|
This template can be accessed from:
AAA Home
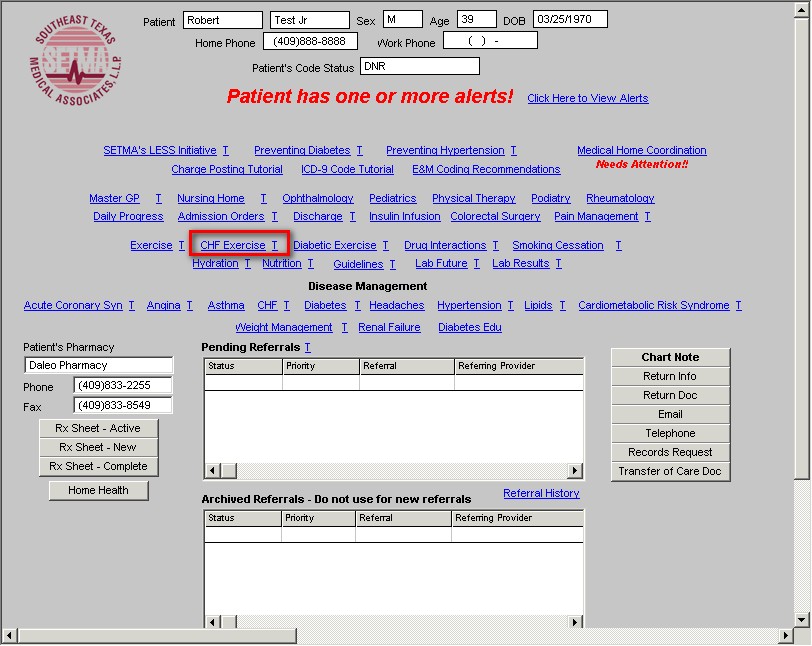
LESS Initiative
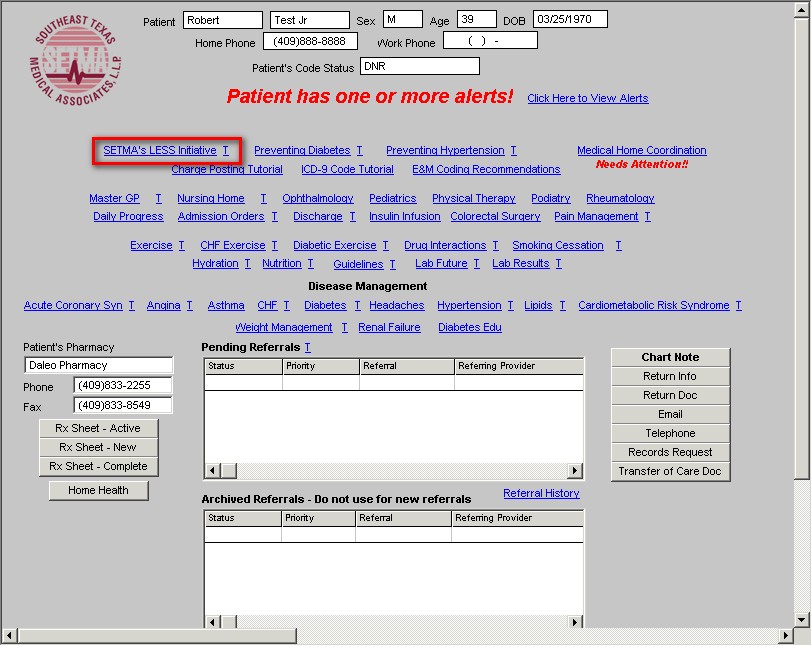
Main Tool Bar
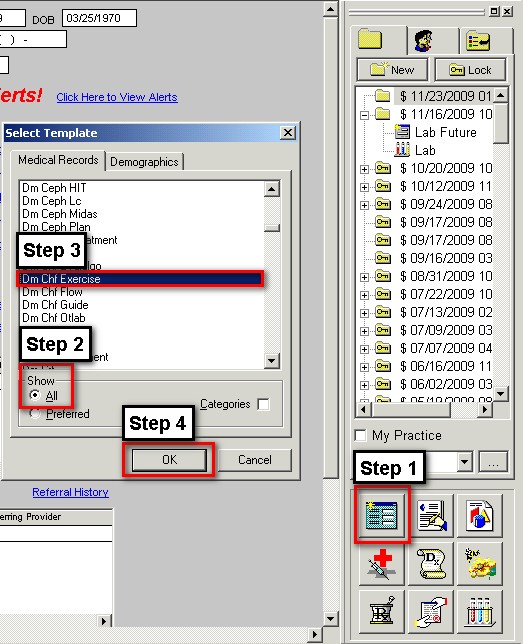
- When the Template button is clicked you will be presented with the preference list.
- If the CHF Exercise Template is listed as one of your preferences, select it.
- If it is not one of your preferences, select the All radio button and scroll down until you find it in the list. Then you may select the template by either double-clicking on the name or single click on the name (so that it is highlighted in blue) and then click the OK button.
NOTE: For more on how to set up your preferences, Click Here
The content of the template:
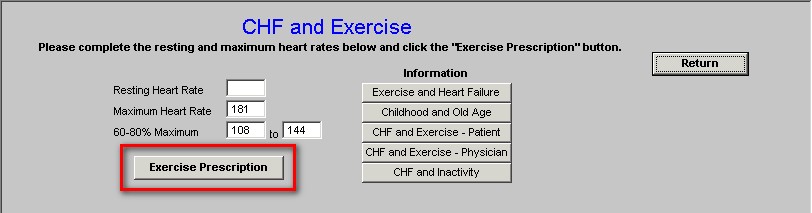
The following data is automatically populated from the patient’s nursing template
- Resting Heart Rate
- Maximum Heart Rate
- 60-80% Maximum
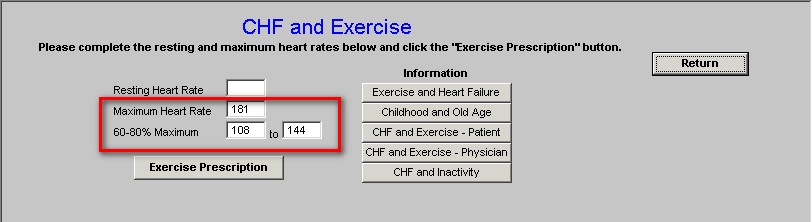
Beneath this data is a button entitled Exercise Prescription. When this button is depressed the exercise prescription for a patient with CHF or other debilitating illnesses is launched.
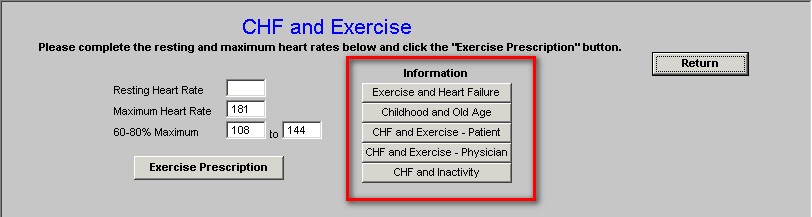
Additionally on this template are the following educational documents:
- Exercise and heart Failure
- Childhood and Old Age
- CHF and Exercise – Patient
- CHF and Exercise Physician
- CHF and Inactivity
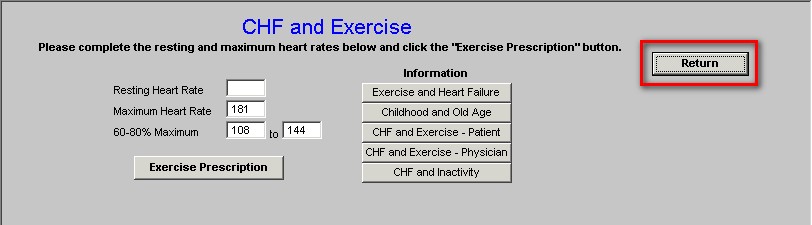
When accessed from the CHF Exercise Template or the LESS Initiative Template, there is a button to the right of the template entitled Return which when depressed returns you to the originating template.
CHF Exercise Prescription
This document contains the following information:
Part 1 –
The first section contains information about the relationship of activity and CHF.
Congestive heart failure (CHF) has been steadily increasing over the past 10 years. Lack of physical activity is considered an independent risk factor for the development of CHF. In addition, other primary risk factors include: obesity, hypertension, and diabetes.
Part 2 –
The second section gives a list of causes of CHF.
Causes of CHF
- Physical inactivity 9.2% of all cases of CHF,
- Hypertension 10.2%,
- Diabetes 3.2%,
- Obesity 8.0%.
Part 3 –
The Third Section gives information about the benefit of physical activity in patients who already have CHF.
Patients diagnosed with CHF benefit greatly from participating in exercise-training programs. For example, exercise training of patients with moderate to severe CHF:
- lowered all-cause mortality by 63% and
- reduced hospital readmission for heart failure by 71%.
The Agency for Health Care Policy and Research Guidelines on Cardiac Rehabilitation recommended exercise training for patients with chronic stable HF.
Part 4 –
This gives introductory information about the first steps and cautions about exercise in patients with CHF.
First Steps
The first step is often interval training, in which you exercise for a few minutes and then rest. This alternating pattern gives you the benefits of exercise without undue strain. Gradually you can increase the time and pace as you grow stronger. Ideally, you will eventually exercise for 30 to 40 minutes three to five times a week.
Cautions
While exercising, if you develop:
- chest pain,
- extreme shortness of breath,
- dizziness, or
- swelling of the extremities,
you should stop exercising and contact your healthcare provider immediately.
Part 5 –
This section gives information about monitoring the intensity of exercise with the heart rate.
Monitoring Exercise by Heart Rate
For improvement in your congestive heart failure, you should exercise between 50-80% of your maximum heart rate. However, if you are taking mediations which prevent your heart rate from increasing significantly, you can use Borgs Scale of Perceived Exertion for measuring your response to exercise.
Part 6 –
This gives the patient personal data about his/her own cardiac rate and exercise.
Your Personal Data
Your resting heart rate is 75.00 beats per minute and your maximum heart rate is 147 beats per minute. Therefore, your optimal exercise heart rate is between 88 and 117 beats per minute.
Part 7 –
This gives the patient information about how to measure the intensity of their exercise by their perceived response based on Borg’s Ratings of Perceived Exertion.
Borg's Ratings of Perceived Exertion (RPE)
6 |
No exertion at all |
7-8 |
Extremely light (very, very light) |
9-10 |
Very light (warm-up/recovery) |
11 |
Light |
12-13 |
Moderate |
14-15 |
Hard |
16-17 |
Very hard |
18-19 |
Extremely hard |
20 |
Maximum all-out effort with absolutely nothing being held in reserve |
The American Heart Association Committee on Exercise, Rehabilitation, and Prevention states that exercising at a Borg Scale of Perceive Exertion of 12 to 13 is usually well tolerated by the stable patient. The Borg Scale is particular useful in patients who are taking Beta Blockers which will prevent them from measuring the intensity of exercise by the increase in heart rate..
Part 8 –
This section begins to discuss the content of the exercise; it starts very slowly and builds up as endurance increases.
Duration of The Exercise
Warmup
Before exerting yourself, spend 10 minutes in slow, easy activity -- walking slowly and stretching -- to increase blood flow to your muscles. The warm-up period may need to be longer in the most debilitated patients. Usually, a period of 10 to 15 minutes is recommended. The warm up is where you very gradually increase your heart rate by stretching and walking. If you dont warm up, the risk of injury or adverse affect of exercise is increased.
Exercise
- Start with walking or stationary biking for 2 minutes at a comfortable pace. Rest for 1 minute. Repeat this five times, until you have exercised for a total of 10 minutes.
- Over 2 weeks, gradually increase the exercise period to about 4 minutes and the rest period to 2 minutes, until your total exercise time is about 20 minutes per session.
- As you become stronger, increase the exercise intervals to 5 minutes and keep the rest intervals at 2 minutes, until your total exercise time is 30 minutes per session. You can also step up your pace.
- Gradually increase the sessions to 40 minutes. You may keep or eliminate the rest stops.
- Vary your program. If you walk for exercise 1 month, for example, try a stationary bike the next. This makes workouts more interesting.
- When your healthcare provider agrees you can extend your exercise period and increase the intensity. At this point always remember the cautions mentioned above. If any of those symptoms arise, stop exercising and call your healthcare provider immediately.
Part 9 –
This section discusses the importance of the “cool down” period and the frequency of exercise.
Cool Down Period
A cool-down period is also advised. This is the reverse of the warm-up period. You gradually slow down and extend your work out until your breathing and heart rate slow down.
How Often Should I Exercise?
Most studies have used 3 to 5 times per week as the optimal training frequency. Patients who develop exhaustion after training may need a day of rest between sessions. Supplemental walking should be encouraged on the non-training days. With your healthcare providers agreement you can exercise 5-6 days a week, if you are not experiencing increasing fatigue..
Part 10 –
This adds information about the importance of weight training in patients with CHF.
Resistance (Weight) Training
Fatigue comes from the muscles inability to continue work. Fatigue can be helped by strengthening your muscles and increasing their ability to use oxygen.
- Respiratory muscle exercises to build up your chest, diaphragm, and abdominal muscles to help you breathe better.
- Resistance training that uses light weights to strengthen muscle groups in your arms, torso, and legs. Stronger muscles will reduce fatigue.
Small free weights (1, 2, or 5 lb), elastic bands, or repetitive isolated muscle training can be used. In addition, the upper body should not be ignored because many activities of daily living require arm work. These muscle groups are often neglected in exercise training. Working out with a personal trainer or getting instruction from our Physical Therapy department can help you improve your health without hurting yourself.
Resistance training using dumbbells and ankle weights or strength training machines can be added to address the muscle fatigue that often limits activity in CHF.
Using low weight and high repetitions prevents straining and breath holding, which place greater demands on the heart.
The focus should be on the major muscles of the upper and lower body and torso.
One to two sets with 12 to 15 repetitions per set provides an adequate training stimulus.
Part 11 –
This section gives some important tips on how to exercise safely when you have CHF or other debilitating illnesses.
Important Tips
- Be alert for symptoms like
- chest pain,
- increasing shortness of breath,
- weight gain,
- ankle swelling,
- abdominal bloating, or
- rapid pulse at rest.
Call your doctor, and stop exercising until the symptoms are controlled.
- Exercise and medication usually work well together. However, if you work out shortly after taking your medication, you may become dizzy or faint. A change in timing of exercise will often relieve the problem. Also, avoid exercise right after meals.
- Warm up. Before exerting yourself, spend 10 minutes in slow, easy activity--walking slowly and stretching--to increase blood flow to your muscles.
Conclusion
The lack of exercise can cause congestive heart failure but the participation in exercise once you have CHF can improve your heart’s performance, your sense of well being and your longevity.
|