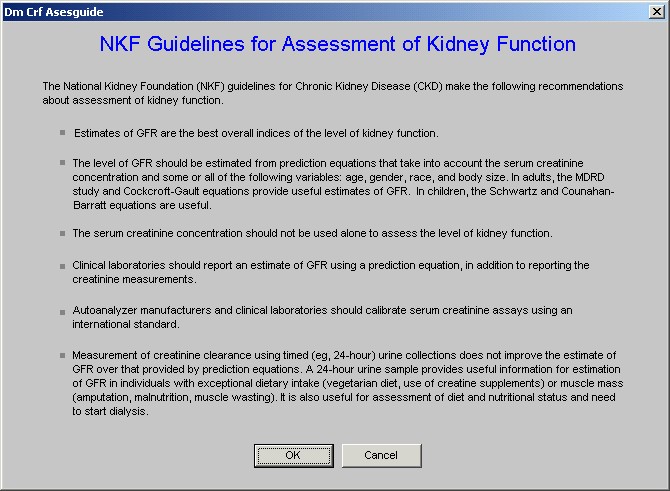
When accessed the Kidney Disease Summary displays the same information as is contained in the ten-page introduction which begins this tutorial.
The remainder of the Master Template is organized into three columns.
The first column displays the patient’s vital signs and links to five related disease management tools:
There is also a button which launches the Vitals over Time function
The following screen shot of the Chronic Renal Failure master template shows this section outlined in red.
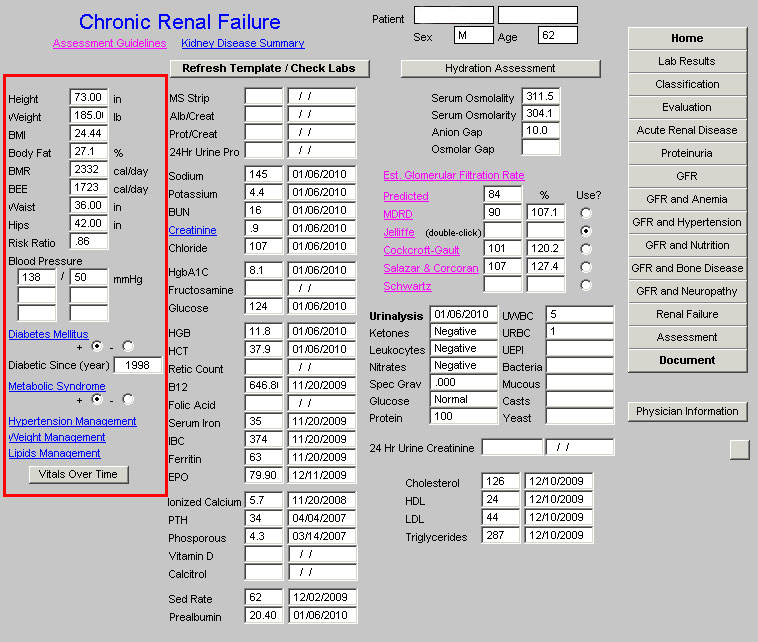
The abbreviations in this column which may note be familiar are:
- BMI – Body Mass Index
- BMR – Basal Metabolism Rate
- BEE – Basal Energy Expenditure
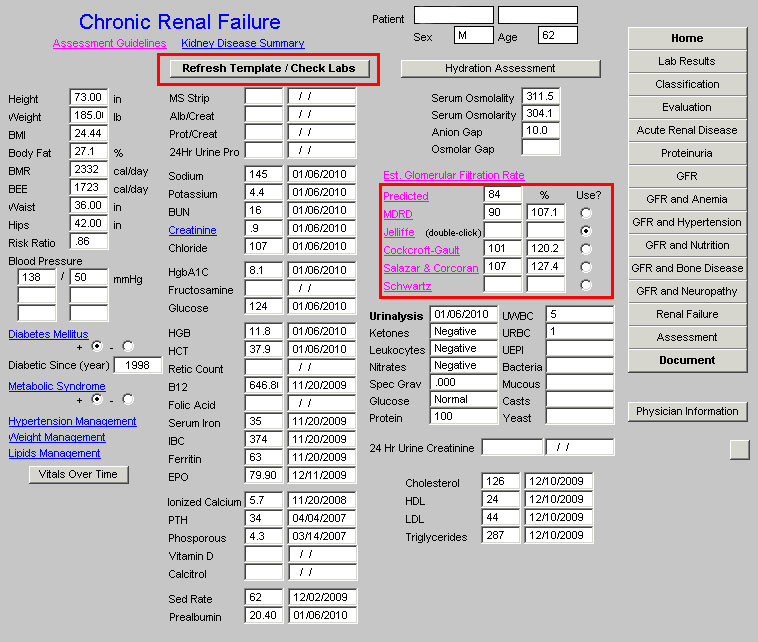
The Second Column begins with a button entitled “Refresh Template/Check Labs” and then lists 40 laboratory values which are related to Chronic Renal Disease. In the third column, just under the formulae for calculating the estimated GFR, additional lab values are displayed which include the Urinalysis, 24 hour urine Creatinine Clearance and the lipid panel.
When the “Refresh Template/Check Labs” is clicked, the laboratory data in column two and at the bottom of column three is updated, and the values for the estimated Glomerular Filtration Rates (see below) are calculated.
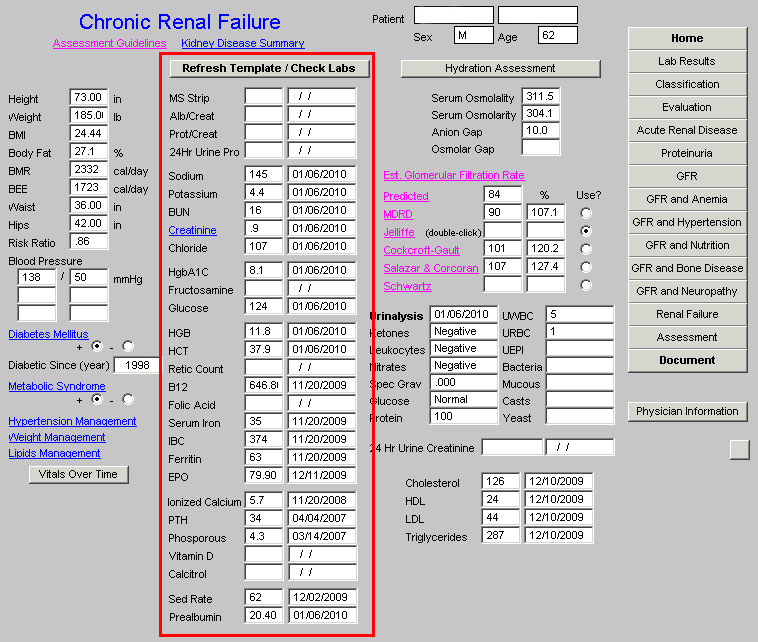
The laboratory values are organized according to the following categories:
Proteinuria – MS Strip, Albumin/Creatinine Ratio, Protein/Creatinine Ratio, 24-hour urine protein
Electrolytes – Sodium, P:otassium, Bun, Creatinine, Chloride
Diabetes – Hgb A1C, Fructosamine, Glucose
Anemia – Hgb, HCT, Reticulocyte Count, B12, Folic Acid, Serum Iron, IBC, Ferritin, Erythropoietin
Bone Disease – ionized calcium, PTH, Phosphorus, Vitamin D, Calcitrol
Random – Sed Rate and Prealbumin
Urinalysis
Lipids – Cholesterol, HDL, LDL, Triglycerides
These values are relevant to the evaluation and treatment of Chronic Renal Disease as it progresses from Stage I into ESRD.
The third column displays the following:
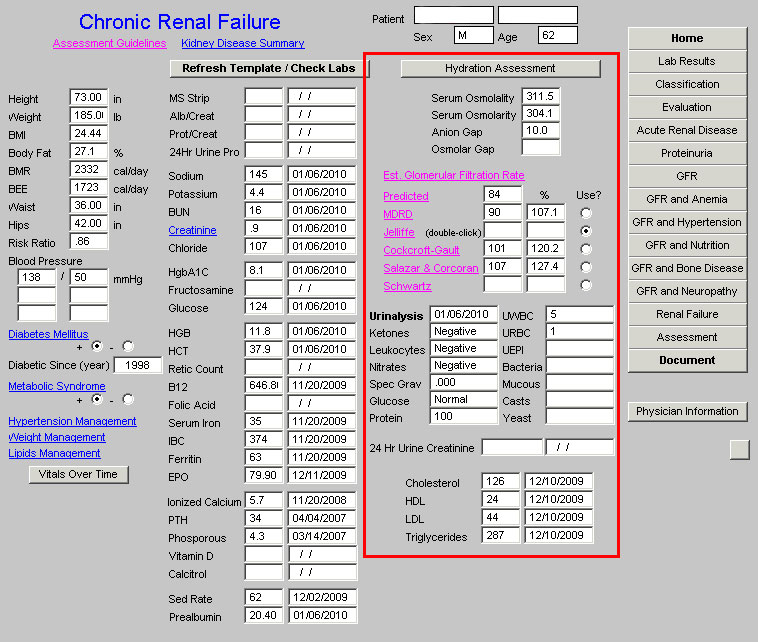
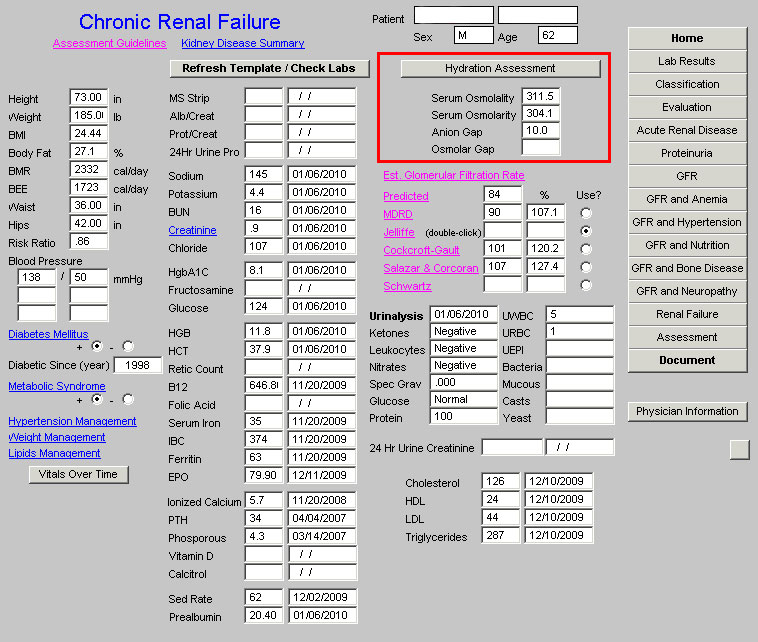
At the top of the third column is a link to the Hydration Assessment Tool which is followed by boxes for four values.
- Serum Osmolality
- Serum Osmolarity
- Anion Gap
- Osmolar Gap
These values are displayed if the Hydration Assessment Template has been completed. If it has not been, it can be completed by clicking on Hydration and following the simple steps of evaluating the risk of dehydration, the physical signs of dehydration and the metabolic evidence of dehydration .
The next function in this third column is a button entitled “Est Glomerular Filtration Rate”, which launches an educational piece entitled “Clinical Applications of Equations to Predict GFR”.
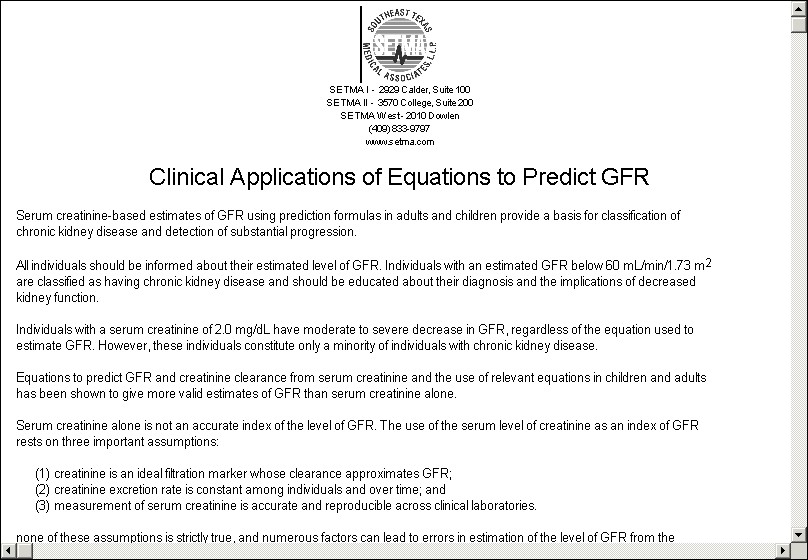
Following this education piece are six different formulae for calculating the estimated GFR
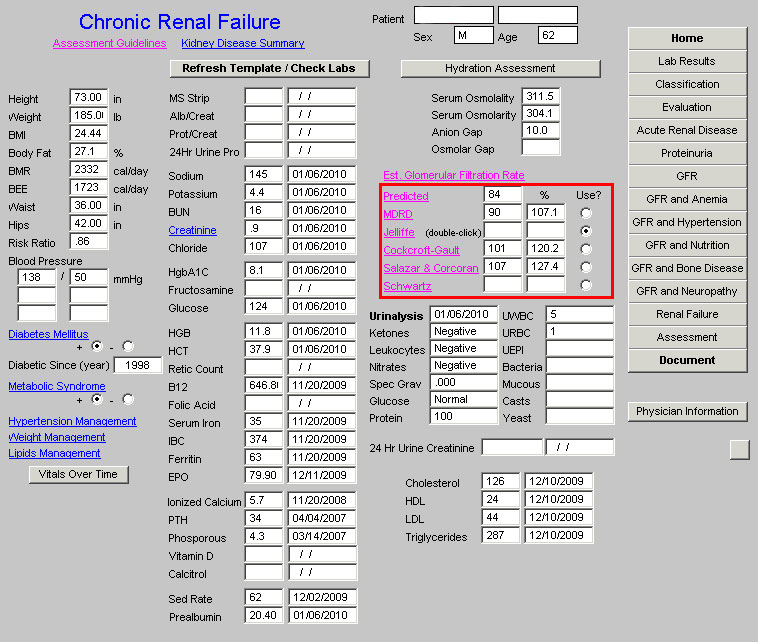
SETMA displays six formulae for which the Calculated GFR can be determined. They are:
- Predicted
- MDRD – this is often considered the most accurate
- Jelliffee – this may be more accurate in patients with unstable renal disease. As will be seen this formula involves a multi-stage process for calculation.
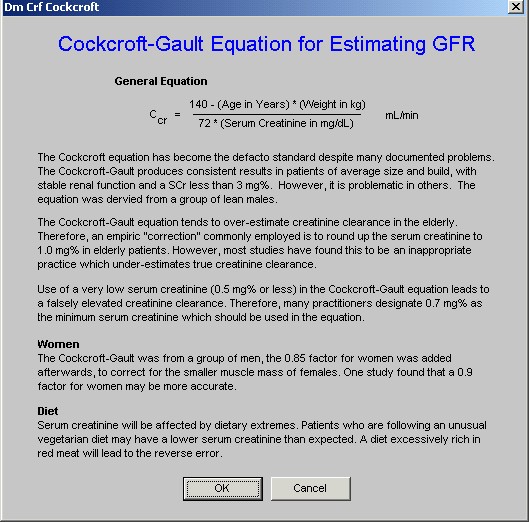
- Cockcroft-Gault – even though there are documented problems with this formula, it is often considered the standard.
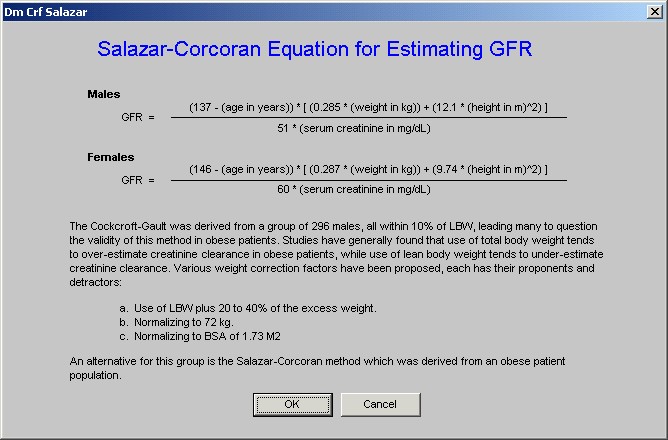
- Salazar-Corcoran – this formula may be more accurate in obese patients.
- Schwartz – this formula may be more accurate in children
Each of the formulae has its own limitations and benefits. All six formulae will be discussed later, but at this point, we will address “MDRD” which is the formula SETMA uses in determinng the Stage of Renal Disease.
Once the button entitled “Refresh Template/Check Labs’ is deployed, the calculated GFR will appear beside each of the formulae names.
You will notice that the titles of each of the formulae are highlighted, which means that they are hyperlinks. If you click on the names, an information pop-up is deployed for each. The second formula, and the first we will discuss, is entitled “MDRD,” which stands for “Modification of Diet in Renal Disease.” When the “MRDR” button is depressed, the following pop-up appears which explains the origin of this formula.
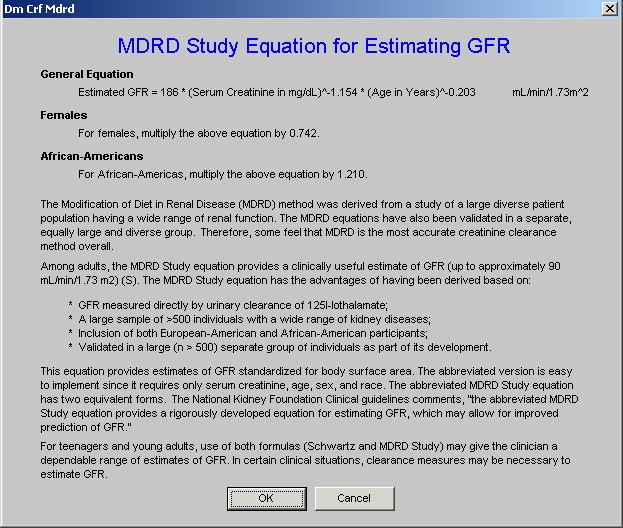
As indicated on this pop-up, many feel that this is the most accurate of the formulae and “MDRD” is the formula SETMA uses in order to calculate the state of renal disease, if any. The other five GFR estimation formulae will be discussed later. To skip to that discussion click here.
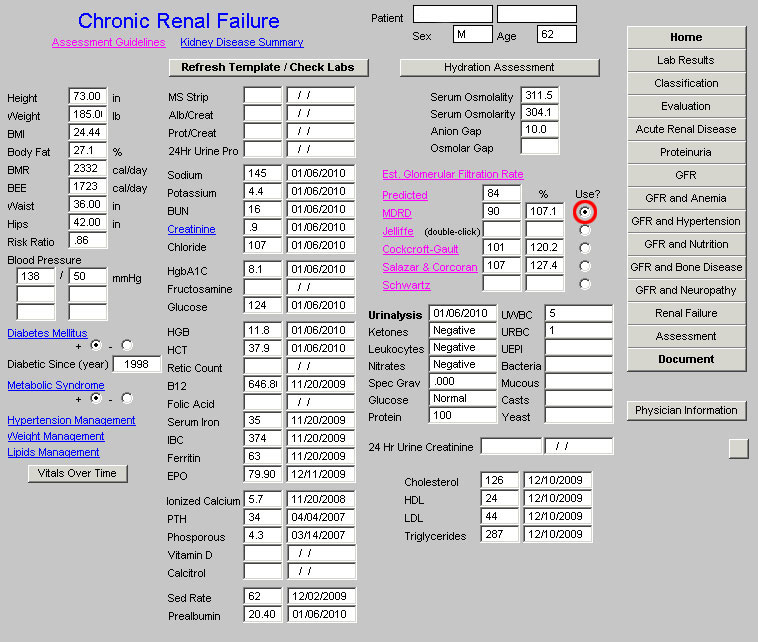
When the “Refresh Template/Check Labs” button is depressed, the box next to “MDRD”, will be automatically checked. In order to use this in the calculation of the stage of renal disease, it is necessary to manually click in any of the boxes next to one of the other formulae and then recheck the box by the “MDRD” calculated GFR. Once this is done, it is possible to calculate the stage of renal disease as will be discussed below. (This action “loads” the computation of Stage of Renal Disease with the formula which will be used for the determination of the estimated GFR which will in turn be used to calculate the Stage of Renal Disease.)
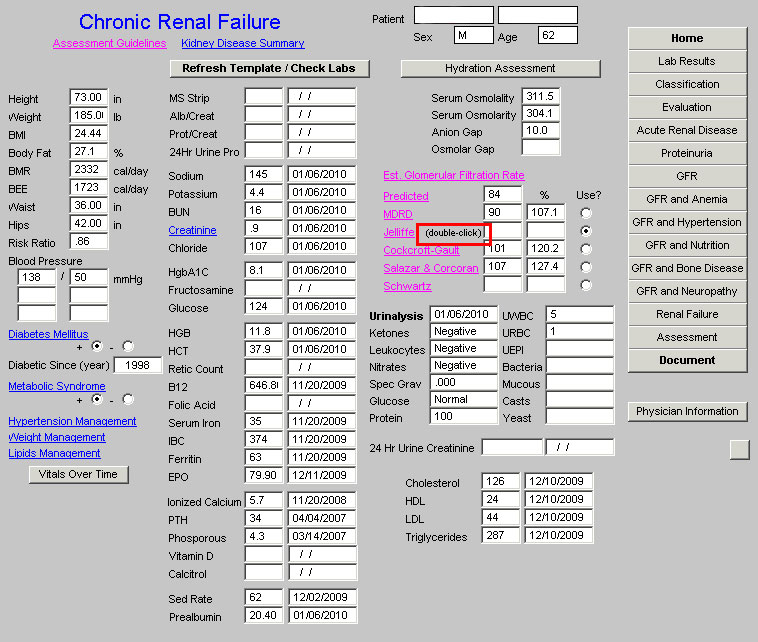
The following is a screen shot of the Master Renal Template after the “Refresh Template/Check Labs” has been clicked. Notice the box next to “MDRD” is checked.
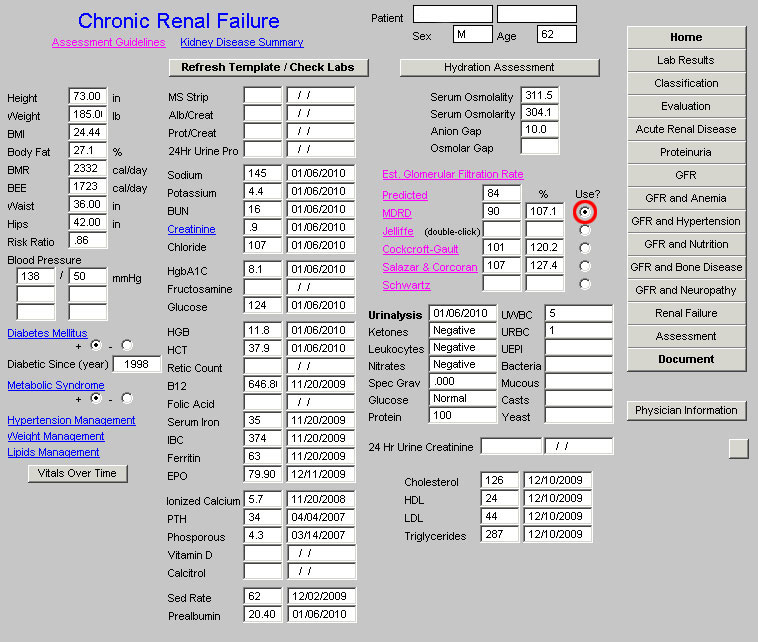
Now it is important to place a check mark in the box beside any formula other than MDRD. See the following screen shot with a red circle around the check box beside the Jeffittee formula box.
Now, you must manually return the check mark to the box by “MDRD.” This process “loads” the equation for the calculation of the Stage of Renal Disease. If you miss this step, you will be told that you have to answer all questions and you will have to come back to this point and take this step before proceeding.
An explanation of the other five formulae will be presented below, but at this point, we will present the explanation of how to complete the evaluation of the stage of renal disease.
After removing the check box from beside the MDRD, placing it next to any of the other five formulae and then returning it to the box next to MDRD, you must select the navigation button entitled “Evaluation” in the fourth column of the Master Renal template. It is outlined in red below.
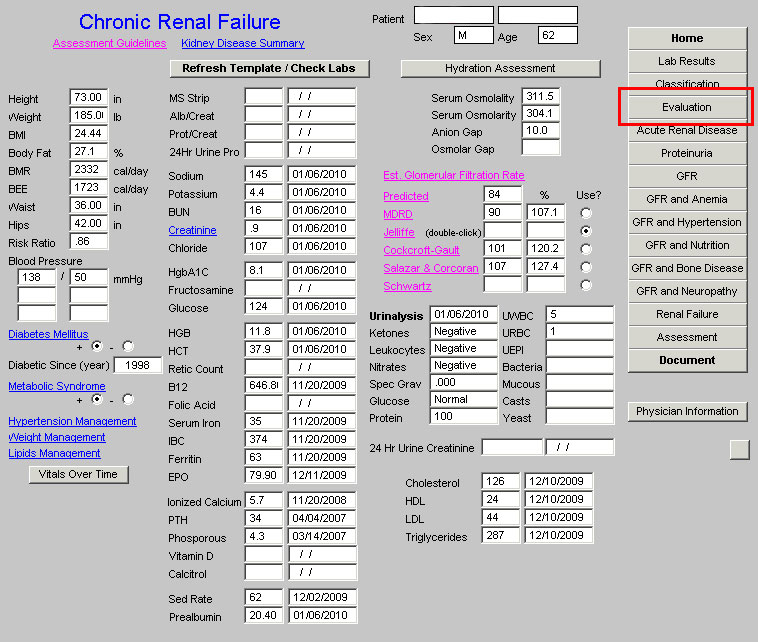
When the “Evaluation” button is depressed, the following template appears.
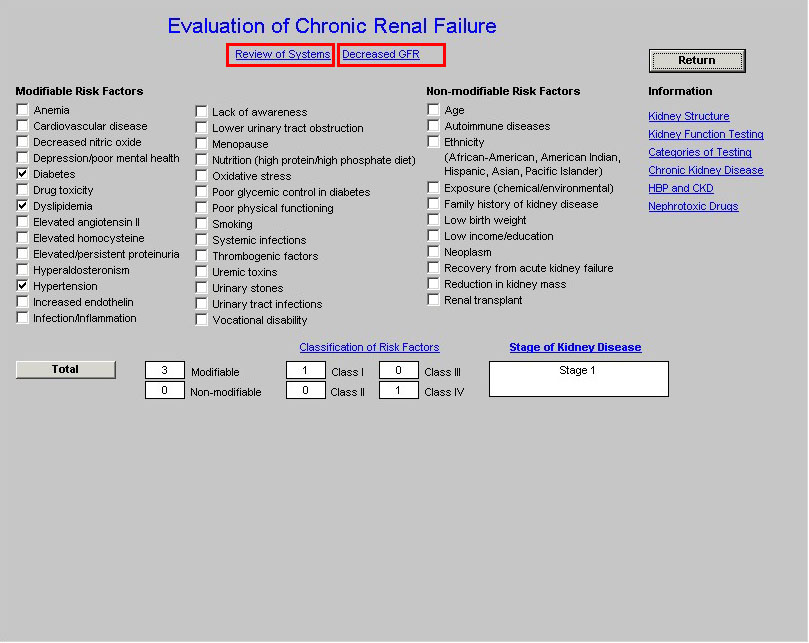
At the top of this template are two buttons:
- Review of Systems
- Decreased GFR
When the Review of Systems button is depressed a pop-up appears entitled Chronic Renal Failure Signs and Symptoms. This displays three classes of signs and symptoms of Chronic Renal disease.
- Initial Symptoms,
- Later Symptoms and
- Additional Symptoms.
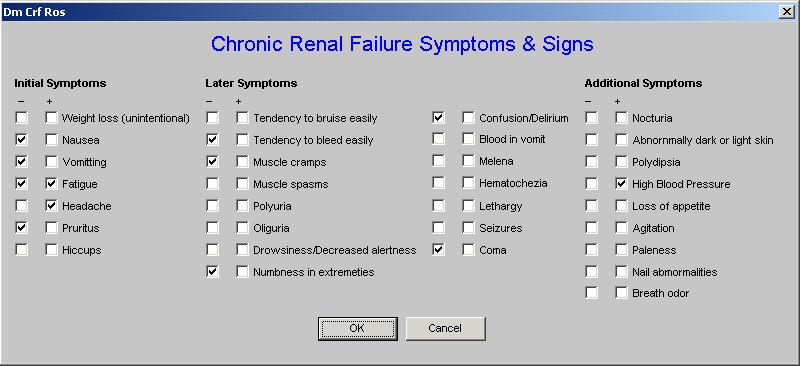
The signs and symptoms which are captured elsewhere in the EMR are automatically checked off, others can be added.
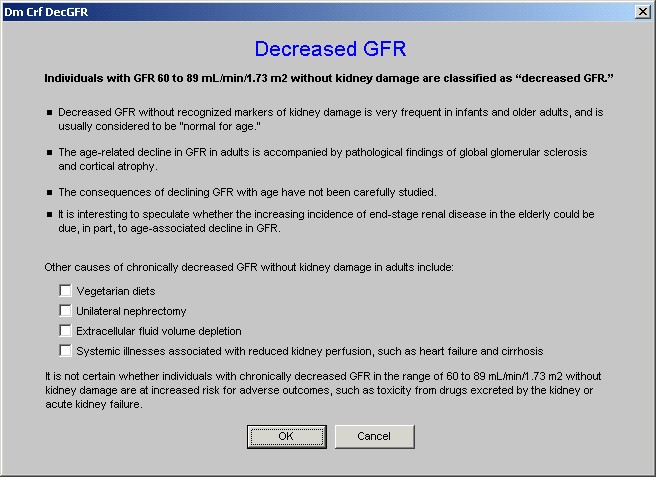
The next button on the Evaluation template is entitled “Decreased GFR”. When that button is activated, the following pop-up appears. It gives a definition of Decrease GFR in the absence of renal disease and also the causes of decreased GFR in the absence of renal disease
Beneath the above two buttons on the Evaluation Template are three columns which display Modifiable Risk Factors and Non-modifiable Risk Factors for Renal Disease. Those factors which are captured elsewhere in the EMR are automatically documented. The provider can mark others which apply.
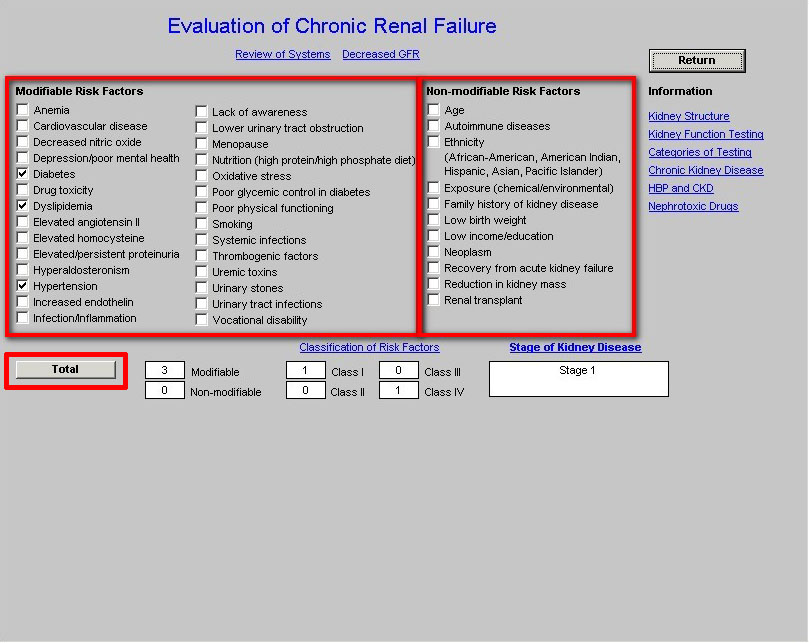
To complete the process of calculating the stage of Chronic Renal Disease, click the button entitled Total. This will do the following:
- Cause the Risk Factors to be totaled into a Modifiable and Non-Modifiable box and
- Cause the Risk Factors to be totaled into one of Four Classes of Risk Factors entitled Class I, Class II, Class III, Class IV.
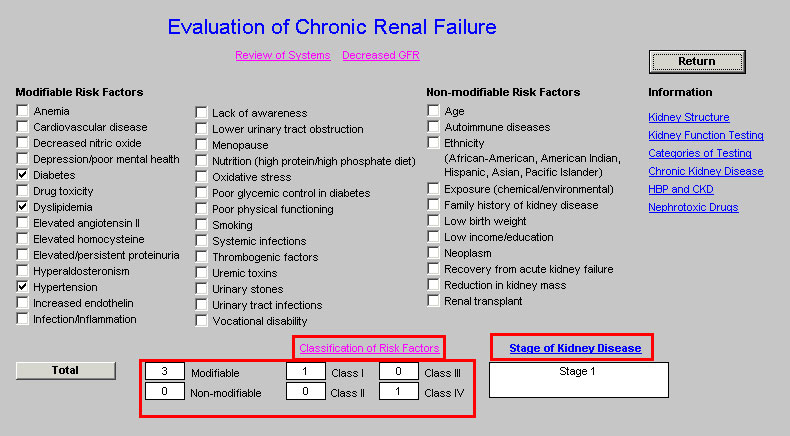
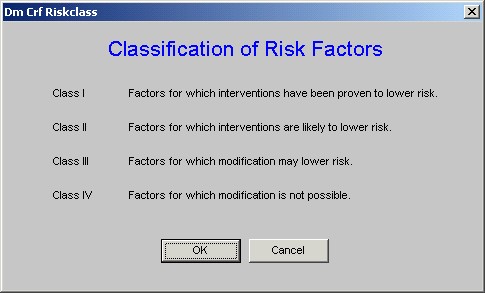
Above the Class I, II, III and IV Risk Classes totals is a button entitled Classification of Risk Factors. When this button is deployed the following pop-up with an explanation of the four classes appears.
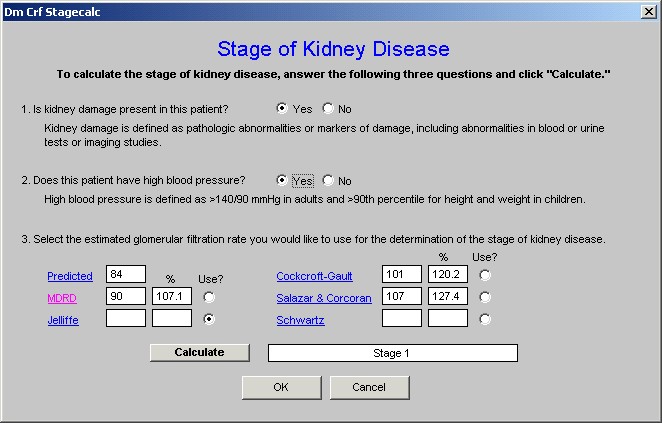
When the Total button is depressed on the Evaluation Template, the following pop-up appears which is entitled Stage of Kidney Disease.
We are now only a step away from the calculation of the Stage of Renal Disease. So far, we are prepared for this process with the following steps:
- Opening the Chronic Renal Disease Master Template.
- Clicking the button entitled Refresh Template/Check Lab.
- Clicking one of the GFR formulae in stead of the MDRD which has been automatically selected.
- Clicking the box next to the MDRD formula
- Clicking the Navigation button in the right hand column entitled Evaluation.
- Clicking the Total button on the Evaluation Template
You are now ready to complete the process of calculating the State of Chronic Renal Disease.. The pop-up which appears when you deploy the Total button on the Evaluation template is entitled Stage of Kidney Disease.
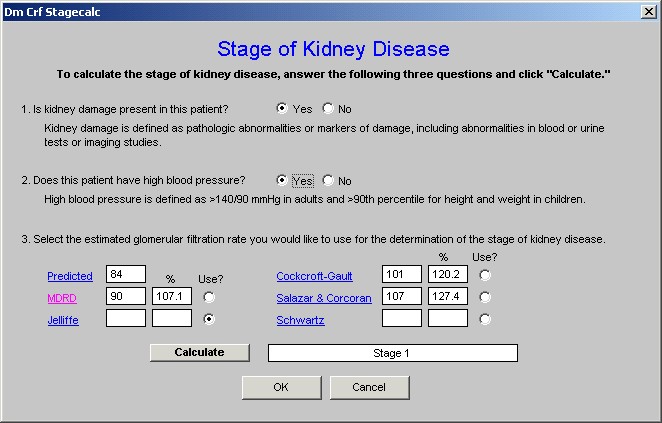
Beneath the title Stage of Renal Disease is the statement, “To calculate the stage of kidney disease, answer the following three questions and click ‘calculate.”” The three questions are:
- Is kidney damage present in this patient? Following the this question is this explanation: Kidney damage is defined as pathologic abnormalities or makers of damage, including abnormalities in blood or urine tests or imaging studies. There are three conditions which allow you to answer “yes” to the question, “Is kidney damage present in this patient”:
a. the presence of microalbuminuria,
b. a serum creatinine above 1.5 and/or
c. an abnormal renal ultrasound which indicates the presence of medical renal disease.
The earliest evidence of kidney damage is the presence of protein in the urine. In the introduction to this tutorial, the National Kidney Foundation defines normal and abnormal urinary albumin or protein excretion
- Normal albumin excretion: <30 mg/24 hours
- Microalbuminuria: 20-200 µg/min or 30-300 mg/24 hour or in men urine albumin/creatinine 2.5-25 mg/mmol and in women urine albumin/creatinine 3.5-35 mg/mmol
- Macroalbuminuria (overt proteinuria): >300 mg/24 hour
- Nephrotic range proteinuria: >3 g/24 hour
(More definitive information on Proteinuria can be found in the explanation of the template entitled Proteinuria)
On the Evaluation template there are six buttons with educational information presented. The fourth button is entitled “Chronic Kidney Disease” and addresses the definition of Chronic Kidney disease. It states:
All individuals with GFR <60 mL/min/1.73 m2 for 3 months are classified as having chronic kidney disease, irrespective of the presence or absence of kidney damage.
- Reduction in kidney function to this level or lower represents loss of half or more of the adult level of normal kidney function,
- This may be associated with a number of complications
All individuals with kidney damage are classified as having chronic kidney disease, irrespective of the level of GFR.
- The rationale for including individuals with GFR 60 mL/min/1.73 m2 is that GFR may be sustained at normal or increased levels despite substantial kidney damage and
- Patients with kidney damage are at increased risk of the two major outcomes of chronic kidney disease: loss of kidney function and development of cardiovascular disease
Once you have answered the first question, “yes,” or “no,” you must answer the second question which is:
- “Does the patient have high blood pressure.”
The definition is then given for the presence of high blood pressure; it is, “High blood pressure is defined as >140/90 in adults and >90 Percentile in height and weight in children.”
If the current blood pressure is elevated, the box indicating “yes” will be automatically selected but if the patient has high blood pressure which is controlled, you will need to manually check the box next to “yes.”
The third question will be automatically answered for you.
- Select the estimated glomerular filtration rate you would like to use for the determination of the stage of kidney disease.
This will automatically default to the MDRD equation and does not need to be changed again.
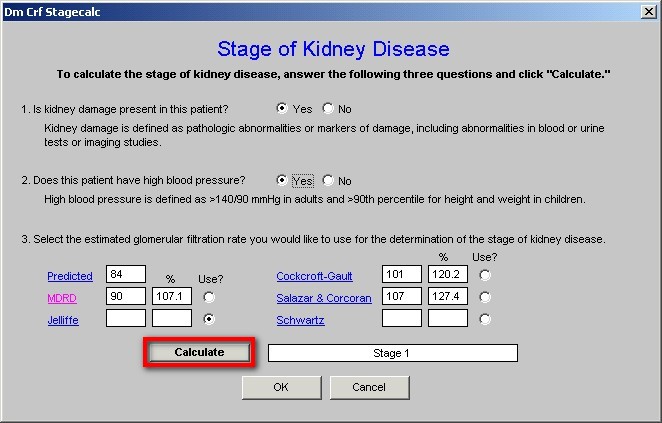
When you depress the “Calculate” button on the Stage of Renal Disease pop-up, the Stage of Renal Disease will appear. Some times, you will receive a message in an alert message which states:
“You MUST answer both questions 1 and 2 as well as select which value is to be used under 3.”
If you have answered questions 1 and 2 and still receive this alert, you must then go back to Chronic Renal Disease Master template and follow the steps which were described above to change the box which was automatically checked beside the MDRD equation. The box must be checked next to another formula and then changed back to MDRD. This alerts the computer that this is the formula which is to be used to calculate the Stage of Chronic
Review of the Steps by which the Stage of Chronic Renal Disease is calculated
The steps to the calculation of the Stage of Renal Disease are as follows. Once learned, these steps take only a few seconds to complete.
- Open the Chronic Renal Disease Master Template.
- Click the button entitled Refresh Template/Check Lab.
- Click one of the GFR formulae in stead of the MDRD which has been automatically selected.
- Click the box next to the MDRD formula
- Click the Navigation button in the right hand column entitled Evaluation.
- Click the Total button on the Evaluation Template
- Answer questions 1 and 2 on the Stage of Kidney Disease Pop-up
- Click the button entitled Calculate on the Stage of Kidney Disease Pop-up
The Stage of Kidney disease will then be displayed and can be added to the ICD-9 Code list under Chronic Conditions and to the Acute Assessment. Any stage of kidney disease is an HCC Risk and needs annual evaluation.
An explanation of the other five formulae for calculating GFR. Click here to go back to the six formulae for calculating Glomerular Filtration Rate.
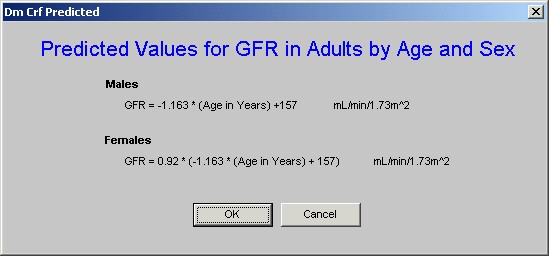
The first formula listed is called “Predicted.”
You will notice that the title of this box “Predicted” is in blue, which means that it is a hyperlink. If you click on “Predicted,” the formula for calculating this Predicted GFR will be displayed.
We have discussed the second formula entitled “MDRD” above. The third formula is entitled “Jeffillee”. The pop-up which appears when the button is clicked states:
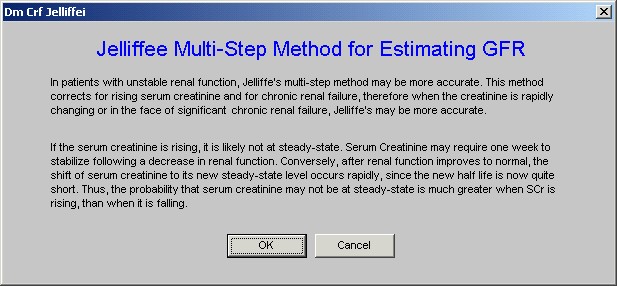
As mentioned previously the Jeffillee formula is the only multi-stage formula. In order to display the estimated glomerular filtration rate calculated by this formula it is necessary to go through several steps.
In the space between the title of this template and the box where the result is displayed is a note which states, “Double Click.”
When you double click in the box next to Jeffillee, the following pop-up is deployed, which is entitled Jeffillee Multi-step Method for Estimating GFR.
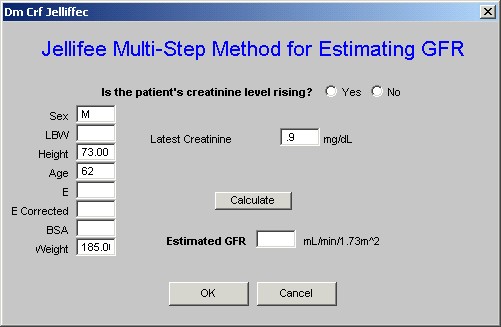
To complete this formula follow the steps indicated.
The fourth formula is the Cockcroft-Gault formula. When the hyperlink is accessed the following pop-up is displayed which gives details about this formula and its value.
The fifth formula is the Salazar & Corcoran formula. The following is the pop-up which appears when this hyperlink is accessed.
The sixth formula is the Schwartz formula. When this hyperlink is accessed, the following pop-up is displayed.
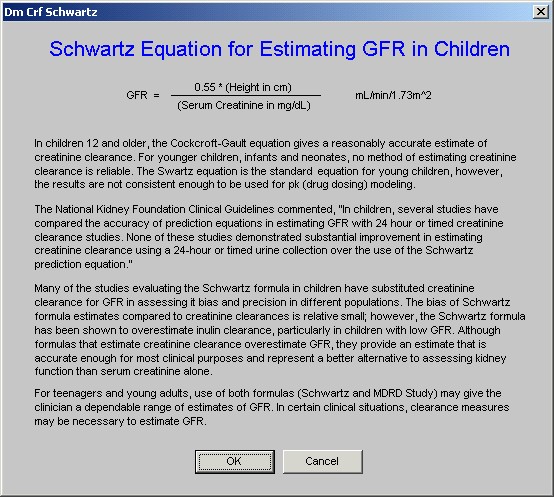
As will be noted by reading this, in dealing with teenagers, the use of the Cockcroft-Gault and Schwartz formulae together may give a better picture of the renal function than either one alone.
Following these six formulae, there is a display of 12 additional lab studies which are discussed above..
The fourth column of the Master Chronic Renal Disease Template contains 16 navigation buttons. Each will be described and its use and means explained. The 16 buttons are outlined in red below:
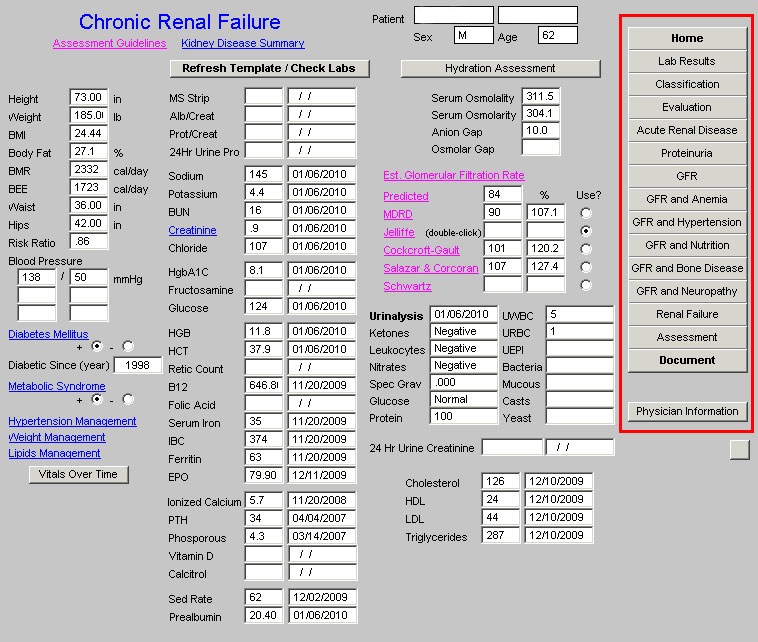
The use of each of these buttons and the functions which they launch will now be described. (For those functions which require more detailed explanation, this general and brief introduction of all of the navigation buttons will be followed by a detailed explanation.)
- Home – this button is used to return the user to the AAA Home template
- Lab Results – this button launches the laboratory results template which will place all current lab on the patient’s Chronic-Renal-Disease chart note. (click here for an explanation of the Lab Results template.)
- Classification – this launches a template which lists the pathology and etiology of most causes of Chronic Renal Disease.
- Evaluation – the content and use of the template has been described above (click here to return to the section on the Evaluation template)
- Acute Renal Failure – this template displays the cause of Acute Renal Failure and explains the three categories of Acute Renal Disease.
- Proteinuria – this template defines microalbuminuria and albuminuria, discusses albumin/creatinine ratio, false positive proteinuria and calculates the degree of proteinuria from laboratory tests which are displayed.
- GFR – this template displays the results of various equations for calculating estimated GFR, discusses the limitations of estimated GFR and calculates the estimated GFR.
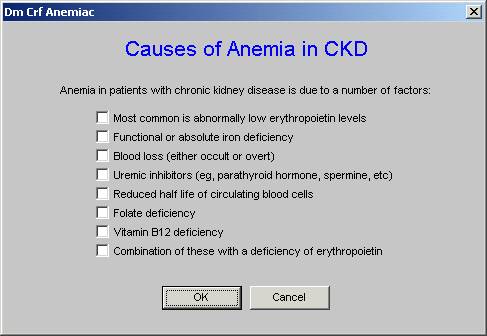
- GFR and Anemia – this template addresses the causes of anemia in Chronic Renal Disease and addresses procrit therapy, dosing and safety.
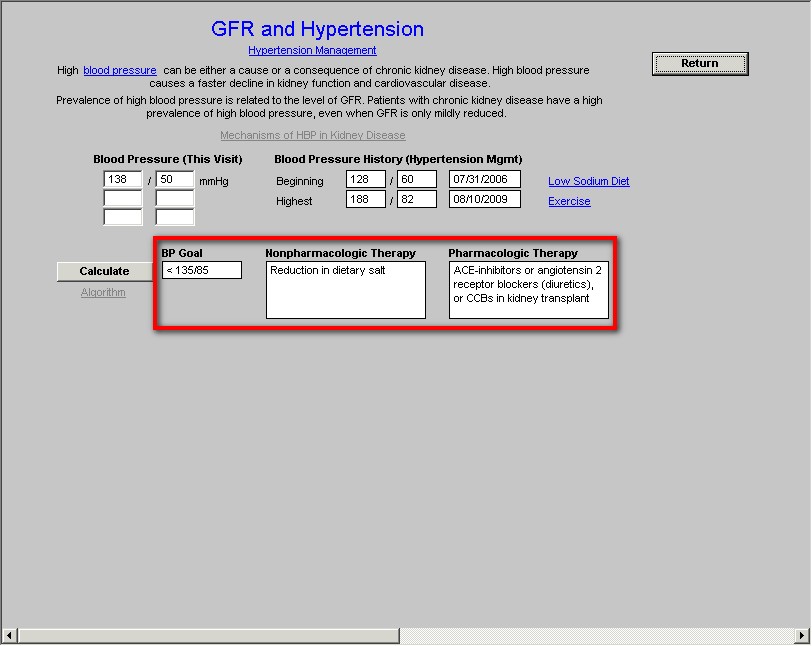
- GFR and Hypertension – this template addresses elevated blood pressure in the patient with Chronic Renal Disease. It includes the ability to identify the mechanisms of blood pressure elevation in Chronic Renal Disease, the goal of blood pressure control, treatment recommendations, and links to SETMA’s hypertension disease management tools, low salt diet, weight management and exercise prescriptions.
- GFR and Nutrition – this template allows for evaluation of Protein Energy Malnutrition (PEM) in chronic renal disease, the definition of PEM, and also calculates Dailey Protein Intake as well as Daily Energy Intake in various stages of Chronic Renal Disease.
- GFR and Bone Disease – this template addresses abnormalities of bone metabolism which is seen in patients with a GFR below 60 ml/min/1.72 meters2. It identifies the importance of Calcium, Phosphate, Vitamin D3, PTH and Ca x PO4 in Chronic Renal Disease.
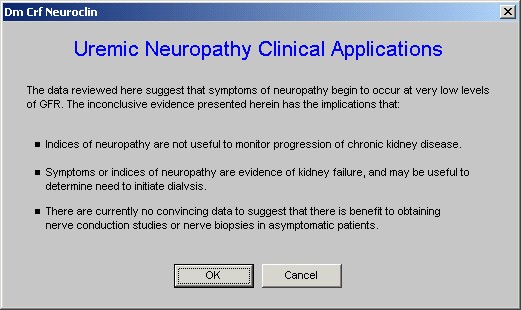
- GFR and Neuropathy – this template discusses the applications of uremic neuropathy including autonomic neuropathy in Chronic Renal Disease. The review of systems and physical examination relevant to uremic neuropathy are discussed.
- Renal Failure – this template discusses common causes of renal failure and common causes of an acute decline in GFR. The definition of renal failure and predicting a decline in GFR are discussed.
- Assessment – this template summarizes the renal status of the patient and includes a summary of the nutritional status, lipid status, Calcium Phosphorus Product, Hyperparathyroidism, Immunizations and habits.
- Document – this button launches the creation of the Renal Chart Note for this patient encounter
- Physician Information – this button launches a series of education documents about the care of patients with renal disease.
Description of the templates launched by Navigation Buttons
Classification
The full title of this template is Classification of Chronic Kidney Disease. In addition to diabetes there are five other classes of chronic kidney disease based on pathology; they are:
- Glomerular Diseases (Primary or Secondary) and these are divided into Proliferative and Non-proliferative
- Vascular Disease
- Tublointerstitial Disease
- Cystic Disease
- Diseases in the Transplant
The template also addresses etiologies of each of the above. Many of the categories and etiologies names are in bold blue, which means that there are documents associated with each of these which give details about each disorder.
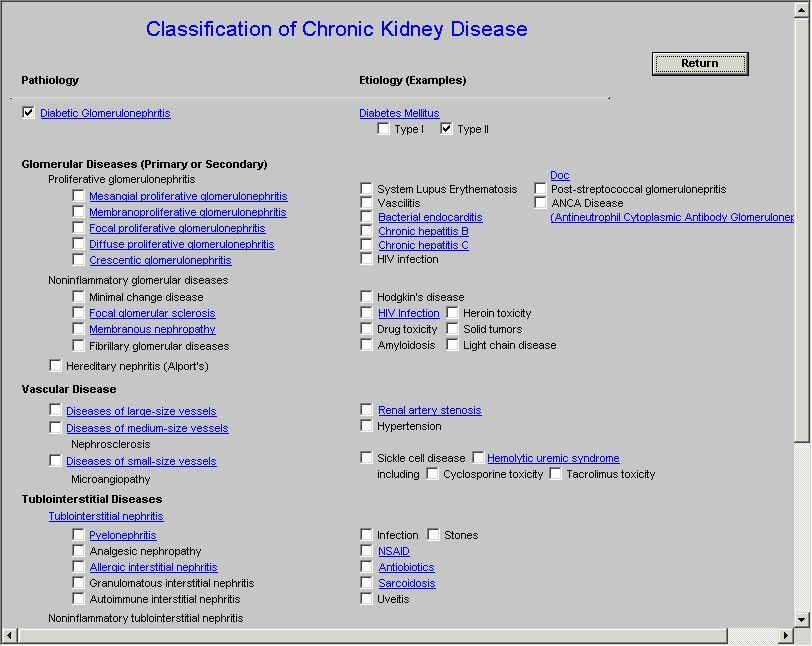
If the pathologic cause of the patient’s renal disease or if the etiology of the patient’s renal disease is selected on the Classification template, it will automatically note that on the Assessment Template (this function does not work at present but will be added in 2010).
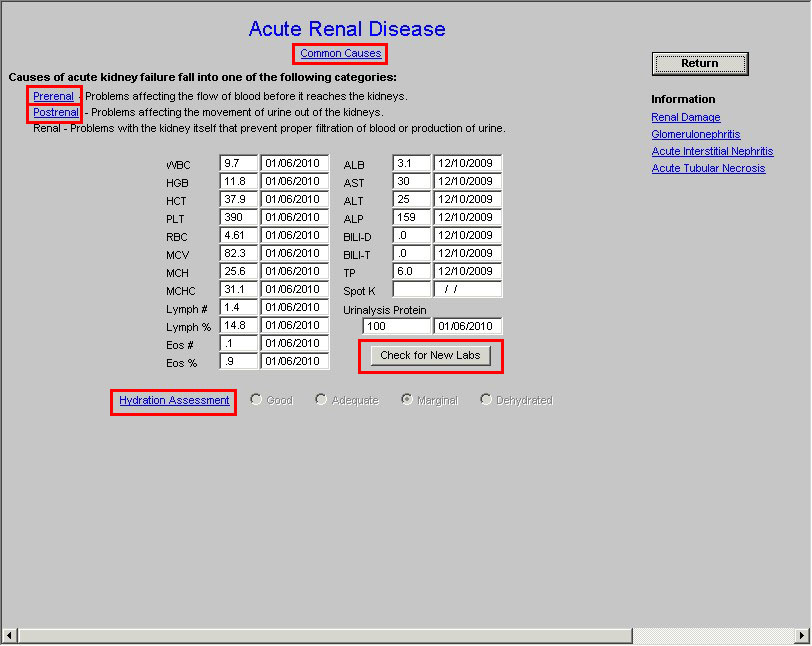
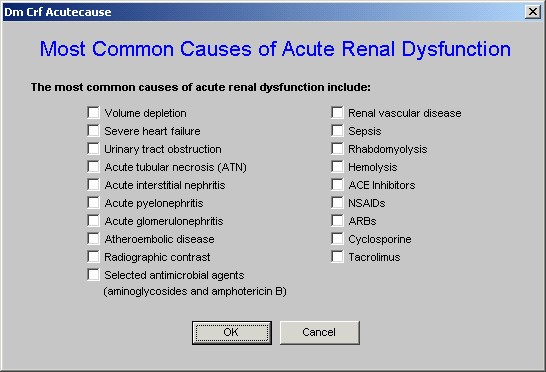
At the top of the Acute Renal Disease template is a button entitled “Common Causes.” When this button is launched a template is deployed which is entitled “The Most Common Causes of Acute Renal Dysfunction.” It is possible for a patient to have more than one of these causes simultaneously and this tool makes it possible to designate as many as apply to the patient.
Below the “Common Causes” button is a section which discusses the three categories of acute renal failure. They are:
Prerenal – this is defined as “Problems which affect blood flow before it reaches the kidney.” When this button is deployed the following pop-up appears.
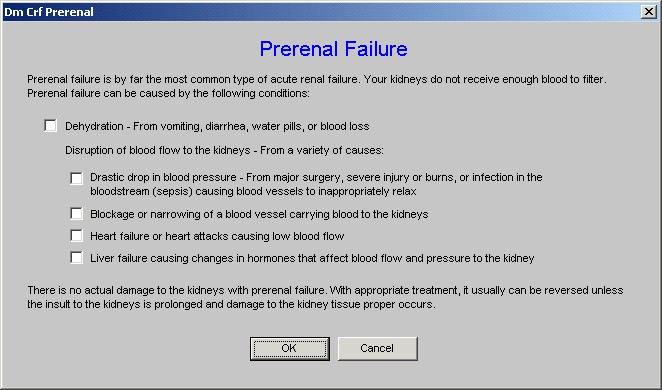
This pop-up makes it possible to designate what the causes of the patient’s decrease in renal function are. There can be more than one affecting a patient at any given time.
Postrenal – this is defined as “Problems affecting the movement of urine out of the kidney.”
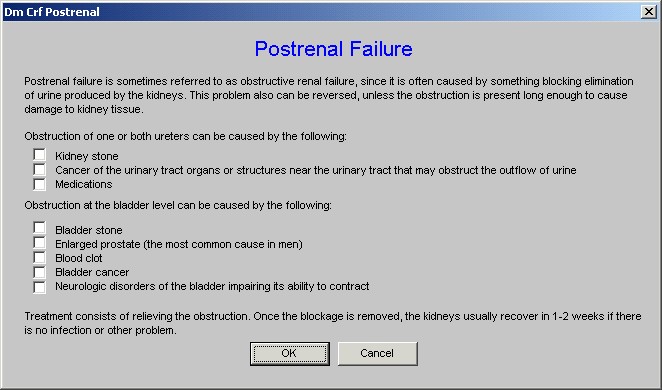
This pop-up addresses the location of obstructions which affect the flow of urine out of the kidney and allow for the documentation of the problem which affects this patient.
Renal – this is defined as “Problems with the kidney itself that prevent proper filtration of blood or production of urine.”
On the Acute Renal Disease Template, after the definitions of prerenal, postrenal and renal disease, there is a display of all laboratory values which relate to kidney function. At the bottom of the second column of lab values, there is a button entitled “Check for New Labs,” which allows you to update the presentation of current labs.
This is followed by a link to the Hydration Template. When the Hydration Assessment has been completed, the results of the level of hydration of the patient is displayed on this template. And, there is a button entitled, “Check for new labs,” which allows the system to check for new laboratory values.
Finally, to the right of the Acute Renal Disease template there are four “information” buttons which launch documents about:
- Renal Disease
- Glomerulonepritis
- Acute Interstitial Nephritis
- Acute Tubular Necrosis
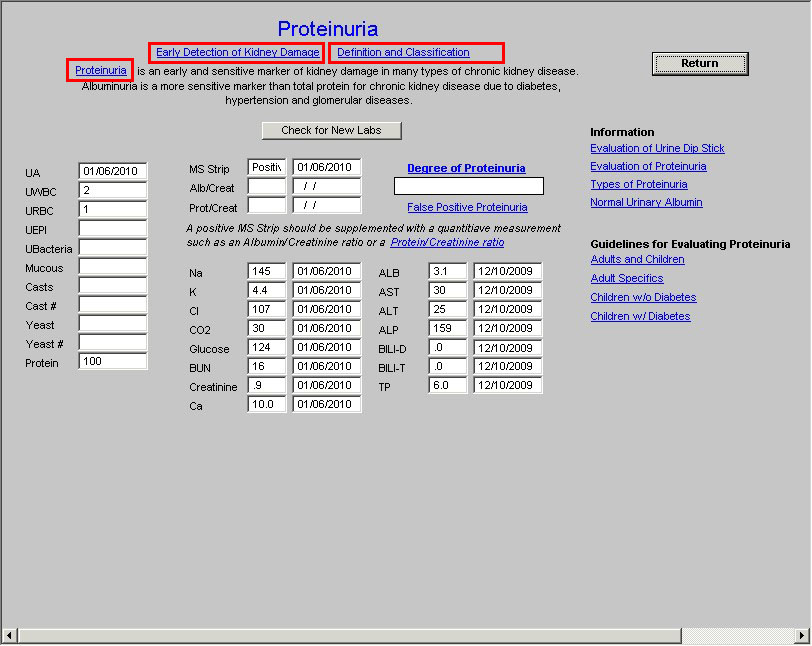
At the top of the Proteinuria template are two buttons which give information about the early detection of kidney damage and definitions of proteinuria and albuminuria.
The first button is entitled “Early Detection of Kidney Damage.” When it is launched the following is displayed.
Early Detection of Kidney Damage
- Early detection: Persistently increased urinary excretion of protein is a sensitive marker of kidney damage. Early detection allows more timely introduction of therapy to slow disease progression.
- Albuminuria is more sensitive marker for adults with CKD due to diabetes, hypertension, and glomerular diseases than total protein.
- NKF recommends random spot urine measurements due to the inconvenience and errors associated with timed- urine samples.
- First morning specimens are preferred: if not available, random specimens are acceptable
- If 1+ protein, assess total protein-to-creatinine ratio or albumin-to-creatinine ratio within 3 months.
The second button is entitled “Definitions of Proteinuria and albuminuria.” When this button is activated, the following information appears.
The next hyperlink on this template is entitled Proteinuria and when launched, it displays the following information:
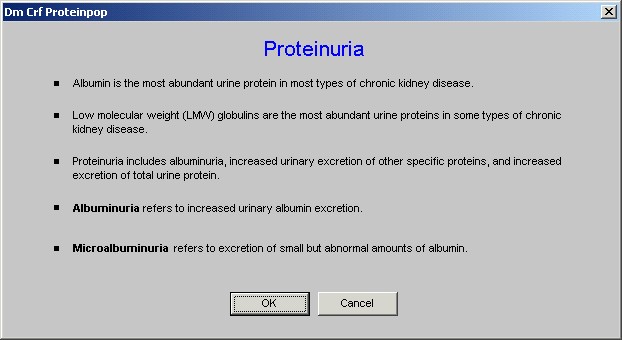
After the hyperlink entitled Proteinuria, there are two facts about proteinuria which are very important:
- Protein is an early and sensitive marker of kidney damage in many types of kidney disease.
- Albuminuria is a more sensitive marker than total protein for chronic kidney disease due to diabetes, hypertension and glomerular disease.
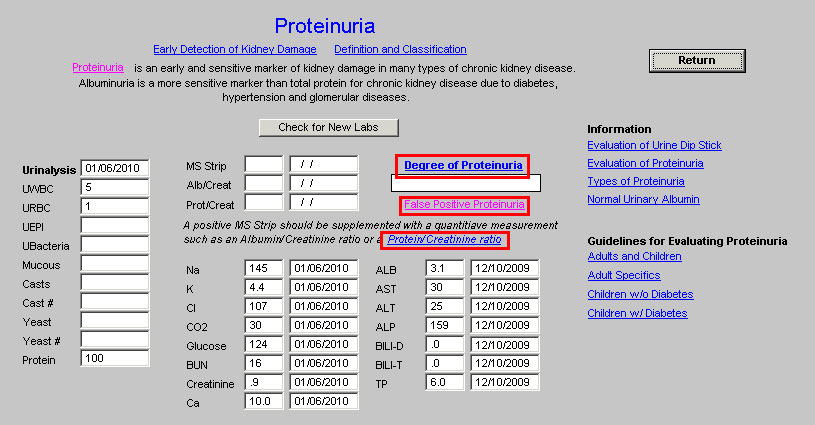
Following these statements, there is a box in which the “degree of proteinuria” is automatically documented.
Note: In order for the “degree of proteinuria” to be calculated an albumin/creatinine ratio or a protein/creatinine ratio must be documented in the lab values.
Above the box entitled “degree of proteinuria,” there is a button of the same name, which when launched displays the following information:
normal: < 150 mg/24hr
microalbuminuria: 30-300 mg/24 (specifically albumin; usually measured in diabetics)
trace proteinuria: 150 to 500 mg/24 hr
mild proteinuria: 500 mg to 1 g/24 hr
moderate proteinuria: 1-3 g/24 hr
nephrotic range proteinuria: > 3 g/24 hr
Beneath the box in which “degree of proteinuria” is displayed, there is a button entitled, “False Positive Proteinuria.” When this button is clicked, the following pop-up is displayed.
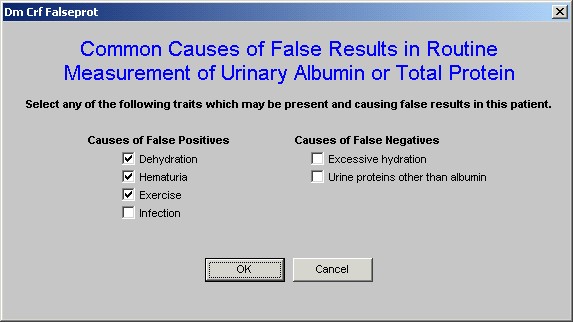
This allows the provider to document the presence of any condition which might influence the measurement of urinary protein and which might give a false value.
Below the Degree-of-Proteinuria box, there is a caution about the MS Strip or Micral Strip. See it below outlined in red.
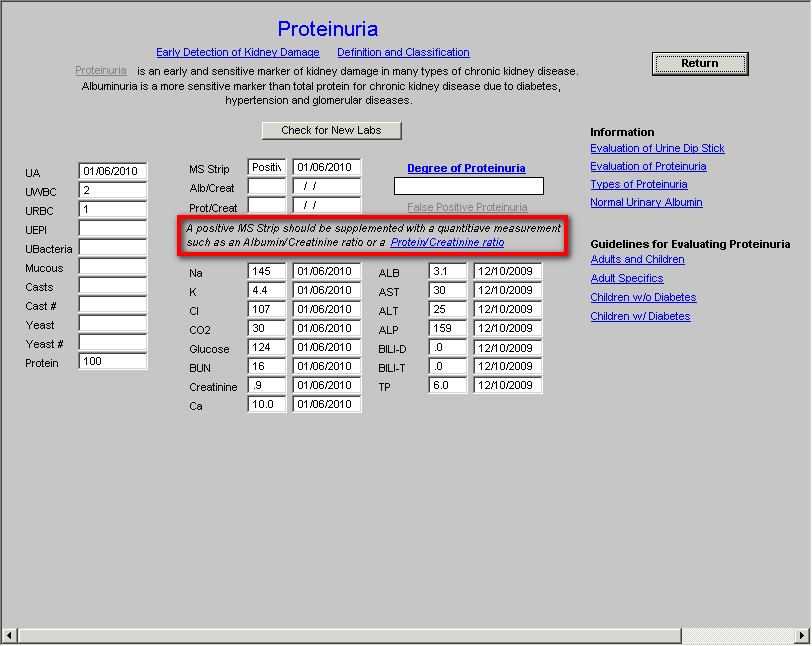
A hyperlink is attached to the phrase “Protein/Creatinine Ratio,” which when launched displays the following:
Spot protein/creatinine ratio estimates 24-hour excretion of protein in grams/24 hr. To perform the test, a random urine sample is submitted to the laboratory for protein concentration (in mg/dL) and creatinine concentration (in mg/dL). The protein/concentration is divided by the creatinine concentration, and the unit-less number is the estimated daily protein excretion in gm/24 hrs. An abnormal ratio is >0.15, which estimates a 24 hour protein excretion of >150 mg/day (>0.15 gm/day). Many nephrologists recommend using protein/creatinine ratios to quantify protein excretion instead of a 24 hour urine collection.
Beneath this information is a display of 15 lab values pertinent to Proteinuria evaluation.
To the right of this information there is a series of information buttons which launch documents on:
- Evaluation of Urine Dip Stick
- Evaluation of Proteinuria
- Types of ‘Proteinuria
- Normal Urinary Albumin
Followed by a series of articles entitled “Guidelines for Evaluating Proteinuria.”
- Adult and Children
- Adult Specific
- Children without Diabetes
- Children with Diabetes
This template addresses the value of GFR as a measure of kidney function; it is simple and straightforward in its use.
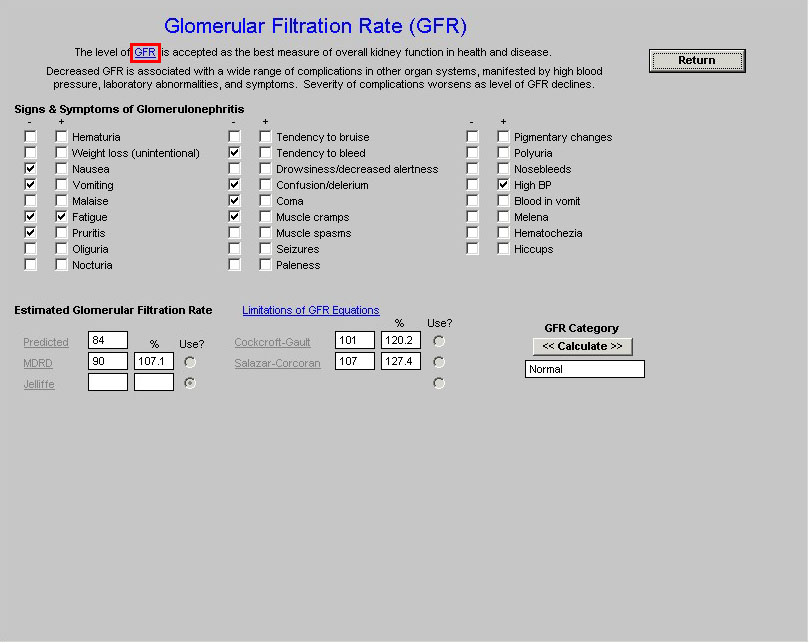
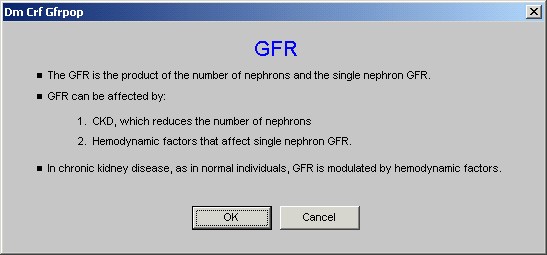
The hyperlink attached to GFR in the first sentence on this template addresses the two ways in which GFR can be affected. When launched the pop-up associated with this hyperlink states:
The remainder of this template is self-explanatory.
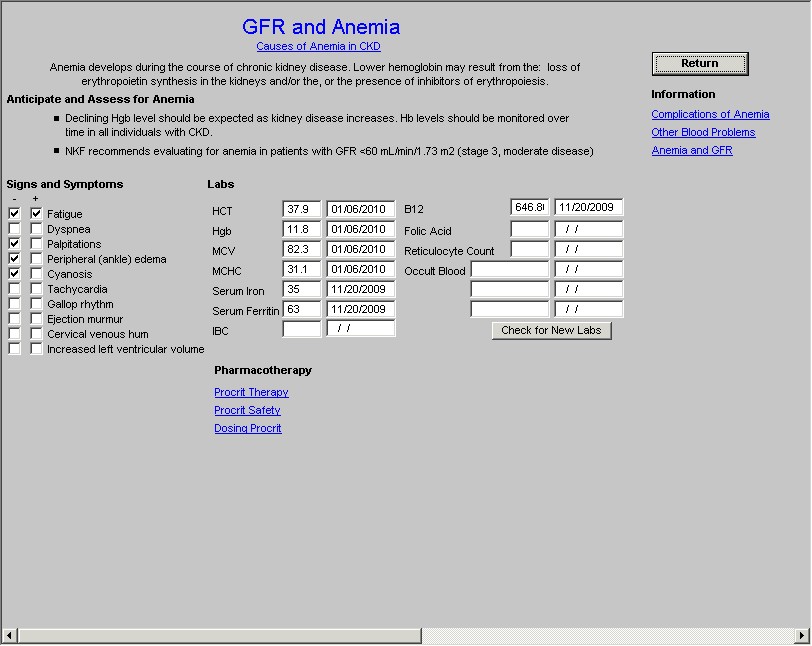
The first button on this template is entitled “Cause of Anemia in CKD.” When this button is clicked, the following pop-up appears on which the known causes of anemia can be documented:
The remainder of the GFR and Anemia is self explanatory. The theory of therapy with Procrit is explained in three documents and there are three documents which address anemia and GRF.
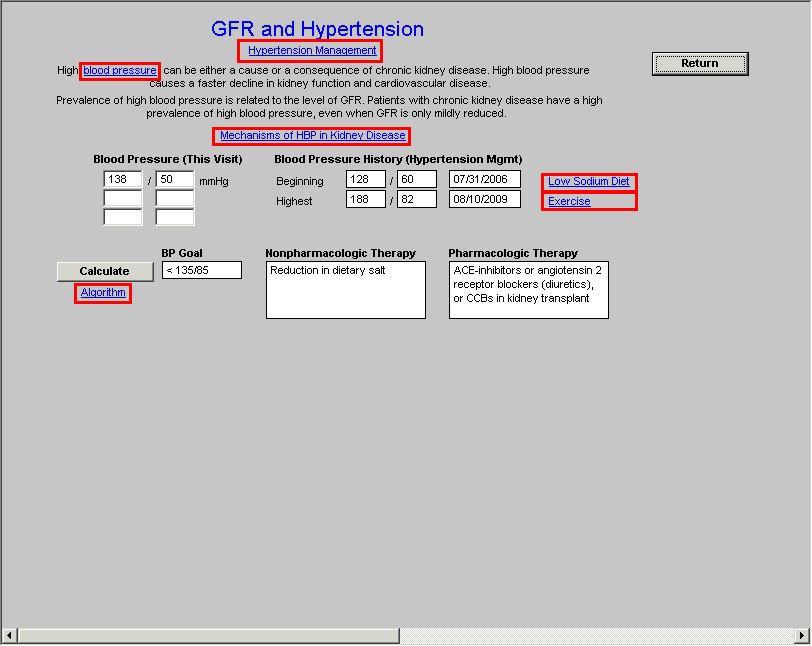
This template displays information about the presence and activity of high blood pressure in patients with renal disease.
There are six hyperlinks on this template.
- “Hypertension” at the top of the template. deploys SETMA’s Hypertension Disease Management Tool
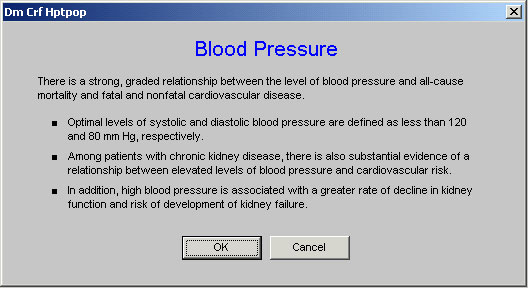
- “Blood Pressure” – deployment of this hyperlink displays the following pop-up which presents three important facts about high blood pressure in patients with chronic kidney disease.
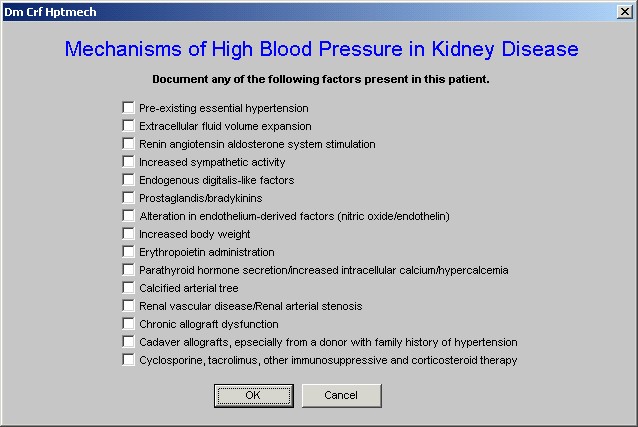
- “Mechanisms of HBP in Kidney Disease.” – this button deploys the following pop-up.
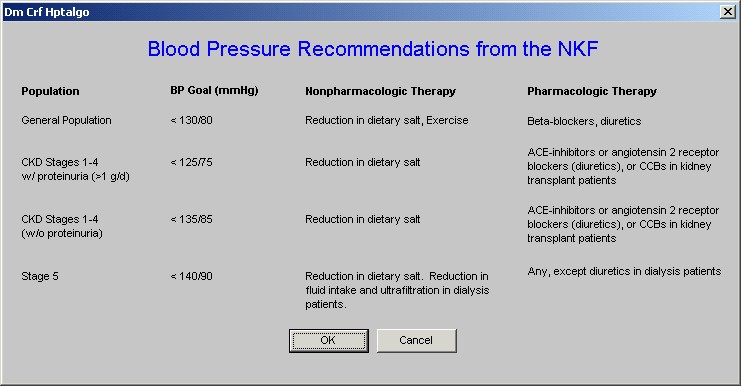
- “Algorithm” which launches a pop-up entitled “Blood Pressure Recommendations from the NKF.”
- “Low Sodium Diet” – this button produces a printable low sodium diet.
- “Exercise” – this button deploys SETMA Exercise Prescription template.
On the GFR and Hypertension template, there is also a button entitled “Calculate.” When that button is activated, it completes the following information for this patient based on the information in “Algorithm” discussed above.
- Blood Pressure Goal
- Non-pharmacologic therapy
- Pharmacologic Therapy
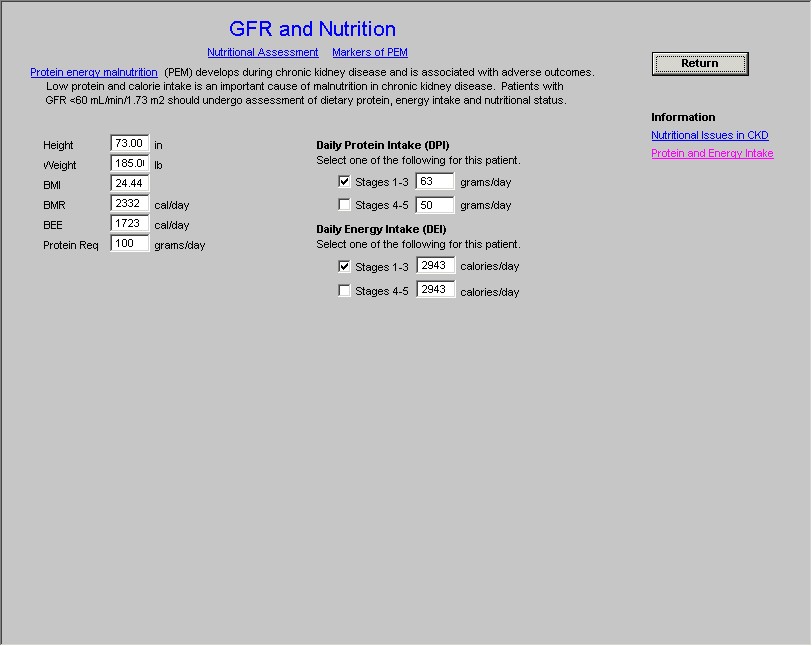
At the top of this template are two buttons:
- “Nutritional Assessment” – this is a hyperlink to SETMA’s Nutrition Assessment Template. You can review this template by clicking on this hyperlink.
- “Markers of PEM “(Protein Energy Malnutrition)
The template then displays the following (if the stage of renal disease has been calculated, it will automatically populate these fields, if it has not been you must select the stage).
- Daily Protein Intake – the NKF recommendation is based on the stage of renal disease
- Daily Energy Intake – the NKF recommendation is also based on the stage of renal disease.
There are then two information pieces which can be launched from buttons entitled:
- Nutritional Issues in
- CKD Protein and Energy Intake
This template declares that bone disease is frequently associated with Chronic Renal Disease when the GFR is below 60 ml/min/1.73 meters2
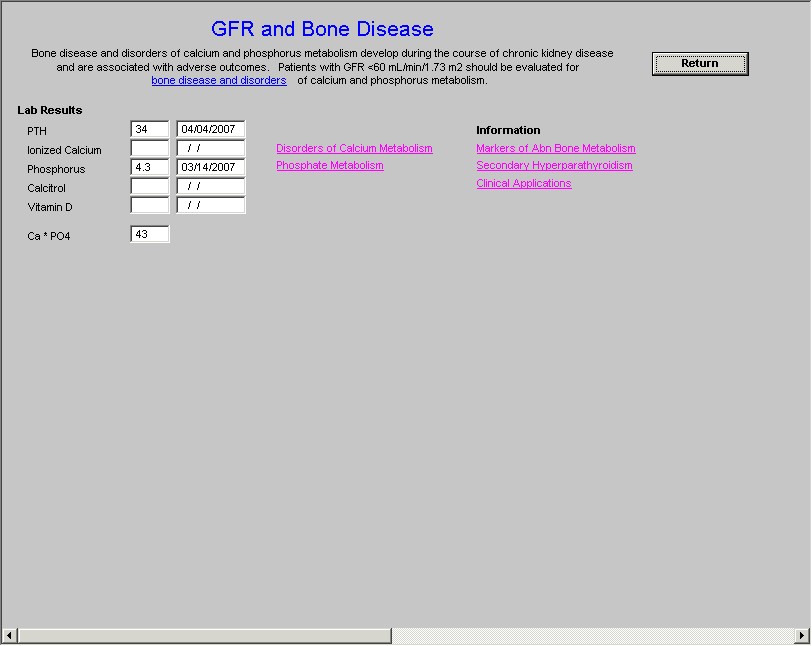
In addition to the laboratory results for chronic renal disease and bone disorders, there are six information pieces present on this template; they are:
1. Bone Disease and Disorders of Calcium and Phosphorus Metabolism
2. Disorders of Calcium Metabolism
3. Disorders of Phosphate Metabolism
4. Markers of Abn Bone Metabolism
5. Secondary hyperparathyroidism
6. Clinical Applications
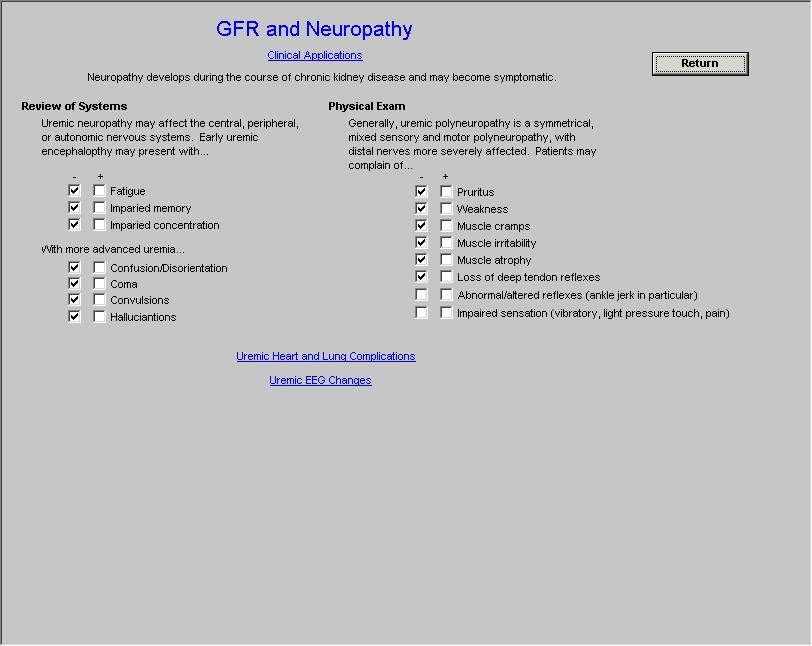
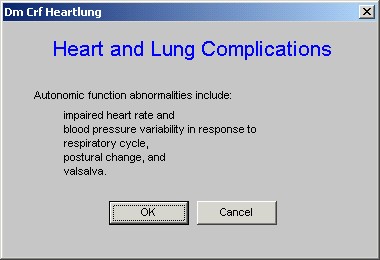
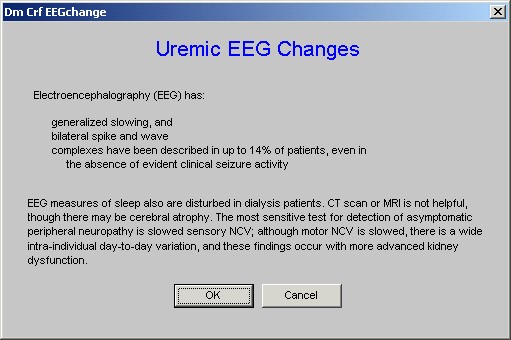
The first element on this template is entitled “Clinical Application” which launches a pop-up entitled “Uremic Neuopahty Clinic Applications.”
After this the template displays a Review of Systems and a Physical Examination which interacts with the body of SETMA’s EMR and which is specific to issues related to uremic neuropathy.
The final elements on this template are two buttons:
- Uremic Heart and Lung Complication
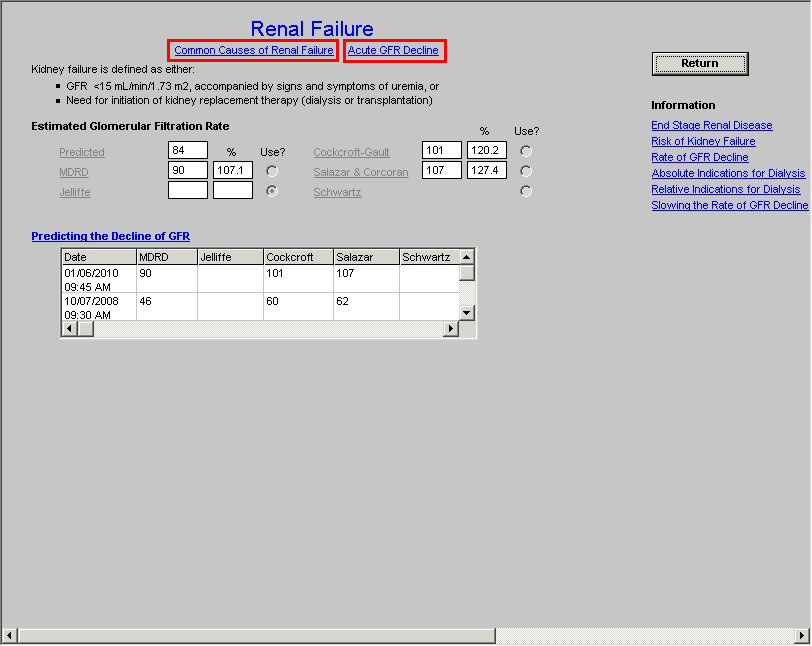
At the top of the template are two buttons:
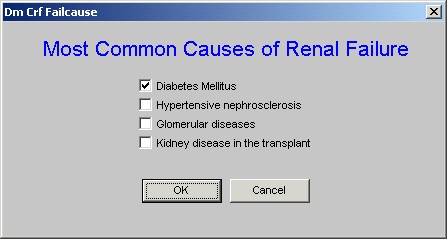
- “Common Causes of Renal Failure” when deployed this launches a template entitled “Most Common Causes of Renal Failure.”
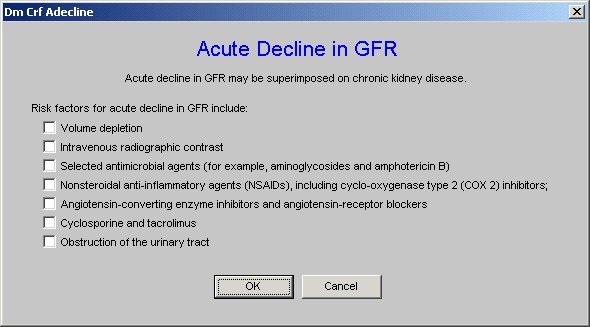
- “Acute GFR Decline” – the first statement on this template is “Acute decline in GFR may be superimposed upon chronic renal disease.”
These two buttons are followed by the definition of kidney failure. This definition is followed by the estimated GFR from the formulae discussed above.
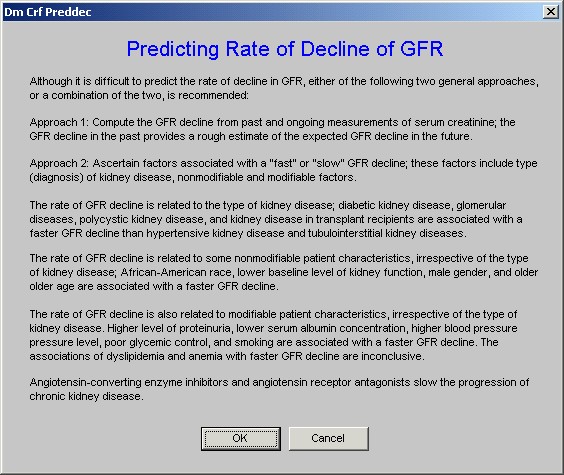
The button “Predicting the decline of GFR” launches the following template which defines how the decline in GFR can be predicted.
Finally, there is a presentation of the estimated GFR by various formulae shown overtime.
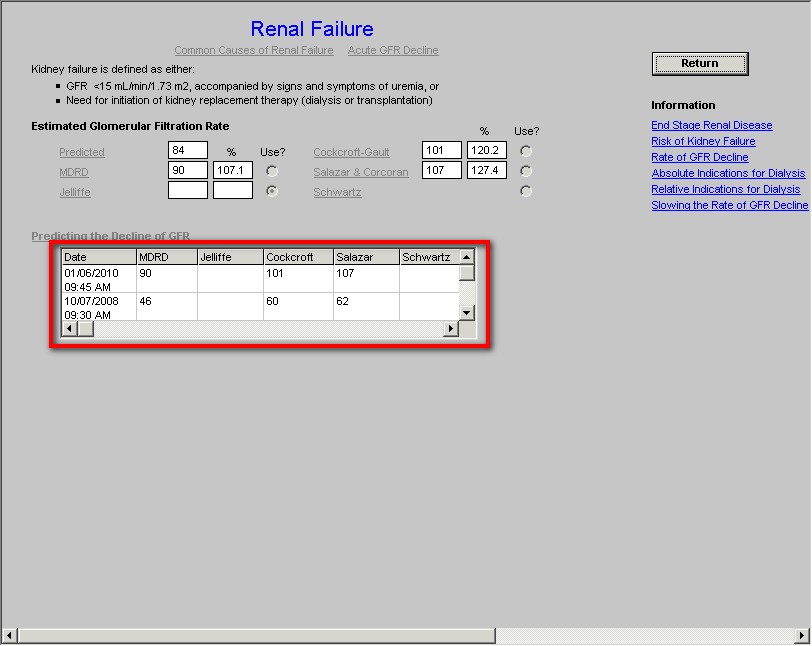
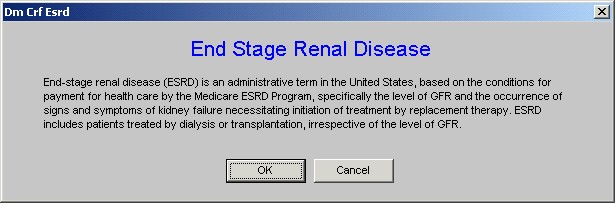
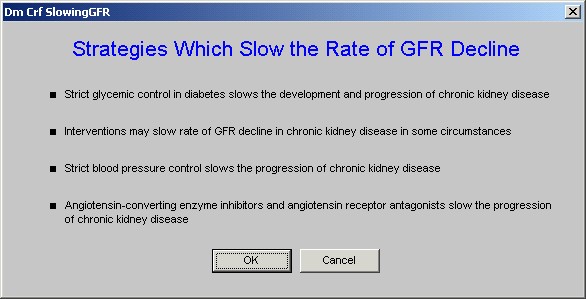
To the right side of this template are six buttons which launch education materials. They are entitled:
- “End stage of renal disease”
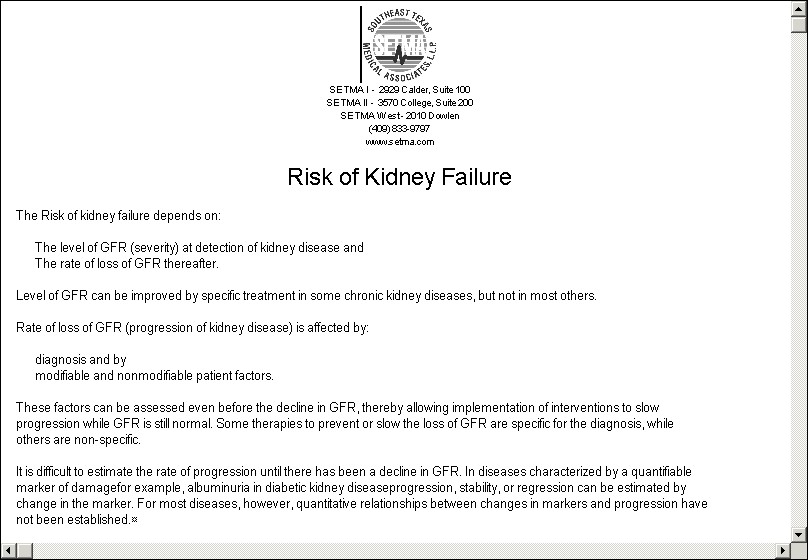
- “Risk of Renal Failure”
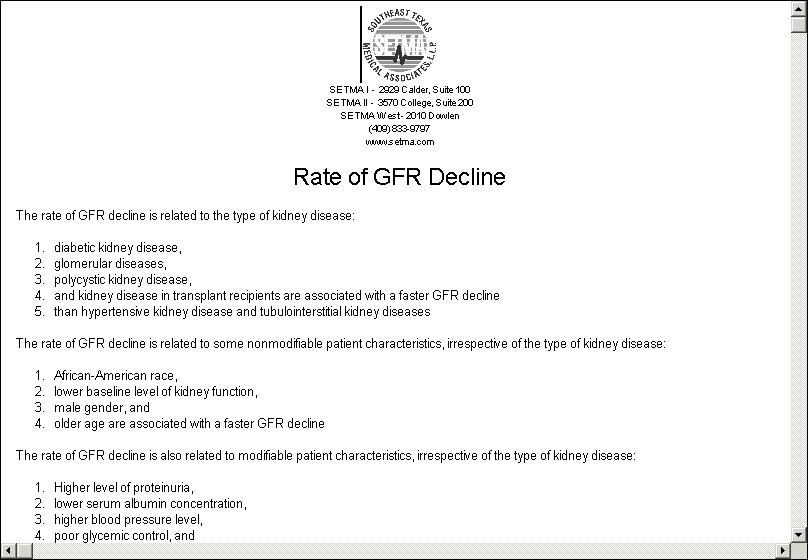
- “Rate of GFR Decline”
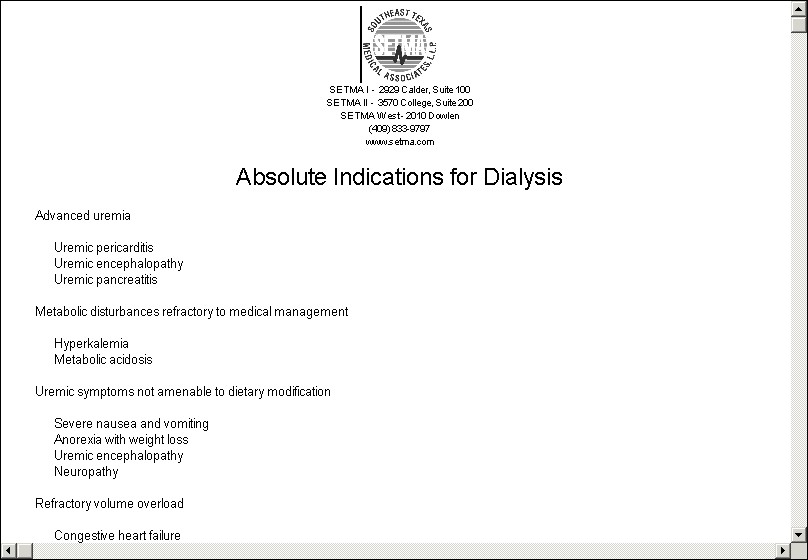
- “Absolute Indications for Dialysis”
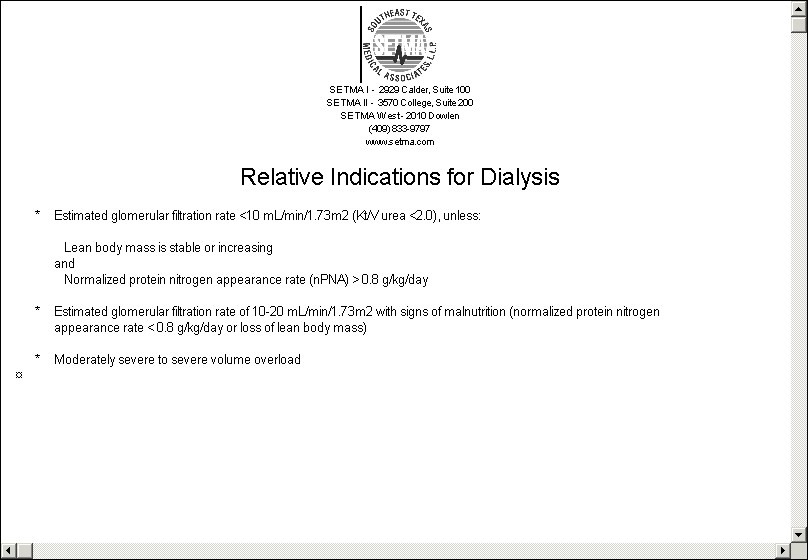
- “Relative Indications for Dialysis”
- “Slowing the Rate of GFR Decline”
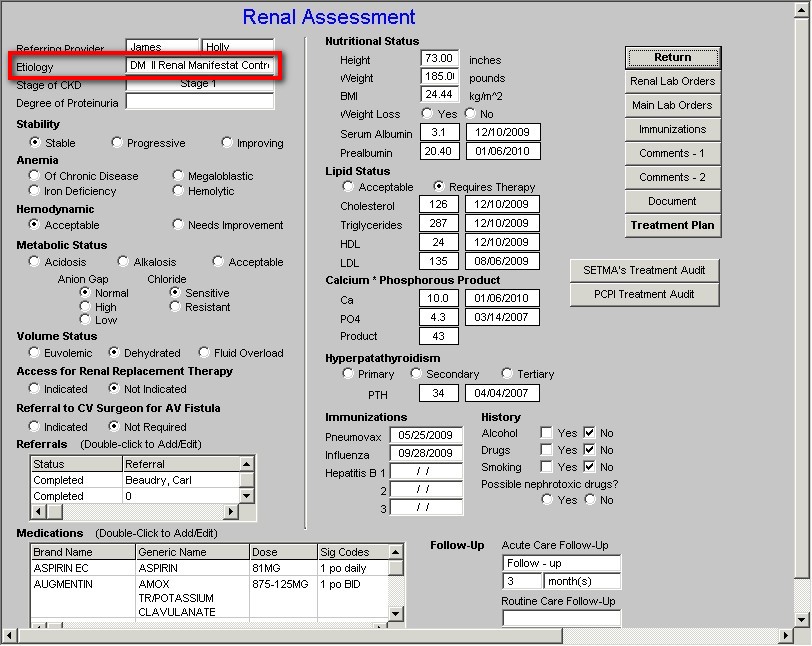
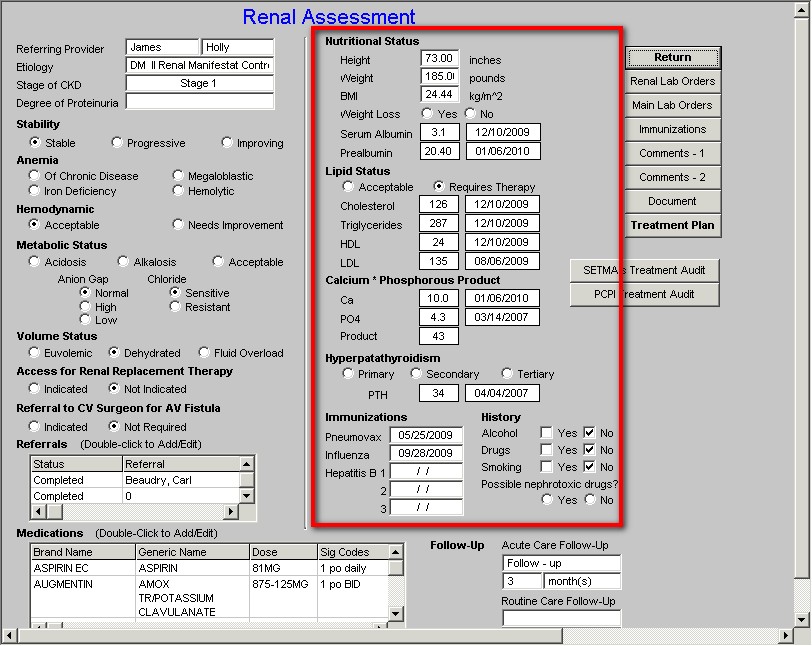
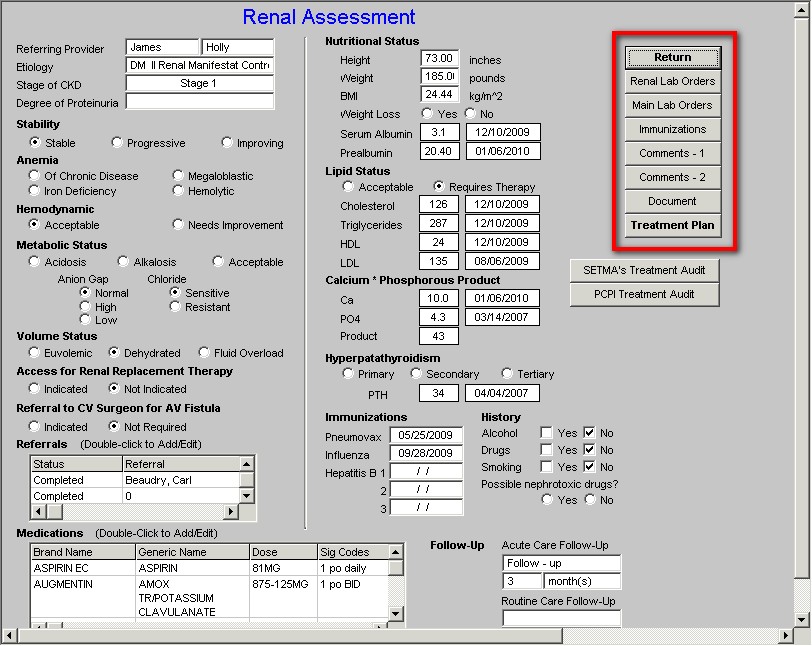
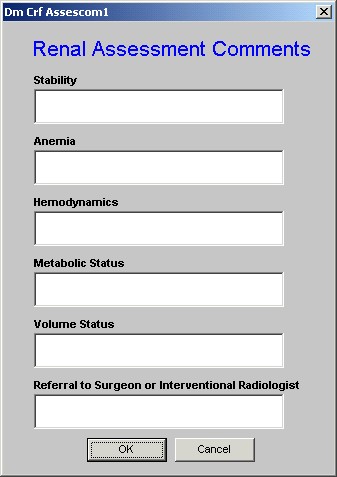
This template provides a summary of the renal evaluation of the patient and provides the ability to order testing and referrals. It is organized into three columns. .
The first four data points in the first column are automatically documented when they have been previously identified. They are:
- Referring Provider – the name of the provider completing the renal evaluation
- Etiology – from the Classification template (the automatic completion of this data point does not occur presently but will in 2010.
- Stage of Kidney Disease – from the Stage of Renal Disease template
- Degree of Proteinuria – from the Proteinuria template
It is then possible to address the following
- Stability – this requires the provider to make a judgment
- Anemia – this requires the provider to note what kind of anemia if any
- Hemodynamics – this requires the provider to note the status
- Metabolic Status including anion gap which is automatically noted if the Hydration template has been completed.
- Volume Status which is automatically noted if the Hydration template has been completed.
- Access for Renal Replacement Therapy – if the patient has renal stag I-III this will be automatically noted as not applicable
- Referral to CV Surgeon or Interventional Radiologist for AV Fistula – if the patient has renal stage I-III this will be automatically noted as not applicable.
A the bottom of the first column are the following functions:
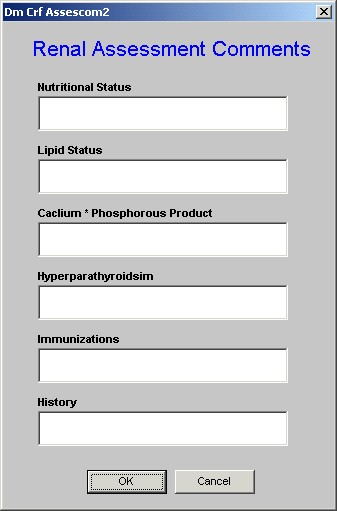
In the second column, it is possible to address the following issues in the care and condition of the patient with Chronic Renal Disease
In this column, the following data is automatically aggregated for review of the patient with renal disease
1. Nutritional Status including
- Height
- Weight
- BMI
- Serum Albumin
- Pre-albumin
- Weight Loss
2. Lipid Status
3. Calcium times Phosphorus Product
4. Hyperparathyroidism
5. Immunization
6. History
- Alcohol
- Drugs
- Smoking
- Neprhotoxic drugs
In the third column, the following functions appear:
- Return – this is a navigation button which returns you to the Master Renal Template.
- Renal Lab Orders – this is a copy of the endocrine lab orders and allows you to order any of these specialized tests
- Main Lab Orders – this is a copy of the main lab order template and allows you to order any of the lab tests which are there.
- Immunizations – this links you to the ability to order immunizations
- Comment I – this allows you to add more detailed comments about elements of column I
- Comment II -- this allow you to add more detailed comments about elements of Column I and II
- Document – this produces a document for the Renal Suite of templates
- Treatment Plan -- This button generates the Plan of Care and Treatment Plan for the Renal Suite of Templates which should be given to the patient at least once a year. The following is an example of a real patient. This patient’s document illustrates the function of each of the templates in this suite particularly of anemia, nutrition, bone health, renal failure and it gives the patient information about how to improve their kidney health.
Beneath the Treatment Plan Button two Audit buttons two additional buttons appear:
- SETMA’s Treatment Audit – because no national agency – PCPI, NQF, NCQA, NQF, AQA, HEDIS or other – has published a renal quality audit for Chronic Renal Disease Stage I-III, SETMA designed its own. This is it.
- PCPI Treatment Audit
The first is SETMA’s Renal Audit. This is an audit tool which SETMA developed to evaluate the care which patients with Stage I-III Renal Disease should be receiving. The second is the PCPI Renal which is the Physician Consortium for Performance Improvement Data Set for evaluating the quality of care which patients with Stage IV & V Renal Disease are receiving

The key to the elements of this audit are:
- The elements in black apply to this patient and have been fulfilled.
- The elements in grey do not apply to this patient.
- The elements in +red apply to this patient and have not been fulfilled.
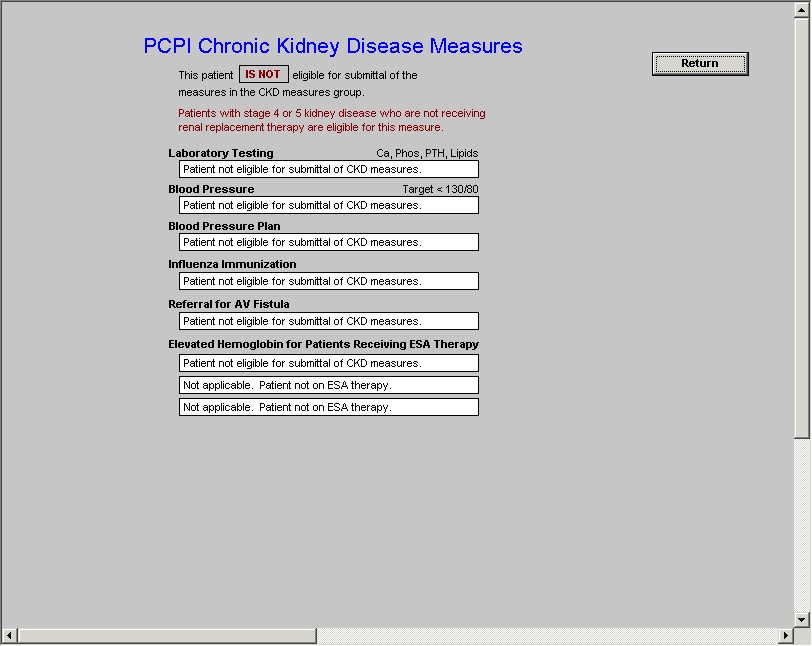
The PCPI Chronic Renal Disease quality measurement set is identical to the PQRS measures for the same condition.
The last button on the Master Chronic Renal Failure template is entitled “Physician Information.” It is outline in red below.
When the navigation button “Physician Information” is deployed the following appears:
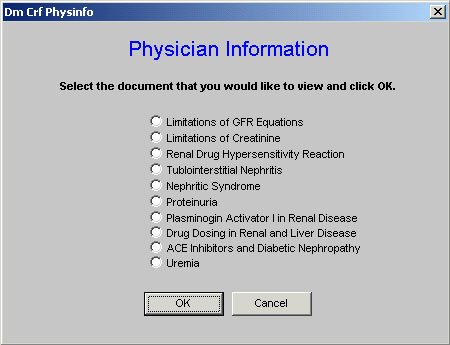
This function provides for healthcare provider information on the following subjects. Any of these documents is launched by checking the box next to the title and the clicking “OK.”
- Limitations of GFR Equations
- Limitations of Creatinine
- Renal Drug Hypersensitivity Reaction
- Tublointerstitial Nephritis
- Nephritic Syndrome
- Proteinuria
- Plasminogen Activator I in Renal Disease
- Drug Dosing in Renal and Liver Disease
- Ace Inhibitors and Diabetic Nephropathy
- Uremia
After completing the review of a patient’s renal status and an analysis of their present renal condition, the following Treatment Plan and Plan of Care, which is personalized with the individual patient’s data, can be completed with the click of a button.
Particularly in regard to the standards of Patient-Centered Medical Home recognition by NCQA and generally in regard to the standards of excellence of care, a written, personalized Treatment Plan and Plan of Care is critical to the patient’s care. This document completes the cycle:
- The patient makes an appointment
- The provider completes a history and physical examination
- Tests and procedures are ordered
- The results are analyzed
- A Treatment Plan and a Plan of Care is prepared
- This document is given to the patient.
- This document becomes the foundation of the patient’s education and the provider’s conversation with the patient about their health and their care.
The following Plan of Care and Treatment Plan is from a real patient who was seen in SETMA’s clinic. The patient’s identify has been removed.
 |
| SETMA I - 2929 Calder, Suite 100 |
| SETMA II - 3570 College, Suite 200 |
| SETMA West - 2010 Dowlen |
| (409) 833-9797 |
| www.jameslhollymd.com |
|
| Renal Follow-Up Note Treatment Plan and Plan of Care |
|
|
| Patient | |
| Date of Birth | |
| Age | 62 years |
| Ethnicity | Caucasian |
| Sex | M |
| Encounter Date | 01/06/10 |
|
|
|
Follow-Up Care
Your next visit should be scheduled in 3 month(s)
Latest Lab Results
|
|
| CBC | | |
| WBC | 9.7 K/uL | 01/06/2010 |
| HGB | 11.8 g/dL | 01/06/2010 |
| HCT | 37.9 % | 01/06/2010 |
| PLT | 390 h/uL | 01/06/2010 |
| RBC | 4.61 M/uL | 01/06/2010 |
| MCV | 82.3 fl | 01/06/2010 |
| MCH | 25.6 pg | 01/06/2010 |
| MCHC | 31.1 g/dL | 01/06/2010 |
| Lymph## | 1.4 K/uL | 01/06/2010 |
| Lymph% | 14.8 % | 01/06/2010 |
| Eos## | .1 K/uL | 01/06/2010 |
| Eos% | .9 % | 01/06/2010 |
|
|
| Urinalysis | 01/06/2010 |
| Color | Yellow |
| Clarity | Clear |
| pH | 6.50 |
| Spec Grav | 1.025 |
| Glucose | Normal |
| URO | |
| Ketones | Negative |
| Leukocytes | Negative |
| Nitrates | Negative |
| Bilirubin | Negative |
| Blood | Negative |
| Protein | 100 |
|
|
| BMP | | |
| Na | 145 mmol/L | 01/06/2010 |
| K | 4.4 mmol/L | 01/06/2010 |
| Chloride | 107 mmol/L | 01/06/2010 |
| CO2 | 30 mmol/L | 01/06/2010 |
| Glucose | 124 mg/dL | 01/06/2010 |
| BUN | 16 mg/dL | 01/06/2010 |
| Creatinine | .9 mg/dL | 01/06/2010 |
| Ca | 10.0 | 01/06/2010 |
|
|
| CMP | | |
| ALB | 3.1 g/dL | 12/10/2009 |
| AST | 30 u/L | 12/10/2009 |
| ALT | 25 u/L | 12/10/2009 |
| ALP | 159 u/L | 12/10/2009 |
| BILI-D | .0 mg/dL | 12/10/2009 |
| BILI-T | .0 mg/dL | 12/10/2009 |
| TP | 6.0 g/dL | 12/10/2009 |
|
|
| Thyroid | | |
| T3 | 1.34 ng/mL | 12/02/2009 |
| T4 | 6.95 ng/dL | 12/02/2009 |
| T7 | .14 | 12/02/2009 |
| TSH | .49 uIu/mL | 12/02/2009 |
| T-Uptake | 1.97 TBI | 12/02/2009 |
|
|
| Lipids | | |
| Cholesterol | 126 mg/dL | 12/10/2009 |
| HDL | 24 mg/dL | 12/10/2009 |
| CHOL/HDL Ratio | 5.25 | |
| LDL | 135 mg/dL | 08/06/2009 |
| Triglycerides | 287 mg/dL | 12/10/2009 |
|
|
| Other | | |
| Amylase | 80 u/L | 12/10/2009 |
| Lipase | 368 u/L | 12/10/2009 |
| PT | 10.1 seconds | 12/10/2009 |
| INR | 1 | 12/10/2009 |
| Ferritin | 63 ng/mL | 11/20/2009 |
| Iron | 35 ug/dL | 11/20/2009 |
| Glyco Hemoglobin | 8.1 % | 01/06/2010 |
| Mean Plasma Glucose | 211.1 mg/dL | |
| BNP | 615.00 pg/mL | 12/10/2009 |
| CPK | 58 u/L | 12/27/2007 |
| B12 | 646.80 pg/mL | 11/20/2009 |
| Digoxin | .0 ng/mL | 03/27/2009 |
| ESR | 62 mm/hr | 12/02/2009 |
| KOH | .00 | 05/14/2008 |
| Magnesium | 1.3 mg/dL | 12/10/2009 |
| Micral Strip Positive | 100mg/L | 01/06/2010 |
| Prealbumin | 20.40 mg/dL | 01/06/2010 |
| PSA | .51 ng/mL | 12/10/2009 |
| Rheumatoid Factor | 4.51 IU/mL | 08/17/2006 |
| Uric Acid | 7.0 mg/dL | 08/06/2009 |
|
|
|
Active Medications
The following are the medications which you should be taking. Please notify your provider if you are unable to obtain your medications for any reason. Do not just stop taking your medication without calling your healthcare provider immediately .
|
|
| Start Date |
Brand |
Dose |
Sig Desc |
| 01/06/2010 |
Augmentin |
875-125mg |
one by mouth twice daily |
| 01/06/2010 |
Tussionex |
10-8mg/5ml |
1/2 to 1 tsp every 12hrs |
| 12/28/2009 |
Fluoxetine Hcl |
20mg |
Take one capsule by mouth daily |
| 12/28/2009 |
Lisinopril |
40mg |
1 tab po once a day |
| 12/28/2009 |
Diovan |
160mg |
1 tab po each monring |
| 12/28/2009 |
Metoprolol Tartrate |
25mg |
one by mouth twice daily |
| 12/28/2009 |
Aspirin Ec |
81mg |
1 by mouth daily |
| 12/28/2009 |
Crestor |
20mg |
1 tab po once a day |
| 12/28/2009 |
Levemir |
100/ml |
75 units sub q in the morning and 85 units in the evening |
| 12/28/2009 |
Novolog |
100/ml |
45 units with meals |
| 12/28/2009 |
Nitrostat |
0.4mg |
take one tablet under tongue to dissolve, every 5 minutes up to 3 times a day |
| 12/28/2009 |
Lasix |
20mg |
Take one tablet by mouth daily |
| 12/28/2009 |
Plavix |
75mg |
1 tab po daily |
| 12/28/2009 |
Vicodin Es |
7.5-750mg |
1 tab q4-6h as needed for pain |
Please review this list of your medications. If any medication you are taking is missing -- if you have medications which are not listed please bring that to your healthcare provider's attention.
Stage of Renal Disease
According to your most recent laboratory evaluation, you have Stage 1 renal disease.
Hydration
Risk Factors for Dehydration Present
Recent infection - Lungs
Diabetes Mellitus, Patient on diuretics, Age over 60 years,
Physical Signs and Symptoms of Dehydration Present
Skin Turgor - good, Buccal Mucosa - moist,
Chemical and Metabolic Inidicators of Dehydration
Urine Spec Grav - .000
Glucose - 357.0 mg/dL
Sodium - 140.0 mg/dL
Potassium - 3.7 mmol/L
Chloride - 100.0 mmol/L
HCO3 - 30.0 mmol/L
Blood Urea Nitrogen - 12 mg/dL
Creatinine - .8 mg/dL
BUN/Creatinine Ratio - 15.0
Serum Osmolality - 311.5
Serum Osmolarity - 304.1
Anion Gap - 10.0
Est. Creatinine Clearance - 113.9
Hydration Status - Marginal
Hypertension
You have high blood pressure. Your last blood pressure was 138 / 50 mmHg . Your blood pressure places you into a High-Normal (Pre-Hypertensive) and into a Group C - High Risk Risk group and risk category. Hypertension (elevated blood pressure) is both a cause of kidney disease and it is caused by kidney disease. To decrease the rate of decline of your kidney function, your blood pressure must be controlled. The most effective ways of doing this is by losing weight, decreasing the salt content of your diet, increasing your exercise and by taking your medication as directed. Other methods will be discussed with you by your healthcare provider.
Diabetes
You have diabetes mellitus which is one of the most common causes of kidney disease. Controlling your blood sugar is critical to decreasing the rate of decline of your kidney function.
Your Last Hemoglobin A1C was 8.1 %. The ideal result is below 6.0%. You need to take measures to maintain your Hemoglobin A1C at or below 6.0%
Cardiovascular Disease
You have been diagnosed with cardiovascular disease. Controlling your heart disease includes controlling your blood pressure, your diabetes, your weight and maintaining an active life style with regular, daily exercise. Your healthcare provider will discuss other steps to help control your heart disease.
Protein in the Urine
You have protein in your urine. This is the earliest evidence of kidney disease and needs to be treated. The best treatment is a class of medications call ACE Inhibitors or ARBs. You are currently on an ARB, DIOVAN, and should continue that medication.
Anemia
Your most recent hemoglobin is 11.8 g/dL. This shows that you are not anemic.
Smoking
Smoking is harmful to every system of your body and particularly to your kidneys. Our records indicate that you smoke. You must stop. Remember, you can smoke or you can live; you just can't do both.
Elevated Cholesterol
Your last lipid analysis shows that your total cholesterol was 126 mg/dL, your good cholesterol (HDL) was 24 mg/dL and your bad cholesterol (LDL) was 135 mg/dL. These values place you at high risk of cardiovascular disease and at increased risk of worsening of your kidney disease.
Nutrition
While excessive weight is detrimental to your kidney’s health, so is malnutrition. While controlling your weight, or even losing weight if you are obese, is important in improving your kidney function, malnutrition is not. With your BMI you should typically be taking in 100 gms of protein each day and 2332 calories of food. However, the National Kidney Foundation’s recommendation for protein intake for a person with Stage I renal disease is 63 grams/day with a recommended caloric intake of 2943 calories/day.
The decrease in protein may improve your kidney function by decreasing the demand to clear waste products of protein metabolism from the blood while the increase in calories reflects the need to make sure that your nutrition level is maintained and that you do not become malnourished. Because of the recommend increase in calories with kidney disease, increase in the amount and consistency in the regularity of exercise are important parts of your protection of your kidneys.
A blood test called “prealbumin” assesses your current state of nutrition. Your most recent value was 24. This indicates that your calorie intake is adequate. Remember, your calorie intake needs to be properly balanced between fats, protein and carbohydrates. You should decrease your intake of simple carbohydrates such as white bread, white rice, mashed potatoes, etc. and increase your intake of complex carbohydrates which will be found in fresh vegetables an in whole fruits.
Diet
Other conditions which can contribute to the worsening of your kidney function are a:
1. High Phosphate Diet
Phosphate is found in association with protein, especially in milk and cheese. Only a few other foods contain a lot of phosphate like wholegrain cereals, baking powder, shellfish. Other sources are convenience foods which have phosphates added by food manufacturers. The following foods are high in phosphate and should be avoided.
1. Soft drinks, soda drinks, especially cola or coke and fizzy lemonade
2. Cordials/fruit syrup beverages
3. Chocolate, sweets, candy, and anything else with a high citric acid and sugar content
4. Ice-cream
5. Skim milk powder (often added to processed foods)
6. Biscuits, cookies, cakes from the supermarket
7. Tomato ketchup
8. Mayonnaise
9. Fish fingers
10. Processed cheese, especially soft cheese spread
11. Frozen pizzas
12. Hot dogs
13. Processed meats
14. Baking powder and self-raising flour often contains phosphate aerator
15. Avoid all foods that list as an ingredient mineral salts, emulsifiers and lecithin.
2. High Protein Diet
While your BMI would suggest that you need 100 grams/day of protein and 2332 calories/day, as your kidney function decreases you will need to decrease your protein intake. The National Kidney Foundation recommendation for protein intake for a person with Stage 1 renal disease is 63 grams/day with a recommended caloric intake of 2943 calories/day. From the brief list below, you can see how you will need to modify your diet to reach these goals.
1. Soy protein isolate - 80 grams protein per 100 grams
2. Soybeans, dry, roasted - 89.6 grams protein per 100 grams
3. Peanuts (raw) - 55 grams protein per 100 grams
4. Hamburger patty, 4 oz - 28.5 grams protein
5. Steak, 6 oz - 42 grams
6. Most cuts of beef - 7 grams of protein per ounce
7. Chicken breast, 3.5 oz - 30 grams protein
8. Chicken thigh - 10 grams (for average size)
9. Drumstick - 11 grams
10. Wing - 6 grams
11. Chicken meat, cooked, 4 oz - 35 grams
A professionally trained nutritionist will help plan a diet and moderate your protein intake in order to slow the rate of decline of your kidney function.
Lifestyle Changes
Because so many of these risk factors are associated with your diet, we have referred you to Medical Nutrition Education for explanation of the following dietary approaches to improving your kidney function, your weight and your overall health. SETMA's registered nutritionist will discuss with you:
Cholesterol Control
Moderation of Salt Intake
Moderation of Protein Intake
Dietary Implications of Kidney Disease
DASH Diet (Dietary Approach to Stop Hypertension)
Weight Maintenance
Immunizations
Because Hepatitis B and other viral infections also contribute to kidney disease, it is imperative for you to get your immunizations. Our records show that the following immunizations are out of date:
Hepatitis
Please ask your health care provider to order these immunizations for you at your next visit or call the clinic and ask to have them done.
SETMA's Chronic Kidney Disease Treatment Audit
Has the patient's urinary protein been assessed within the last year? Yes
Has the stage of the patient's renal disease been assessed within the last year? Yes
Has the patient been referred to Medical Nutrition Therapy at least once? Yes
Has the patient had lipid panel within the last year? Yes
Has the patient had a prealbumin test within the last year? Yes
Has the patient received a personalized exercise prescription within the last year? Yes
Has the patient received a weight management assessment including BMI, BMR and how to change both within the last year? Yes
If the patient smokes, have they received counseling as to stopping and been given methods of doing so? Yes
Has the patient received an immunization for influenza? Yes
Has the patient received an immunization for pneumonia? Yes
Has the patient received an immunization for Hepatitis B? No
Has the renal treatment and plan of care document been generated within the last year? Yes
PCPI Chronic Kidney Disease Measures Group
Applies to only Stage 4 and 5
Laboratory Testing
Patient not eligible for submittal of CKD measures.
Blood Pressure
Patient not eligible for submittal of CKD measures.
Blood Pressure Plan
Patient not eligible for submittal of CKD measures.
Influenza Immunization
Patient not eligible for submittal of CKD measures.
Referral for AV Fistula
Patient not eligible for submittal of CKD measures.
Elevated Hemoglobin for Patients Receiving ESA Therapy
Patient not eligible for submittal of CKD measures.
Not applicable. Patient not on ESA therapy.
Not applicable. Patient not on ESA therapy.
Lab Order Today
BMP
CBC
Glycohemoglobin
Micral Strip
Occult Blood
Prealbumin
Urinalysis
Urine, Albumin/Creatinine Ratio
Conclusion
The three most important things for you to do in order to support the health of your kidneys are:
1. Strict control of your blood sugar
2. Strict control of your blood pressure
3. ACE Inhibitors or ARBs medications
You can live successfully with kidney disease. It is a progressive condition but the earlier you begin aggressive treatment, the longer you will remain healthy.
Bring this document with you to your next visit and ask your healthcare provider to explain anything that you do not understand.
________________________________________________
James L. Holly MD
Southeast Texas Medical Associates, LLP
|
|
|