|
Routine medication reconciliation is critical to the maintenance of accurate and complete medication records. Medication reconciliation requires the matching of the medication:
- The patient is actually taking,
- With the medications the provider thinks the patient is taking,
- With the medications which have been prescribed by all physicians
- With medications which have been changed at critical points of transitions of care such as between the discharge from the hospital to another facility or to the ambulatory setting
- With the medications which the patient has actually had filled
- With the medications the patient has had refilled
This is a complex and time consuming task but with opioids and other potentially habit forming medications it is critical. The assumption that the patient is only taking the medications, the provider thinks they are taking is a dangerous assumption without a rigorous medication reconciliation process.
There was a time when medication reconciliation was done by comparing the medications brought to the doctor’s office in a brown paper by a patient which was compared to a hand-written list of medications the provider thinks the patient is taking.
This did not allow for:
- Did the patient fill the prescriptions given by the provider?
- Did the patient refill the prescription which he/she was taking?
- Is the patient getting medications from multiple providers?
- In the case of controlled substances is the patient seeing multiple providers and receiving pain medications for each of them?
Physician's Role in Medication Reconciliation
In 2007, the American Medical Association published its 37-page monograph entitled, The Physician's Role in Medication Reconciliation: Issues, Strategies and Safety Principles. The preface gives this warning to physicians: "Medication Reconciliation is essential to optimize the safe and effective use of medications. It is one element in the process of therapeutic use of medications and medication management for which physicians are ultimately held legally accountable...".
Medication Reconciliation is hard and it is critical. The dynamic nature of medications being taken creates the complexity of maintaining and accurate lists as does the fact that most patients on multiple medications are being seen by two to seven providers annually. The probability for medication reconciliation to result in accuracy in medication administration is increased by the frequency of reconciliation being completed, particularly when each reconciliation is thorough. If a patient has ten to fifteen medication reconciliations or more per year, adverse medication events will decline and hopefully disappear. Such reconciliations are time consuming and require perseverance, but the result will be increased safety and improved care with decreased cost.
In the context of the Special Forces principles defined by Admiral McRaven and discussed previously discussed in this series, the “surprise” is that now healthcare provider have access to at least two data bases for determining the medications patients are taking.
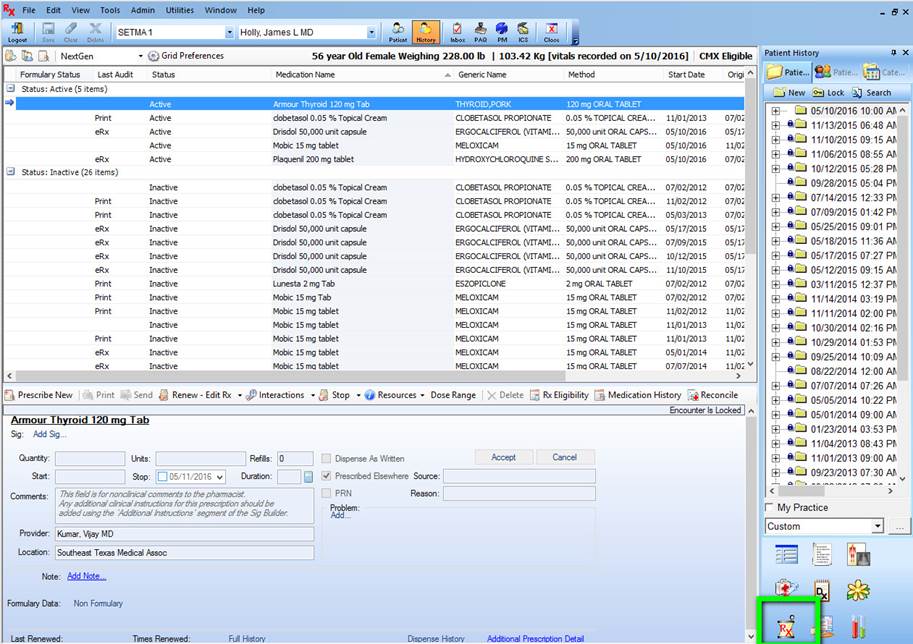
The first one is built into the EMR. The most important aspect of medication reconciliation is data collection. With the use of an EMR, such as used by SETMA, this process can be systematized. When A SETMA provider goes to the medication module, he/she will find a “medication module” icon (see below outlined in green).
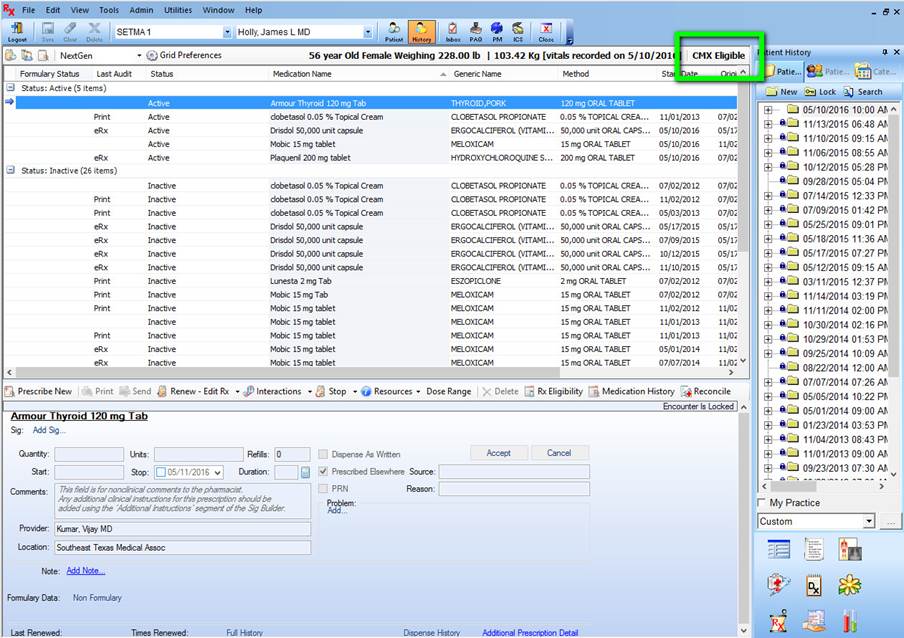
Once on the medication module, you can see if this patient is eligible for use of the automated medication reconciliation by looking at the designation in green. As long as this does not read “Not Eligible” then you may use the reconciliation function for that patient.
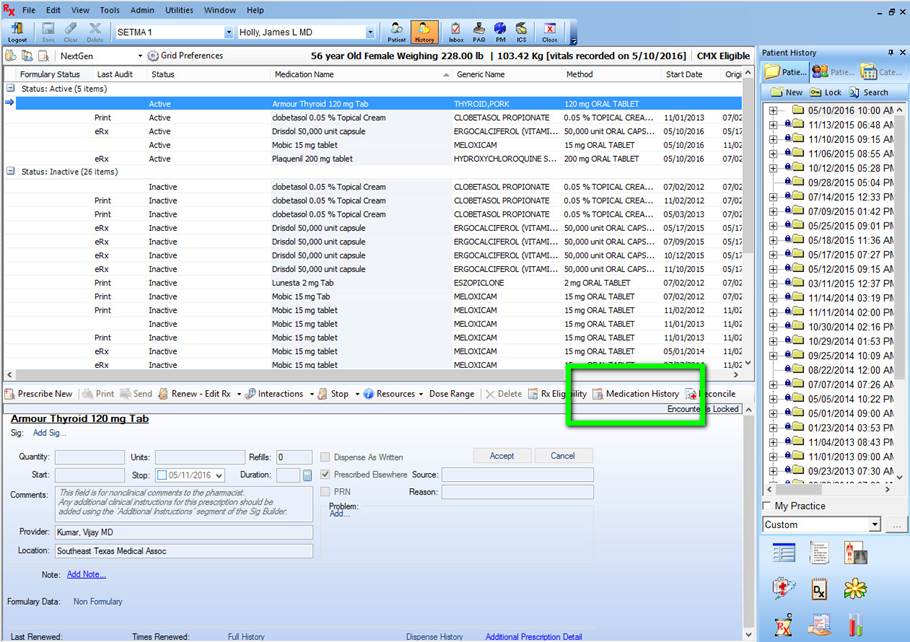
If the record shows that the patient is eligible for medication reconciliation, you will click on the button entitled “Medication History,” seen below outlined in green.
When this function is launched, you will see a screen which states “Queued for processing, please wait.” The first time you do the Medication Reconciliation, this will take a little longer but is very fast once you have used the function.
When the process is complete, you will see the following screen which gives you all the medications which this patient has received. Typically, this is up-to-date. I have had a patient who filled his medication at 4 PM the day before being seen at 8 AM the next day and the medication was in the queue.
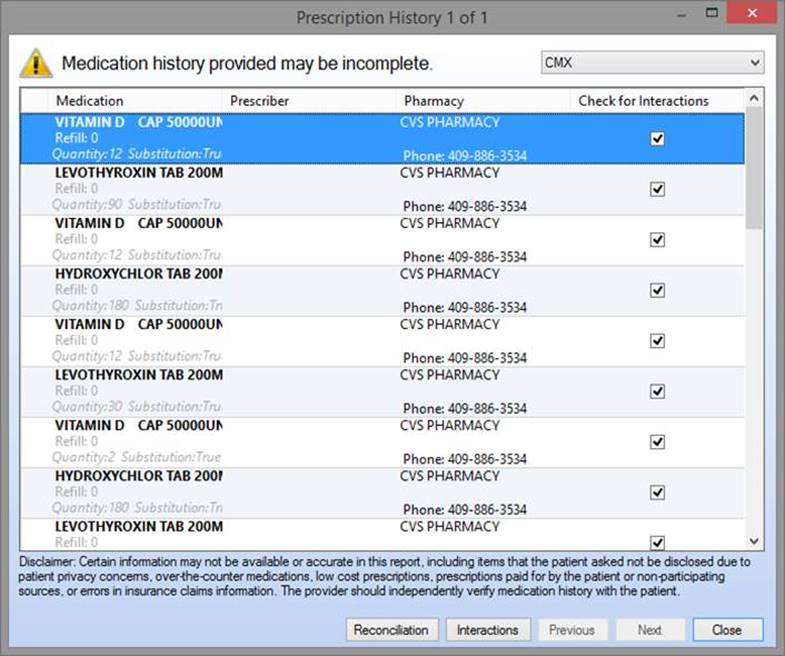
The medication reconciliation function will then display the medications filled with the medications in the EMR. If there are discrepancies, these can be resolved so that the medication list is accurate and complete.
Next week, we will discuss medication reconciliation for controlled substances.
|