|
Diabetes Disease Management Tool
The complexity of Diabetes Management is changing rapidly. The integration of diabetes care with hypertension, Cardiometabolic Risk Syndrome, weight management, lipids, renal disease, nephrology, neurology, ophthalmology, podiatry and many other disciplines makes it the ideal treatment focus for electronic patient management.
Also, the care of diabetes has moved through the three stages of health care decision making: intuitive - which requires great skill, knowledge and experience; evidenced-based - which requires knowledge of current standards of care; precise medicine - where the goals and treatments are standardize such that except in unusual cases it is possible to care for patients based on algorithms, treatment protocols and guidelines.
SETMA’s disease management tool standardizes care and brings to bear on each patient’s care, what is known in the medical literature about optimal, excellent care of patients with diabetes.
Following SETMA’s Model of Care, our care of diabetes includes:
- Tracking quality metrics one patient at a time
- Auditing metrics over panels and populations of patients
- Analyzing the audited data to find leverage points for improvement
- Public Reporting provider performance and transparently sharing with our patients that performance.
- Designing quality improvement initiatives based on these four steps.
A complete description and explanation of this Model of Care can be found at: Primary Care: The Future - Primary Care Progress (PCP)
As SETMA grew, we came to believe that the future of healthcare will be founded on four domains:
- Method -- The methodology of healthcare must be electronic patient management.
- Content -- The content and standards of healthcare delivery must be evidenced-based medicine.
- Structure -- The structure and organization of healthcare delivery must be patient-centered medical home.
- Compensation - The payment must be capitation with rewards for quality in both process and outcomes.
In this time, SETMA has become an NCQA Tier-Three Patient Centered Medical Home and a AACH accredited ambulatory care clinic, an AAACH Medical Home and the first multispecialty group to become an affiliate of Joslin Diabetes Center. We document all patient care in the same database whether the patient is in the hospital, home heath, physical therapy, hospice, nursing home, clinic or emergency department and are supporting the development of a regional health information exchange.
Quality Metrics Philosophy
SETMA’s approach to quality metrics and public reporting is driven by these assumptions:
- Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care. Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare “Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there.
- The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and patient-population data.
- There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- The collection of quality metrics should be incidental to the care patients are receiving and should not be the object of care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
SETMA currently tracks the following:
- 34 NCQA HEDIS measures;
- 14 NCQA Diabetes Recognition Metrics;
- 35 NQF-endorsed measures;
- 27 PQRS measures;
- 9 PCPI measures related to the physician role in hypertension management;
- 43 measures of the Bridges to Excellence program for Asthma, Chronic Stable Angina, Congestive Heart Failure, COPD, Diabetes and Hypertension;
- 10 PCPI related to Diabetes;
- 6 PCPI for Stages 4 and 5 of Chronic Kidney Disease;
- 5 PCPI for Chronic Stable Angina;
- 7 PCPI for Congestive Heart Failure;
- 20 PCPI Transition of Care measures.
We are also participating in the Guidelines Advantage Program which is a collaborative between the American Heart Association, the American Diabetes Association and the American Cancer Society. And we are tracking the metrics associated with the MA STARS, the ACO quality metrics and the Meaning Use metrics.
In addition to endorsed-measurement sets, SETMA tracks these self-designed quality measures: 10 measures related to hyperlipidemia; 12 measures related to Chronic Kidney Disease Stages 1-III. Also, in the hospital setting, SETMA has designed an internal study to identify patterns in hospital readmissions, such as lengths of stay, morbidities and co-morbidities, socio-economic status, ethnicity, gender, age, follow-up calls, follow-up visits in clinic, etc.. The purpose is to control cost and increase safety by reducing preventable readmissions to the hospital.
Population Management and Quality Improvement Metrics
SETMA tracks a number of key data points for diabetes, hypertension and hyperlipidemia for its entire patient population. These measures are compared between patients who are controlled against patients who are not controlled. Secondly, the results for the controlled and uncontrolled populations are further analyzed by gender, age, ethnicity, numbers of medications, frequency of visits, frequency of test, income and other measures in an effort of to reduce disparities in patient care across all demographics.
To ensure timely adherence by providers, SETMA has designed functions within its EHR to alert providers to patient conditions which must be reported to local or state agencies for infectious disease control. SETMA reports the results of all of measures publicly, by provider name, at www.jameslhollymd.com.
The Limitations of Quality Metrics
The New York Times Magazine of May 2, 2010, published an article entitled, "The Data-Driven Life," which asked the question, "Technology has made it feasible not only to measure our most basic habits but also to evaluate them. Does measuring what we eat or how much we sleep or how often we do the dishes change how we think about ourselves?" Further, the article asked, "What happens when technology can calculate and analyze every quotidian thing that happened to you today?" Does this remind you of Einstein's admonition, "Not everything that can be counted counts, and not everything that counts can be counted?"
Technology must never blind us to the human. Bioethicist, Onora O'Neill, commented about our technological obsession with measuring things. In doing so, she echoes the Einstein dictum that not everything that is counted counts. She said, "In theory again the new culture of accountability and audit makes professionals and institutions more accountable for good performance. This is manifest in the rhetoric of improvement and rising standards, of efficiency gains and best practices, of respect for patients and pupils and employees. But beneath this admirable rhetoric the real focus is on performance indicators chosen for ease of measurement and control rather than because they measure accurately what the quality of performance is."
Technology Can Deal with Disease but Cannot Produce Health
In our quest for excellence, we must not be seduced by technology with its numbers and tables. This is particularly the case in healthcare. In the future of medicine, the tension - not a conflict but a dynamic balance - must be properly maintained between humanity and technology. Technology can contribute to the solving of many of our disease problems but ultimately cannot solve the "health problems" we face. The entire focus and energy of "health home" is to rediscover the trusting bond between patient and provider. In the "health home," technology becomes a tool to be used and not an end to be pursued. The outcomes of technology alone are not as satisfying as those where trust and technology are properly balanced in healthcare delivery.
Our grandchildren's generation will experience healthcare methods and possibilities which seem like science fiction to us today. Yet, that technology risks decreasing the value of our lives, if we do not in the midst of technology retain our humanity. As we celebrate science, we must not fail to embrace the minister, the ethicist, the humanist, the theologian, indeed the ones who remind us that being the bionic man or women will not make us more human, but it seriously risks causing us to being dehumanized. And in doing so, we may just find the right balance between technology and trust and thereby find the solution to the cost of healthcare.
It is in this context that SETMA whole-heartedly embraces technology and science, while retaining the sense of person in our daily responsibilities of caring for persons. Quality metrics have made us better healthcare providers. The public reporting of our performance of those metrics has made us better clinician/scientist. But what makes us better healthcare providers is our caring for people.
Team Approach to Healthcare Delivery
The ideal setting in which to deliver and to receive healthcare is one in which all healthcare providers value the participation by all other members of the healthcare-delivery team. In fact, that is the imperative of Medical Home. Without an active team with team-consciousness and team-collegiality, Medical Home is just a name which is imposed upon the current means of caring for the needs of others. And, as we have seen in the past, the lack of a team approach at every level and in every department of medicine creates inefficiency, increased cost, potential for errors and it actually eviscerates the potential strength of the healthcare system.
Why is this? Typically, it is because healthcare providers in one discipline are trained in isolation from healthcare providers of a different discipline. Or, they are in the same buildings and often are seeing the same patients but they rarely interact. Even their medical record documentation is often done in compartmentalized paper records, which are rarely reviewed by anyone but members of their own discipline. This is where the first benefit of technology can help resolve some of this dysfunction. Electronic health records (EHR), or electronic medical records (EMR) help because everyone uses a common data base which is being built by every other member of the team regardless of discipline.
While the use of EMR is not universal in academic medical centers, the growth of its use will enable the design and function of records to be more interactive between the various schools of the academic center.
And, why is that important? Principally, because more and more healthcare professionals are discovering that while their training often isolates them from other healthcare professionals, the science of their disciplines is crying for integration and communication. For instance, there was a time when physicians rarely gave much attention to the dental care of their patients, unless they had the most egregious deterioration of teeth. Today, however, in a growing number of clinical situations, such as the care of diabetes, physicians are inquiring as to whether the patient is receiving routine dental care as evidence-based medicine is indicating that the control of disease and the well-being of patients with diabetes is improved by routine dental care. Also, as the science of medicine is proving that more and more heart disease may have an infectious component, or even causation, the avoidance of gingivitis and periodontal disease have become of concern to physicians as well as dentist.
Disruptive Innovation
In addition, Medical Home places major emphasis upon issues which historically have been the concern of nurses. Physicians who use EMRs are discovering that the contribution of nursing staff can make the difference in the excellent and efficient use of this documentation and healthcare-delivery method. No longer is the nurse a “medical-office assistant” ancillary to the care of patients, but the nurse is a healthcare colleague central and essential to the patient’s healthcare experience. As evidence-based medicine expands the scope of what The Innovator’s Prescription: A Disruptive Solution for Health Care By Clayton M. Christensen labels as “empirical medicine” which ultimately leads to “precise medicine,” it is possible for physicians and nurses to be a true-healthcare delivery team, as opposed to the nurses only being an aide to the physician.
It is as a result of the need for the integration of healthcare disciplines at the delivery level, that the imperative becomes obvious for the restructuring of the training of the members of this healthcare team. And, the first change must come in the relationships between the leaders of the training programs who educate and mentor future healthcare scientist, teachers, caregivers and researchers. The educational leaders must model this integration for their disparate student bodies and that modeling will require the investment of the most precious and rare resource: time.
The Diabetes Suite of Templates can be accessed from:
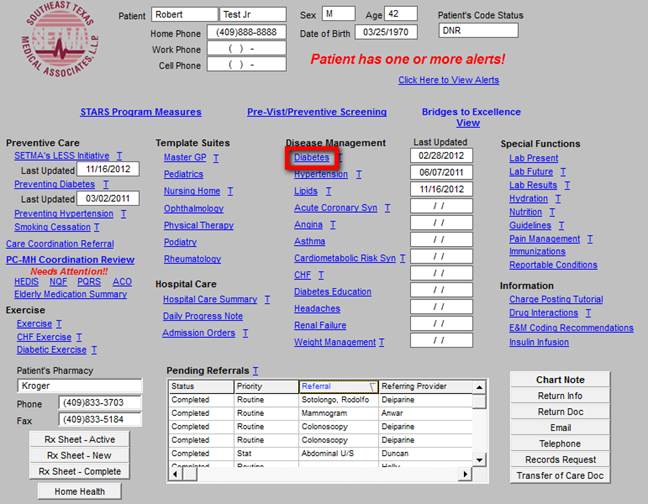
- NextGen’s Main Tool Bar’s Template Icon
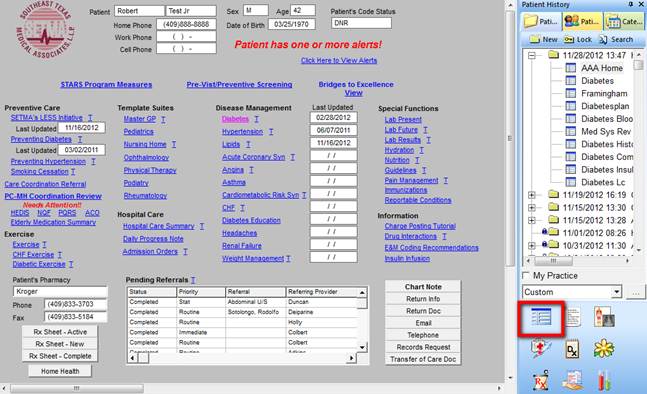
- When the Template button is clicked you will be presented with the preference list.
- If the Diabetes master template is listed as one of your preferences, select it.
- If it is not one of your preferences, select the All radio button and then scroll down until you find it in the list.
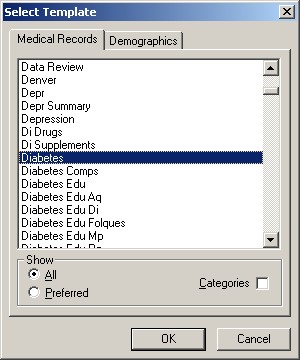
NOTE: For more on how to set up your preferences, Click Here
Before detailing the Diabetes Master Template (the first template in the diabetes suite), we need to look at the standard of excellence for Diabetes Care which is tracked and documented by SETMA’s Diabetes Suite of Templates.
- To do this, go to SETMA’s Navigation Buttons on the right hand side of the Diabetes Master Template.
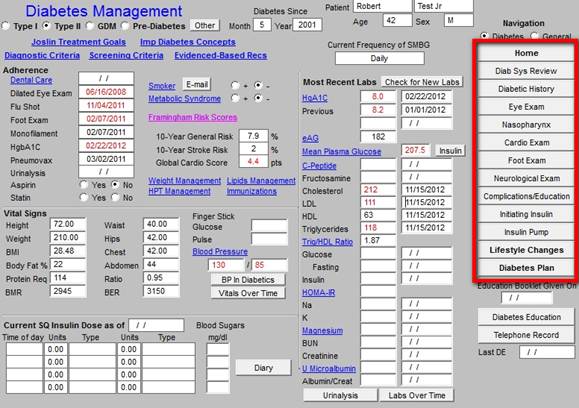
- At the top of the Navigation Buttons, there is the title Navigation.
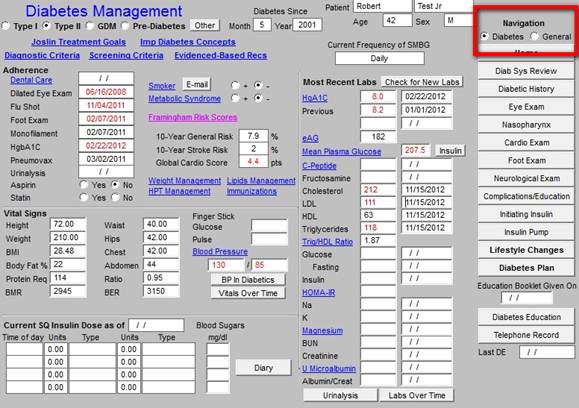
- The next function is two buttons which are entitled:
- Make sure the box beside the word “Diabetes” is checked.
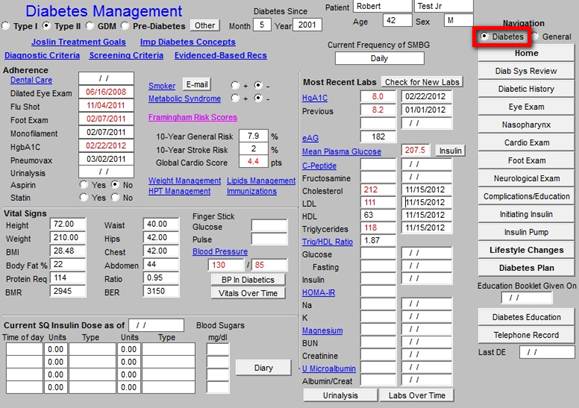
- This will display twelve Navigation Buttons.
- The Navigation button at the bottom of this list of twelve is “Diabetes Plan”
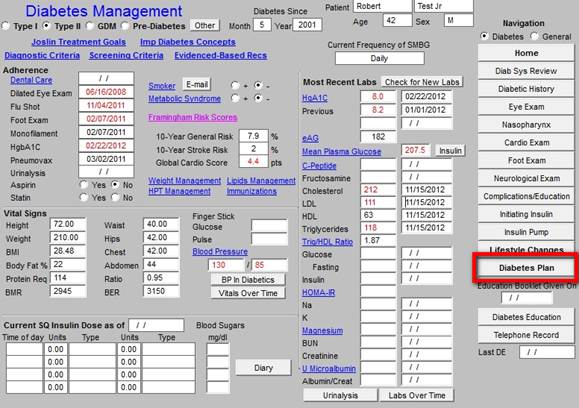
- Click on the Diabetes Plan Button, this launches the Diabetes Plan template (We will discuss the content of this template later).

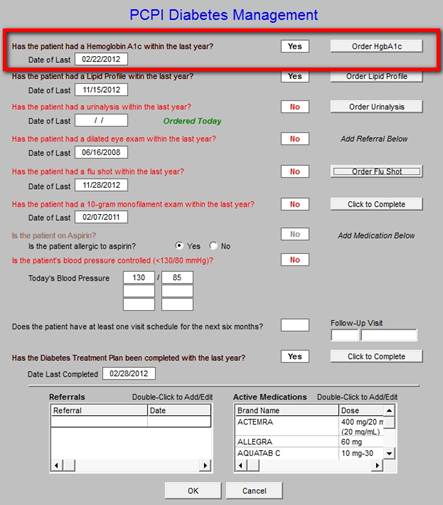
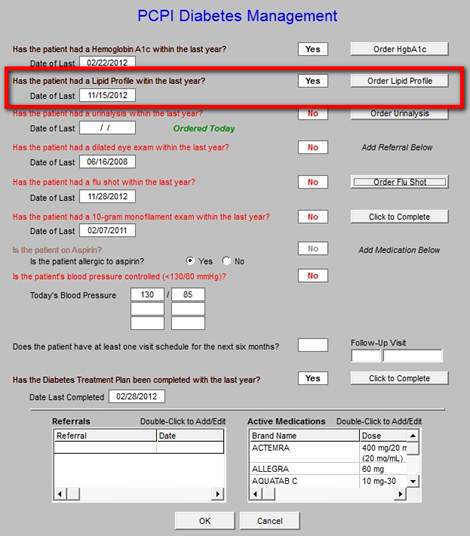
- In the list of Navigation Buttons at the right hand side of the Plan Template, the second button is entitled Consortium Data Set, click on that button. This will launch a pop up window titled "PCPI Diabetes Management". The Diabetes Management is a means of measuring diabetes care given by a provider. The data points are taken from the Physician Consortium for Performance Improvement (PCPI). Additional functionality has been added to make it easier to provide diabetes care right rather than not at all.
Upon completing the evaluation and treatment of a patient with diabetes, the provider can launch the PCPI measure set function. The measures which are done appear in black; those which are not done appear in red. For any metrics which are not completed, the button to the right can be clicked. Depending upon the metric, the provider will be taken to the point in the EMR where that element is documented such as in the Foot examination or in the case of a lab test, the clicking of the button will order the test, send it to the lab, send it to charge posting and place the order on the chart.
In addition to the PCPI diabetes data set, SETMA also tracks:
- The HEDIS Diabetes set
- The PQRS Comprehensive Diabetes Data set
- The Joslin Diabetes Data set
- The NCQA Diabetes Data Set - this differs from the HEDIS measurement set although it is also produced by NCQA.
- The Bridges to Excellence Diabetes Measurement set.
- National Quality Forum Comprehensive Diabetes Measurement Set
- AQA Diabetes Measurement Set
Those will be learned elsewhere.
The Physician Consortium for Performance Improvement
The Physician Consortium for Performance Improvement (PCPI) is a group of clinical and methodological experts convened by the AMA. The Consortium includes representatives from more than 60 national medical specialty and state medical societies, the Agency for Healthcare Research and Quality, and the Centers for Medicare and Medicaid Services.
The Consortium's vision is to fulfill the responsibility of physicians to patient care, public health, and safety by:
- becoming the leading source organization for evidence-based clinical performance measures and outcomes reporting tools for physicians; and
- ensuring that all components of the medical profession have a leadership role in all nationalforums seeking to evaluate the quality of patient care.
The Consortium's mission is to improve patient health and safety by:
- identifying and developing evidence-based clinical performance measures that enhance quality of patient care and that foster accountability;
- promoting the implementation of effective and relevant clinical performance improvement activities; and
- advancing the science of clinical performance measurement and improvement.
The Consortium works to develop evidence-based clinical performance measures and clinical outcomes reporting tools to support physicians in quality improvement efforts.
The Consortium has published a number of disease management data sets which established quality of care measures with which physicians and other healthcare providers can measure their own performance.
The 9 data points which are automatically captured and documented by SETMA’s Diabetes Suite of Templates, and, which are collected and displayed on the Consortium Data Set pop-up on the Diabetes Plan, are the quality measures for diabetes developed by the Consortium.
These 9 data points are the basis along with several other data points of SETMA’s Daily Diabetes
Care Audit. These data points are:
- Collected automatically
- Provide a quick and easy review for the SETMA healthcare provider to evaluate his/her own Diabetes care.
- Provide a quick and easy way of completing the Diabetes measures required if they were not completed.
- Attention to these data points places in you line for additional reimbursement when CMS begins paying providers for performance in the coming years.
- The Consortium material should be completed by the nursing staff and reviewed by the provider.
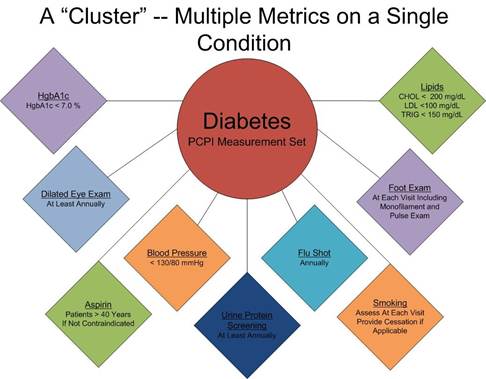
SETMA employs two definitions in quality metrics analysis:
- A “cluster” is seven or more quality metrics for a single condition, i.e., diabetes, hypertension, etc.
- A “galaxy” is multiple clusters for the same patient, i.e., diabetes, hypertension, lipids, CHF, etc.
SETMA believes that fulfilling a single or a few quality metrics does not change outcomes, but fulfilling “clusters” and “galaxies” of metrics which are measurable at the point-of-care can and will change outcomes. The following illustrates the principle of a “cluster” of quality metrics. A single patient, at a single visit, for a single condition, will have eight or more quality metrics fulfilled for a condition, which WILL change the outcome of that patient’s treatment.
The following illustrates a “galaxy” of quality metrics. A single patient, at a single visit, may have as many as 60 or more quality metrics fulfilled in his/her care which WILL change the quality of outcomes and will result in the improvement of the patient’s health. And because of the improvement in care and health, the cost of that patient’s care will be decreased as well.
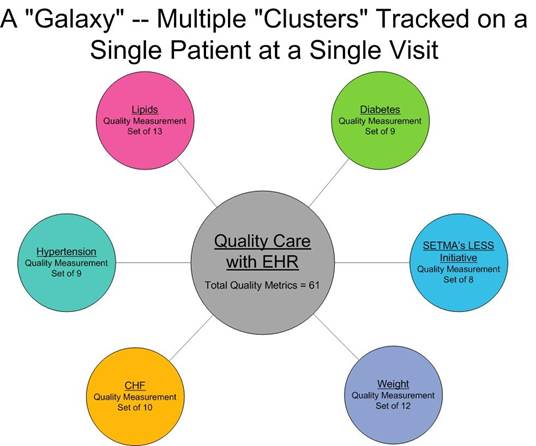
SETMA’s model of care is based on the concepts of “clusters” and “galaxies” of quality metrics. Foundational to this concept is that the fulfillment of quality metrics is incidental to excellent care rather than being the intent of that care.
The Elements of the Consortium Data Set for Diabetes
Hemoglobin A1C -
- The standard is that the patient has had a Hemoglobin A1C in the last year or has one at this visit.
- The date of the last Hgb A1C is displayed on this template.
- If this data point is out of date, a button will appear to the right of the date box.
- When you depress this button you will automatically order and charge post a Hgb A1C, making it easier to do it right than not to do it at all.
Fasting Lipid Profile Current -
- The standard is that there has been a Lipid Profile in the last year or one has been done today.
- If the Lipid Profile is out of date, the order button will appear to the right of the date box which when depressed will order and charge post a Lipid Profile.
- If the patient has not fasted for twelve hours, a Lipid panel should be ordered by the Future Labs Template.
Diabetes is an independent risk factor for cardiovascular disease, as is LDL. In addition to limb, renal function and vision preservation, the careful treatment of diabetes is necessary to mitigate the cardiovascular risk burden placed on a patient’s life by their having diabetes. Part of the optimal care of patients with diabetes is the calculation of their Framingham Risk Scores and the discussion with them of their “What IF” scenarios. They can be found at
Framingham Cardiovascular Risk Assessment
Several of the scores include the presence or absence of diabetes and one score which is derived from the Framingham data entitled Global Cardiovascular Risk Score includes the Hemoglobin A1c value as an element of the score’s calculation.
In addition, the calculation of the Cardiometabolic Risk Syndrome assessment for each patient with diabetes is important. The tutorial for that calculation is found at:
Metabolic Syndrome Tutorial
The Cardiometabolic Risk Syndrome has been known at one time or another by the following names:
- Syndrome X
- Metabolic Syndrome
- Insulin Resistance Syndrome
In SETMA’s tutorial for the Cardiometabolic Risk Syndrome, the following chart appears which shows the progression from pre-diabetes to diabetes. It shows the elements of that progression.
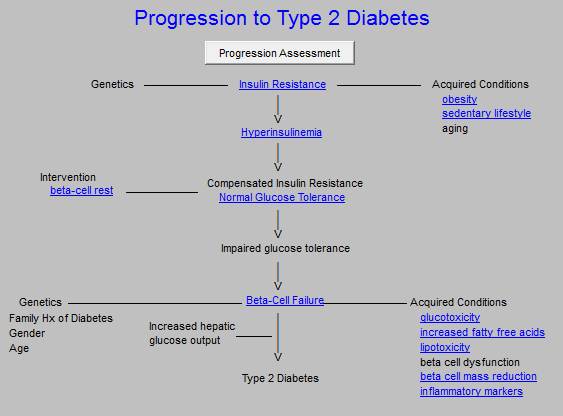
In the EMR, each of the underscored elements in blue are hyperlinks and can be accessed for information on the contribution of each of the elements to the progression to diabetes. The following are the documents which are deployed when each of these buttons are clicked:
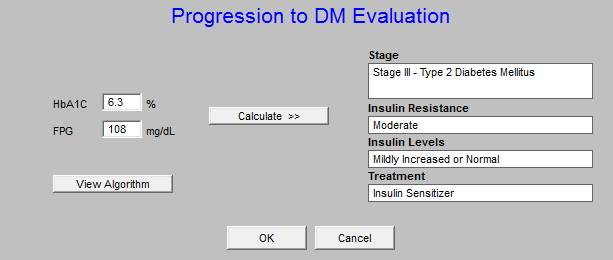
The button entitled Progression Evaluation when accessed deploys the following. When used in the EMR, the template is automatically populated with the HbA1c and the Fasting Blood Glucose to calculate the stage toward the development of diabetes.
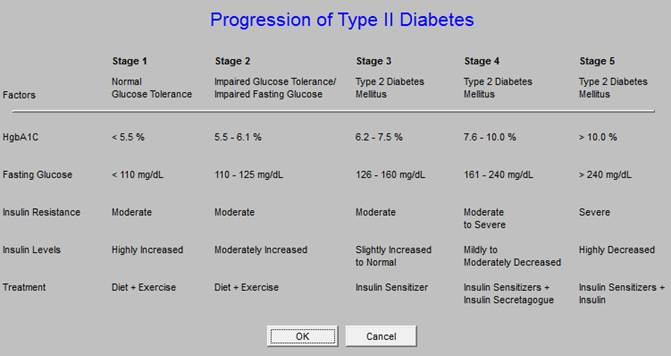
The following is deployed with you click on the button entitled View Algorithm and it defines the stages of progression to diabetes.
The next PCIP measure is for urinalysis.
Urinalysis Current -
- The standard is that a urinalysis with microscopic examination and protein analysis is done at least once a year.
- If the date box indicates that the urinalysis is “out of date,” a button will appear.
- When depressed a urinalysis will be ordered and charged posted and sent to the lab.
Preservation of renal function is so important in patients with diabetes, SETMA has created a disease management tool for renal disease from the National Kidney Foundation’s published standards of kidney care. The following link will take you to the tutorial for that tool.
Renal Tutorial
The following is the Evaluation of Chronic Renal Failure from that management tool. When completed, this will give the provider the stage of renal disease.
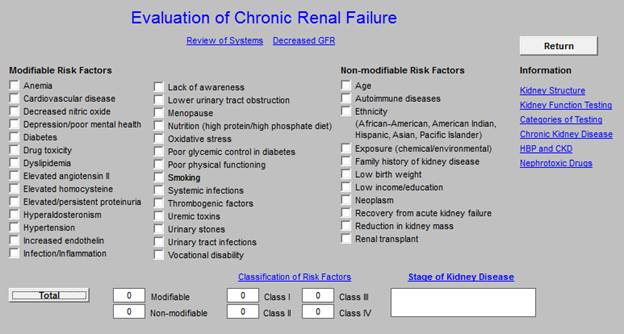
Uncontrolled diabetes is the most common cause of renal failure in the United States. Routine urinalysis is the first step in anticipating renal impairment.
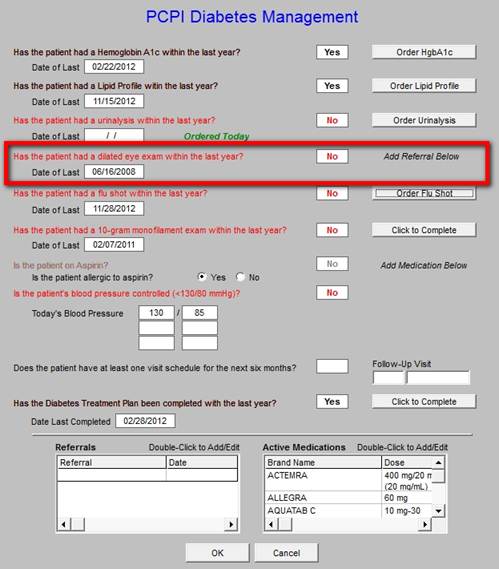
Eye Exam Current -
- The standard is that a dilated eye examination by an ophthalmologist is done annually on all patients with diabetes.
- If the date box indicates that there has not been a dilated eye examination in the past year, the referral template can be access at the bottom of the screen to complete a referral to an ophthalmologist.
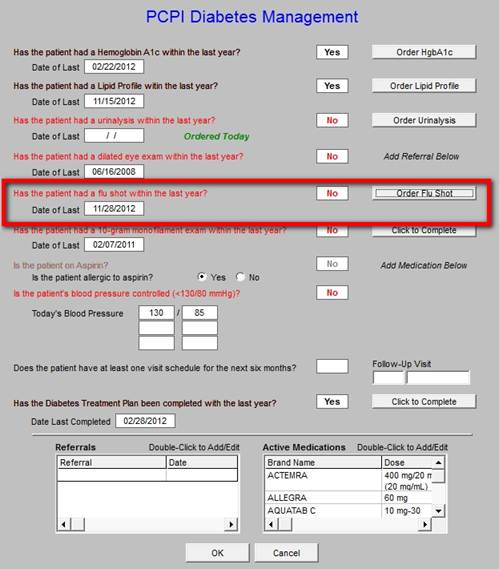
Flu Shot Current -
- The standard is that a flu shot has been given each year to patients with diabetes.
- If the flu shot has not been given in the past year, there will be a button which allows you to indicate that a flu shot is being ordered for today.
- If you depress this button, it is necessary also to complete the Immunization Template for a flu shot and to tell your nurse to give the flu shot.
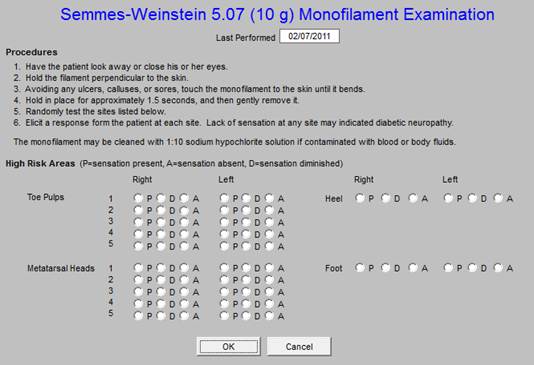
Foot Exam Current -
- The standard of care is that a thorough foot examination be completed at least once a year and at every visit for patients with diabetes.
- This foot examination must include:
- A visual inspection of the foot and especially the skin between the toes.
- An examination of the pulses in the foot.
- A 10-gram monofilament examination of the sensory capacity of the foot.
- An examination of the nails.
- If a foot examination has not been done, a button will appear which when depressed will take you right back to the Foot Exam on the Diabetes Suite of Templates allowing you to quickly and easily complete that required examination.
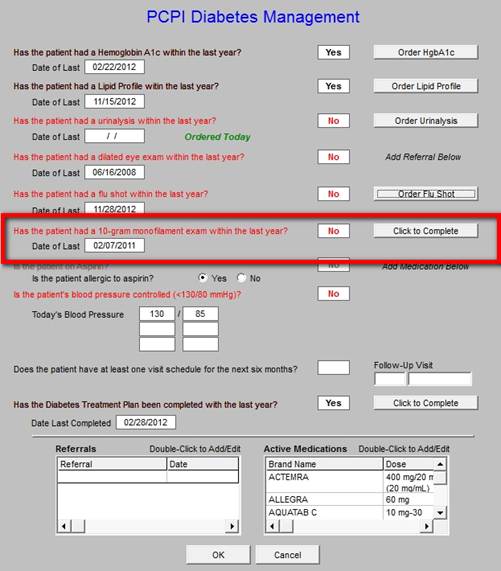
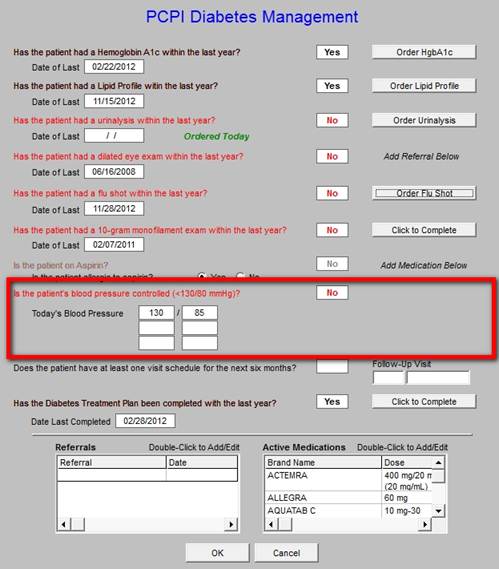
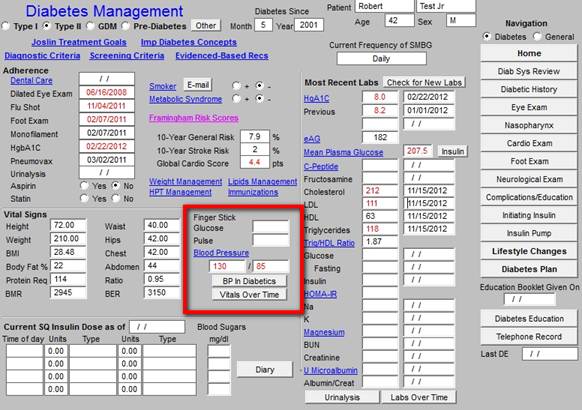
Monitor Blood Pressure -
- The standard is that the patient’s blood pressures should be measured at every visit.
- The box beside the name “blood pressure,” does not contain the date as the standard is “every visit,” but it documents today’s blood pressure.
- If the blood pressure is higher than the standard for blood pressure care for a patient with diabetes, the blood pressure value will be in red.
- The blood pressure standard for patients with diabetes less than 130/80 mmHg.
- Many diabetologists argue that blood pressure control is more important than blood sugar control for avoiding the complications of diabetes.
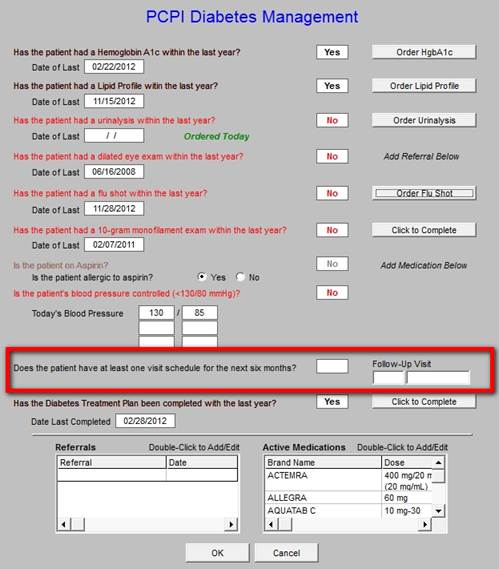
Ensure the patient has at least two office visits per year -
- The standard of this measure is indicated in its name.
- Enter the timeframe for a follow-up within the next six months to fulfill this measure.
- The patient’s follow-up instructions are documented here.
Is the patient on Aspirin? -
- The standard is that every patient who has diabetes should be on aspirin, unless there is a contraindication.
- Aspirin is so important because of the increased inflammatory and prothrombotic state of all patients with diabetes that it is asked about on:
- The Diabetes Master Template (see below),
- The Diabetes Plan Template
- The Diabetes Management template as an element of the Consortium data set.
- There are check boxes for saying that the patient is or is not on Aspirin.
- These check boxes are interactive with the check boxes on the Master template and the Plan template.
- If the patient has a contraindication for aspirin, it should be documented on this template.
- The acceptable contraindications are concurrent treatment with the following medications or one of the listed complications:
- Aggrenox
- Allergic
- Bleeding
- Coumadin
- Patient Refuses
- Plavix
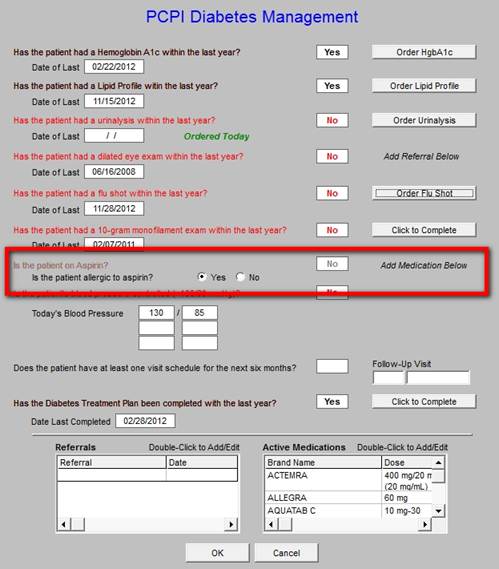
Once these elements have been checked and it only takes a few seconds, the documentation of excellence in diabetic care based on the consortium data set has been completed. In two years, when Medicare starts paying providers for performance, the completion of the Consortium Data Set will qualify you for increased reimbursement from Medicare.
Diabetes Patient Adherence
SETMA also tracks the adherence of patients with Diabetes. There are 7 data points which are tracked. These data points are displayed on a pop-up which is launched by a button entitled Patient Adherence which is found on the Diabetes Plan beneath the Consortium Data Set button.
These compliance data points must be manually documented on each visit. The compliance materials should be completed by the nursing staff. This is also part of SETMA’s diabetes care audit. The data points are:
- Adherent with medication?
- Adherent with Follow-up?
- Adherent with Diet?
- Adherent with Education?
- Adherent with Exercise?
- Patient sees an endocrinologist? Outside physician?
- Yes/No
- If yes, list the physician below (a pop-up gives the names of endocrinologists)
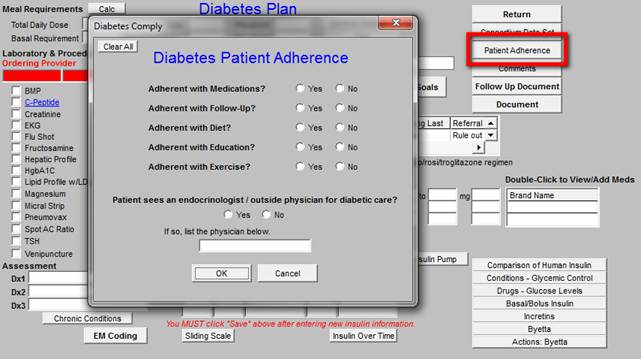
Now click Ok, and it takes you back to the Diabetes Plan template.
Back to the Diabetes Master Template
On the Diabetes Master Template It will be noted that like all SETMA templates, which are built on NextGen’s platform, they appear with the following at the top of each template:
- Title Bar
- Menu Tool Bar
- Top Tool Bar
NOTE: For more information on NextGen Toolbars, Click Here.
Beneath the Top Tool Bar there are three lines of functions before getting to the main Diabetes management tool; they are:
- A line in which the patient’s type of diabetes is documented.
- On this line there are check boxes for Type 1, Type 2, GDM (Gestational Diabetes Mellitus), “pre-Diabetes and a button for “Other.”
- When depressed the “Other” launches a pop-up which 28 forms, types or presentations of diabetes.
- One of the first four, or one of the last 24 types of diabetes should be documented as the type of diabetes this patient has.
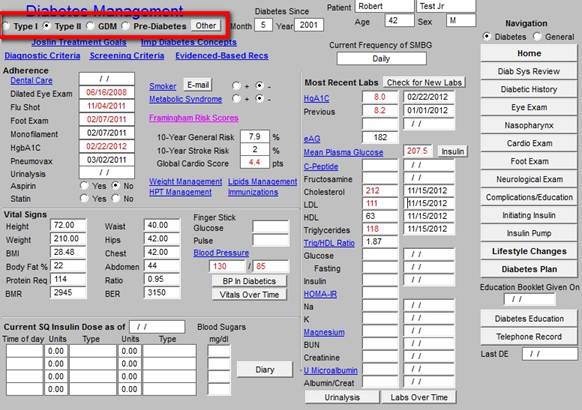
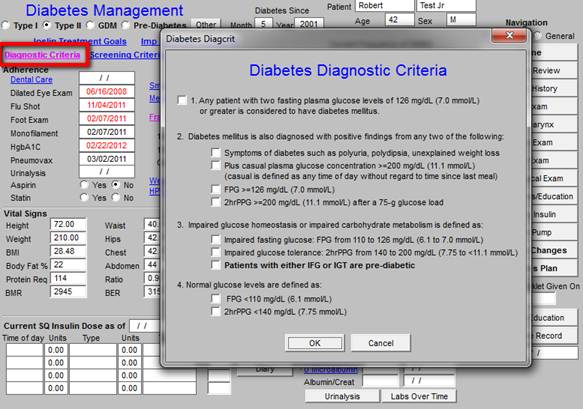
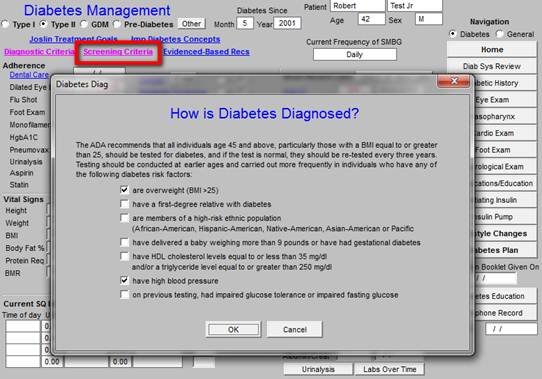
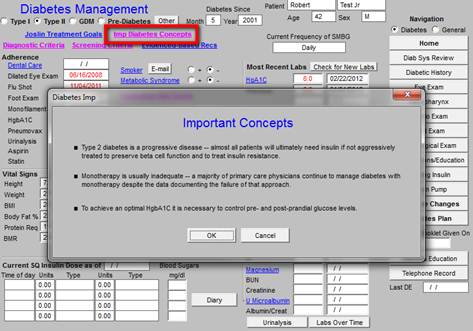
- A line with five hyperlinks for the following pop-ups:
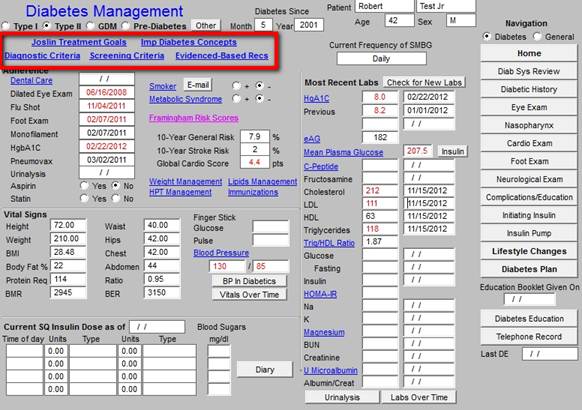
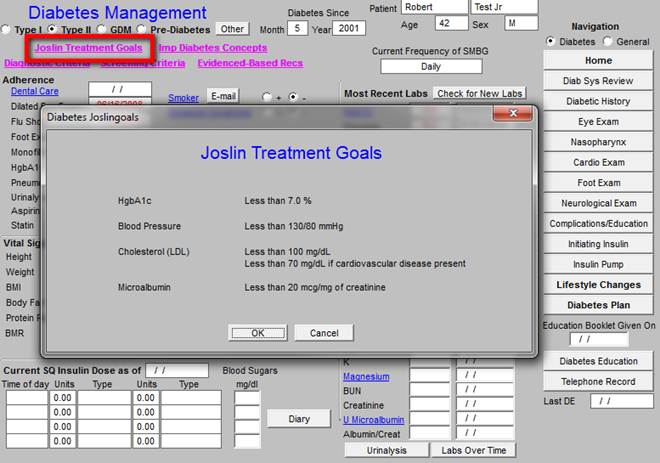
- Diagnostic Criteria - this launches a pop-up which is entitled Diabetes Diagnostic Criteria.
- Screening Criteria - this launches a pop-up entitled, How Is Diabetes Diagnosed?
- This data is also found in the Preventing Diabetes function on AAA Home.
- It is on the pop-up which is launched from Screening Recommendations.
- Expanded information on Impaired Fasting Glucose and Impaired Glucose Tolerance is found on the Preventing Diabetes template on the pop-up launched from IFG and IGT.
- Imp. Diabetes Concepts - this identifies three key principles (but not THE key principles) for the successful management of diabetes.
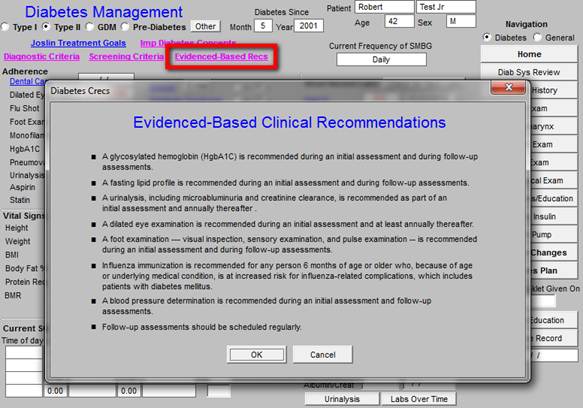
- Evidenced-Based Rec - this launches a pop-up on which 8 evidence-based recommendations are made for successful diabetes management. Those recommendations are:
- A glycosylated hemoglobin is recommended during an initial assessment and during follow-up assessments.
- A fasting lipid profile is recommended during an initial assessment and during follow-up assessments.
- A urinalysis, including microalbuminuria and creatinine clearance, is recommended as part of an initial assessment and annually thereafter.
- A dilated eye examination is recommended during an initial assessment and at least annually thereafter.
- A foot examination - visual inspection, sensory examination and pulse examination - is recommended during an initial assessment and during follow-up assessments.
- Influenza immunization is recommended for anyone 6 months of age and older, who because of age or underlying condition is at increased risk for influenza related complications, which includes patients with diabetes.
- A blood pressure determination is recommended during an initial assessment and during follow-up assessments.
- Follow-up assessments should be scheduled regularly.
Beneath these two lines, the Diabetes Master Template is organized into three columns; the first column has two columns within itself:
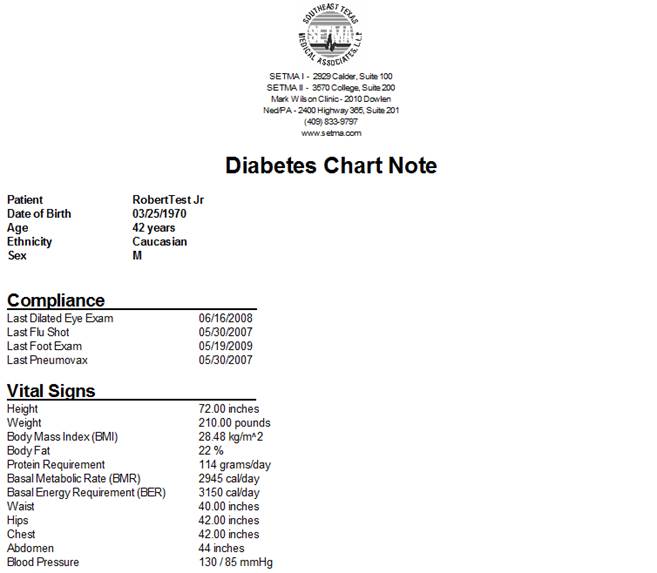
Column 1: Part A
Compliance - Ten elements are documented which are key to the proper treatment of diabetes. The date of last performance is listed at the side of each element. The nine elements are:
- Dental - It has been found that an annual dental examination promotes improved diabetes management.
- Dilated Eye Exam - An annual dilated eye examination is one of the standards of care for diabetes.
- Flu Shot - All patients with diabetes should receive a flu shot annually.
- Foot Examination Including Monofilament Exam - A foot exam including a 10 gram monofilament sensory examination should be part of EVERY visit.
- HgbA1C - Should be performed at each visit and at least three times a year.
- Urinalysis - Annual UA is the standard of care for diabetes.
- Aspirin - All patients with diabetes who are not allergic to aspirin, on coumadin or have had a bleeding episode should be on
- Statin - All patients with diabetes and the metabolic syndrome should be on a statin and all patients with diabetes probably should be on a statin.
A quick review of these 10 elements of compliance will indicate what care is deficient in this patient and will therefore guide the provider in instructing the patient.
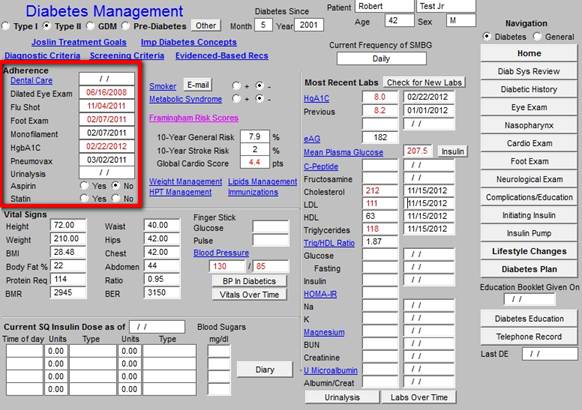
Vital Signs - In two columns 12 aspects of the patient’s vital signs, body habitus and metabolism are documented, including:
- Height
- Weight
- BMI
- Body Fat %
- Protein Requirement
- BMR
- Waist
- Hips
- Chest
- Abdomen
- Ratio
- BER

Finally, there is the information on the current SQ Insulin Dose:
- There is a box where the most recent update of the insulin dose is documented
- There are four boxes where the insulin type, units, and time of day are documented. Beside row of boxes is another box with the heading Blood Sugars mg/dl where the blood sugar trigger for any sliding scale dose can be documented.
- Insulin changes and updates are not made on this template but on the Plan Template. (see below)
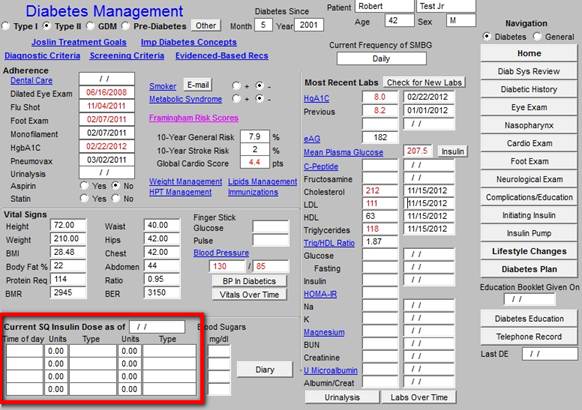
Blood Sugar Diary
Next to the Insulin Dose is a button entitled Diary
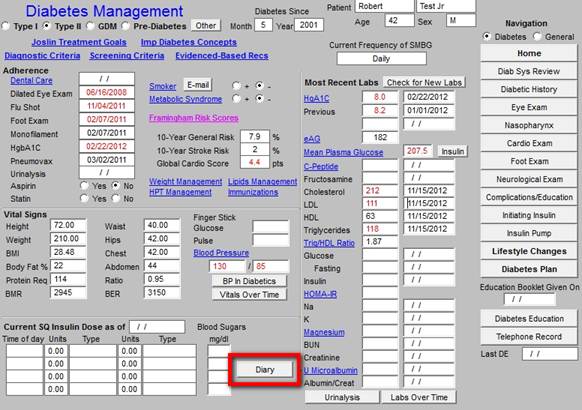
- This is a function where the patient’s home diary can be manually put into the computer.
- When the button entitled Diary is clicked, a new screen is displayed.
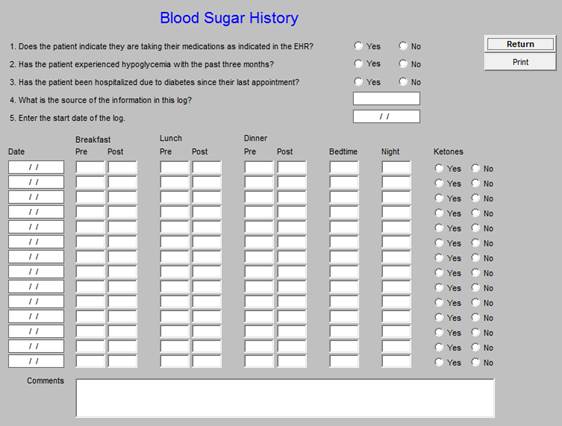
- At the top of the screen you should ask the patient to answer the questions about medications, hypoglycemia and hospitalization and document their response.
- At the bottom of the screen, you can enter up to 14 days of blood sugar history for the patient. All of the values are not required for each date you chose, but you should enter as much data as the patient has available.
- At the far right of each date, you can also indicate the presence or absence of ketones if the patient is monitoring them.
By clicking on “return,” you will be taken back to the Diabetes Master Template.
Column I Part B
At the beginning of Part B of the first column are 9 hyperlinks which take you to other tools needed for optimal diabetes care; they are:
- Smoker - There are check boxes for documenting whether the patient is a smoker or note. If the patient history has been filled out for “Current Habits,” this will automatically populate. By clicking on the word “Smoker,” you are taken to the Smoking Cessation template, which should have already been completed through the LESS Initiative. There is also a button entitled “E-mail.” This creates an electronic tickler file for reminding you to call the patient in one month about their success in stopping smoking.
- Metabolic Syndrome - There are check boxes for documenting whether the patient has the metabolic syndrome or not. By clicking on the words “Metabolic Syndrome,” you will be taken to the Metabolic Syndrome Suite of Templates’ Assessment Template. This will be automatically populated with the vital signs and laboratory work and an automatic conclusion will be drawn as to whether the patient has the Metabolic Syndrome. At that point, the “yes” or “no” boxes next to Metabolic Syndrome on the Diabetes Master Template will be updated appropriately.
- Framingham CVD 10-Year Risk - There is a box for the Framingham CVD Risk assessment to be documented. When you click on the hyperlink, you are taken to the Framingham function and given directions for its completion.
- Framingham Stroke 10-Yr Risk - same as for the CVD Risk.
- Global Cadio Risk - This is a recently developed risk assessment for stratification of cardiovascular risk. It is built on the Framingham data but with the non-modifiable risk factors eliminated.
NOTE: The Framingham CVD 10-Year Risk, Framingham Stroke 10-Yr Risk, and Global Cadio Risk draw their results from a SINGLE Framingham Assessment
- Weight Management - this takes you to the weight management suite of templates. Weight management is a key aspect of excellent diabetic care.
- Hypertension Management - this takes you to the hypertension management suite of templates. Blood pressure control is as important and maybe more important than glucose control in diabetes.
- Lipids Management - this takes you to Lipid suite of templates. Reduction of cardiovascular risk in diabetes is dependent upon rigorous cholesterol control.
- Immunizations - all patients with diabetes must have routine immunizations for flu and pneumonia.
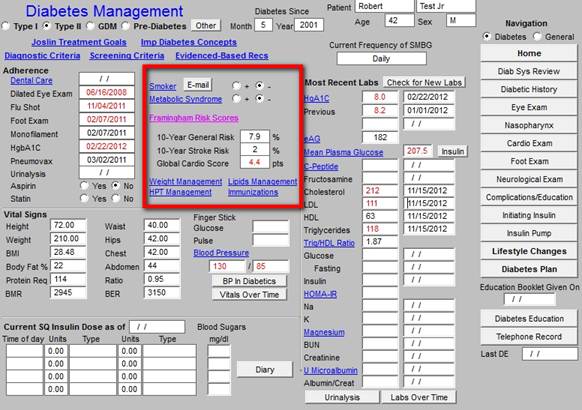
Beneath these hyperlinks are 5 additional functions related to Diabetes Care; they are:
- Finger Stick Blood Glucose - this is manually entered by the nurse.
- Pulse - this is auto filled from the nursing template.
- Blood Pressure - this is auto filled from the nursing template.
- BP in Diabetes - this is a treatment protocol for hypertension in the patient with diabetes.
- Vitals over Time - this enables you to review the patient’s vital signs over time.
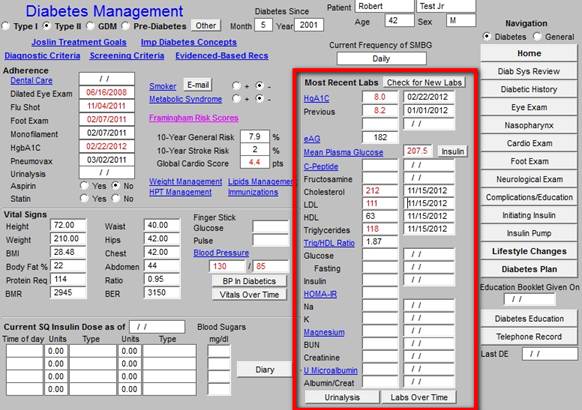
Column 2
This displays the Most Recent Labs and the date the test was done. The button entitled “Check for New Labs” when depressed will search for any newer labs than the ones displayed. The lab tests which are displayed are:
- HgA1C -
- Estimated Average Glucose (eAG - The eAG has been found to correlate with the HgA1c better than the Mean Plasma Glucose. Therefore when the patient is self monitoring and with their diabetes plan of care showing them the correlation, they can better predict what their HbA1c is.
- Mean Plasma Glucose - this is a calculation based on the HgA1C
Note: Launched from the Help Button entitled “Insulin" which is next to the mean Plasma Glucose is a document entitled “Summary of Treat-to-Target Trial: Randomized Addition of Glargine (Lantus) or Human NHP Insulin to Oral Therapy of Type 2 Diabetic Patients”
- C-Peptide - by clicking on the name, a document will launch which tells how the C-peptide is used clinically.
- Fructosamine - this test gives an estimate of the plasma blood glucose for the past 30 days.
- Cholesterol
- LDL
- HDL
- Triglycerides
- Trig/HDL Ratio - this ratio reflects the presence of insulin resistance if the ratio is above 2.
- Glucose
- Glucose Fasting
- Insulin - this should always be a fasting level.
- HOMA-IR - the Homeostasis Model Assessment of Insulin Resistance is a calculation based on the Fasting Insulin and Fasting Plasma Glucose. If the HOMA-IR is above 2, the patient is insulin resistant.
- Sodium
- Potassium
- Magnesium
- BUN
- Creatinine
- U Micoalbumin
- Albumin/Creatinine Ratio
- Urinalysis Button - this displays all of the elements of the urinalysis
- Labs Over Time Button - this shows the diabetes labs over time.
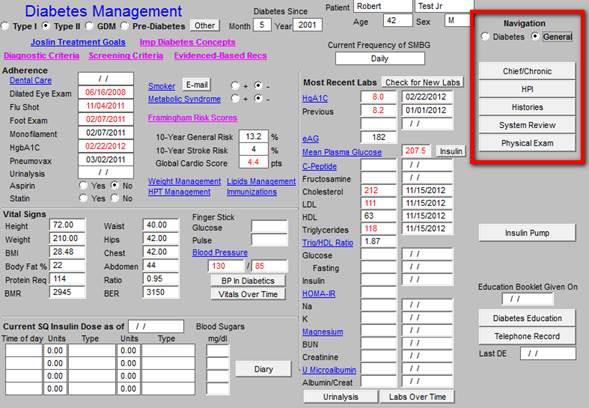
Column 3
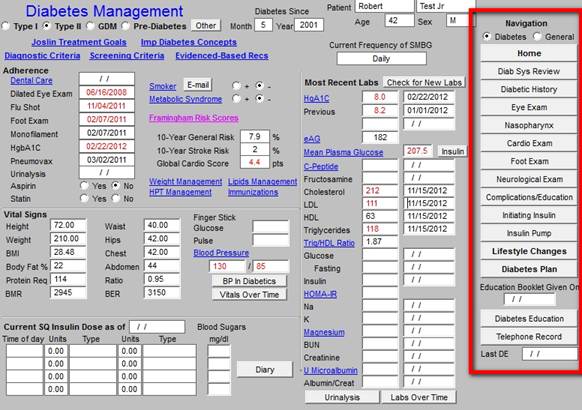
This column is entitled Navigation and presents SETMA’s Navigation Bar for the Diabetes Suite of
Templates. The first function is the choice between the Diabetes templates the General Templates.
If the check box beside the General is clicked, the following General Templates from the Master GP Suite of Templates will be displayed:
- Chief/Chronic - this is the chief complaint and Chronic conditions from the Master GP Suite of Templates.
- HPI - this is the History of Present Illness from the Master GP Suite of Templates.
- History - this is the History Template from the Master GP Suite of Templates.
- System Review - this is the Systems Review from the Master GP Suite of Templates
- Physical Examination - this is the Physical Examination from the Master GP Suite of Templates
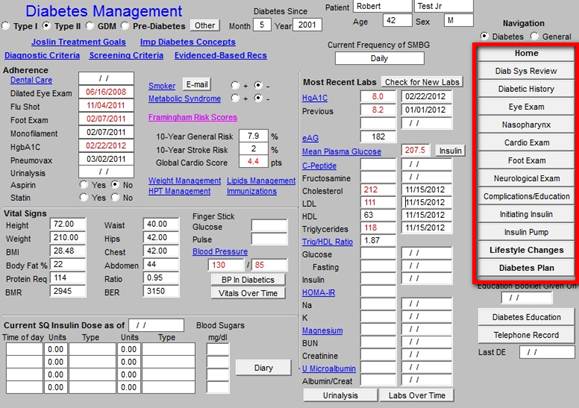
If the check box beside Diabetes is checked, the Diabetes Suite of Templates will be displayed. There are 15 functions here; they are:
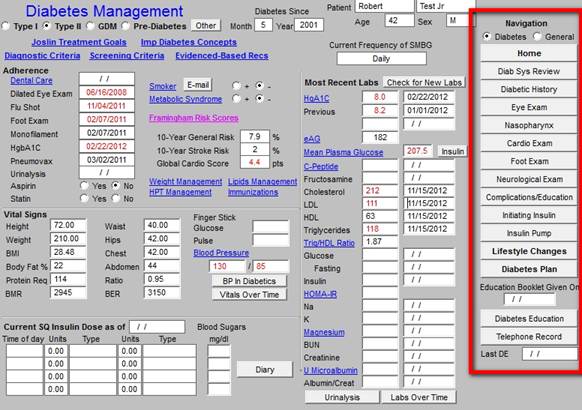
- Home - this navigates you back to the AAA Home template
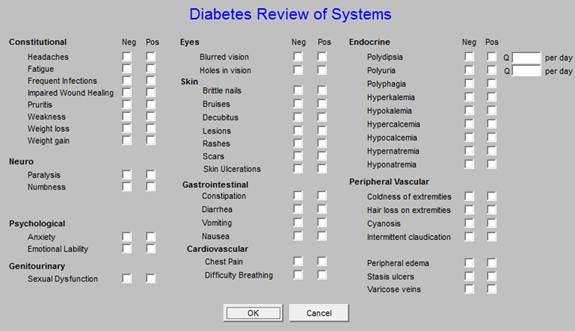
- Diabetes Systems Review - this is a ROS which is targeted for diabetes. All of the fields in this ROS interact with the ROS on the Master GP Suite of Templates’ Review of Systems.
- Diabetes History - this documents the patient-with-diabetes’:
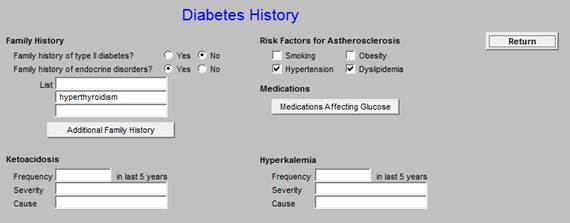
- Family History of Type 2 Diabetes
- Family History of Other Endocrine Disorders
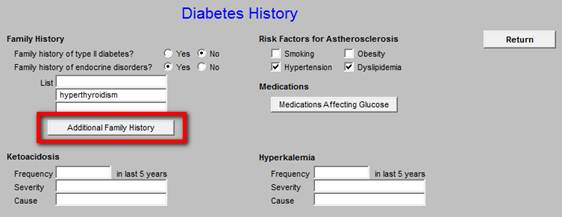
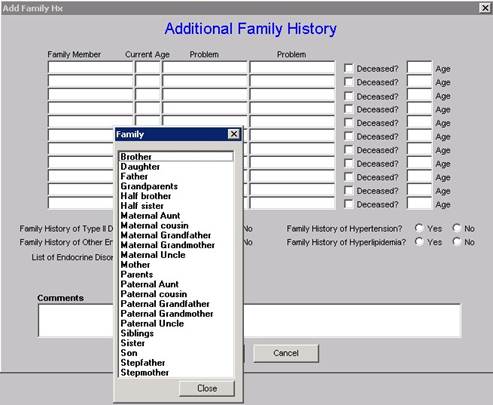
- Additional Family History
- Ketoacidosis
- Risk Factors for Atherosclerosis
- Smoking
- Obesity
- Hypertension
- Dyslipidemia
- Hyperkalemia
- Medications Affecting Glucose
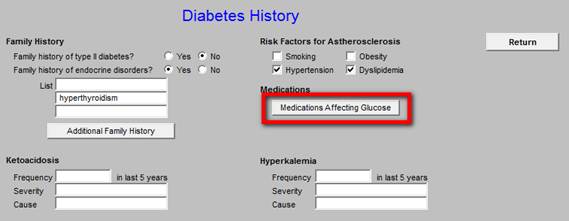
- Drugs with Well Established Affects on Blood Glucose
- Drugs that increase blood sugar
- Drugs that decrease blood sugar
- Drugs with Less Well Established Affects on Blood Glucose
- Drugs that increase blood sugar
- Drugs that decrease blood sugar

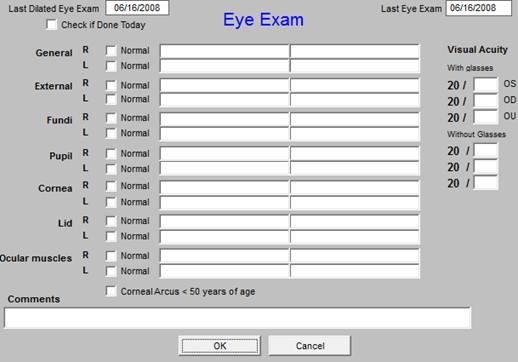
- Eye Exam - this is the eye examination template from the Master GP Suite of templates. It distinguishes between the dilated eye examination and the non-dilated eye exam done in the routine office visit.
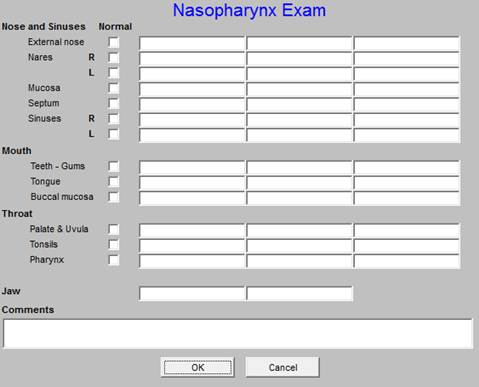
- Nasopharynx - this is the nasopharynx exam from the Master GP Suite of templates.
- Cardio Exam - this is the cardiovascular examination from the Master GP Suite of Templates.

- Foot - this has three pop-ups which are important:
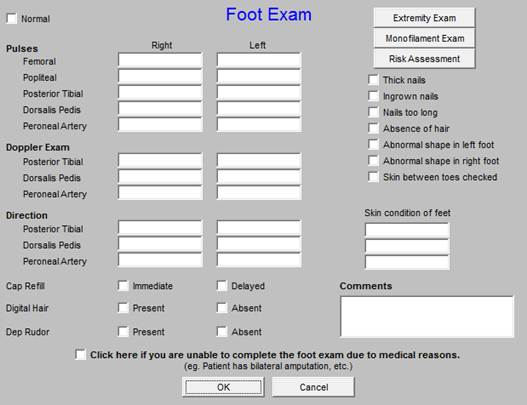
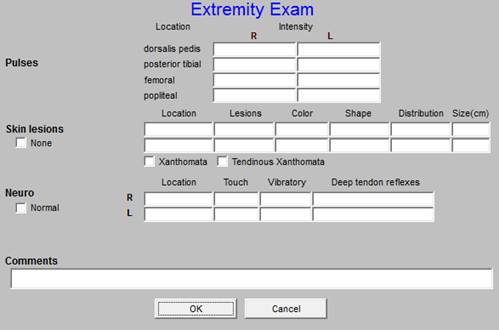
- Monofilament neuro-exam of the foot - also gives instructions on how to do monofilament examination.
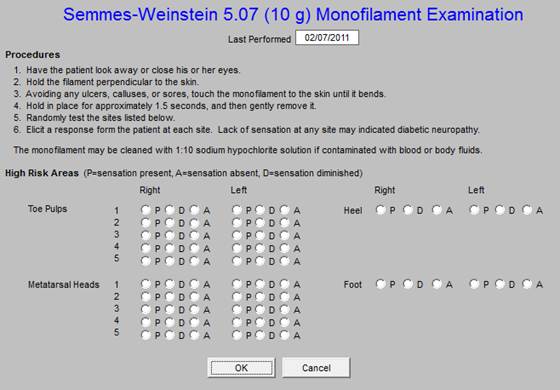
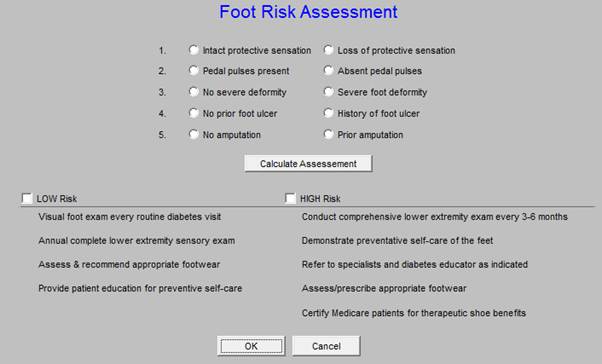
- This requires documenting the pulses, sensory status, deformity, ulcer, and amputations.
- When those entries are made by check boxes, activate the “calculation” button which will execute a plan of care for foot care, particularly important for the diabetic.
- This will print on the chart note.
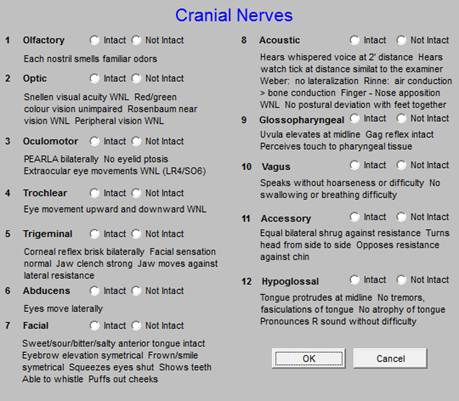
- Neurological Exam - this is the neurological examination from the Master GP Suite of Templates that includes 2 additional pop ups.
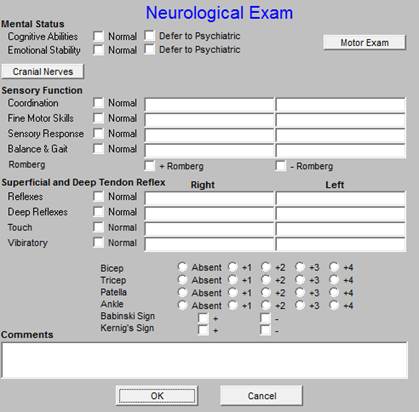
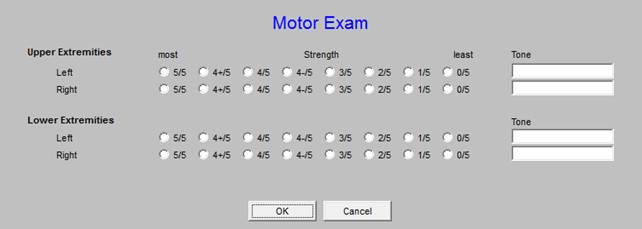
- Motor Exam - this template allows the documentation of a patient's level of strength
- Cranial Nerves - this function helps document the status of a patient's cranial nerves
- Complications/Education -
- The top portion of this template allows for the documentation of five complications of diabetes:
- Nephropathy - each of the complications categories allows for the documentation of the degree and nature of the complication via pick lists.
- Neuropathy
- Retinopathy
- Cardiovascular
- Peripheral Vascular
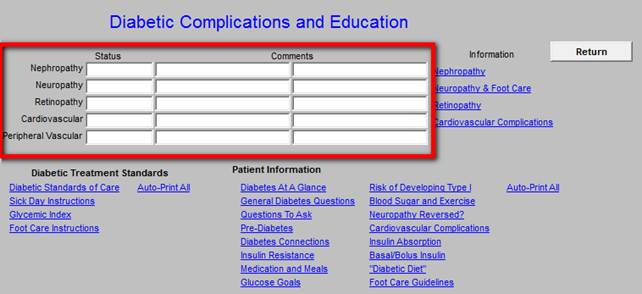
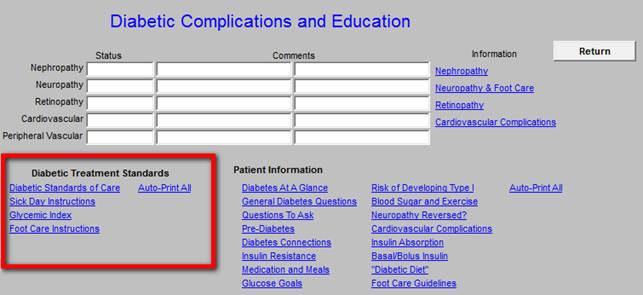
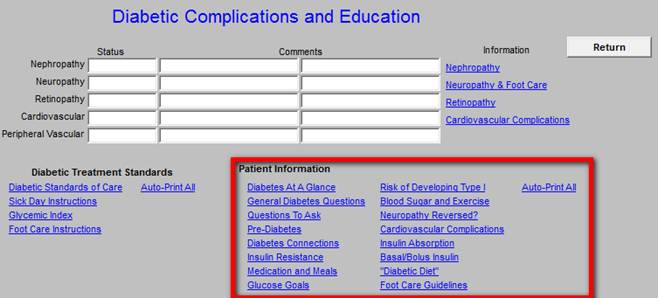
- The bottom portion of this template provides educational documentation for the patient:
- Diabetic Standards of Care
- A glycosylated hemoglobin (HbA1C) is recommended during an initial assessment and during follow-up assessments.
- A Fasting Lipid Profile is recommended during an initial assessment and during follow-up assessments.
- A urinalysis, including microalbuminuria and creatinine clearance, is recommended as part of an initial assessment and annually thereafter.
- A dilated eye examination is recommended during an initial assessment and at least annually thereafter.
- A foot examination --- visual inspection, sensory examination, and pulse examination -- is recommended during an initial assessment and during follow-up assessments.
- Influenza immunization is recommended for any person 6 months of age or older who, because of age or underlying medical condition, is at increase risk for influenza-related complications, which includes patients with diabetes mellitus.
- A blood pressure determination is recommended during an initial assessment and follow-up assessments.
- Follow-up assessments should be scheduled regularly.
- Sick Day Instructions
- Glycemic Index
- Foot Care Instructions
- Auto-Print All - This will print all 4 of the above documents.
- Diabetes At A Glance
- General Diabetes Questions
- Questions To Ask
- Pre-Diabetes
- Diabetes Connections
- Insulin Resistance
- Medications and Meals
- Glucose Goals
- Risk of Developing Type I
- Blood Sugar and Exercise
- Neuropathy Reversed?
- Cardiovascular Complications
- Insulin Absorption
- Basal/Bolus Insulin
- "Diabetic Diet"
- Foot Care Guidelines
- Auto-Print All - This will print all 16 of the above documents.
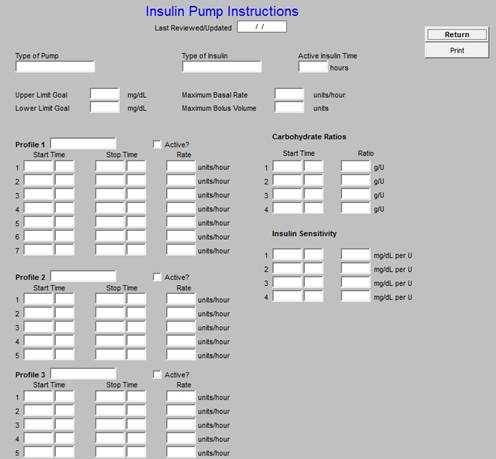
- Insulin Pump- this is a screen which allows you to document details instructions for a patient’s insulin pump if they use one. Completing this template satisfies two goals. First, it ensures that patient knows how their insulin pump should be configured. Second, it allows the patients pharmacists to provide the correct amount of insulin.
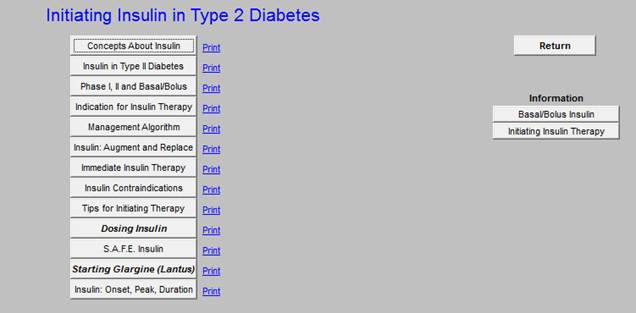
- Initiating Insulin - this is a tutorial on how to start insulin on a patient. It includes the following functions:
- Concepts about insulin
- Insulin in Type 2 Diabetes
- Phase 1, II and Basal/Bolus
- Indications for Insulin Therapy
- Management Algorithm
- Insulin, Augment and Replace
- Immediate Insulin Therapy
- Insulin Contraindications
- Tips for Initiating Therapy
- Dosing Insulin - this calculates the beginning insulin doses for you.
- S.A.F.E. Insulin
- Starting Glargine (Lantus) - this calculates the beginning Lanus dosage for you.
- Insulin, Onset, Peak, Duration
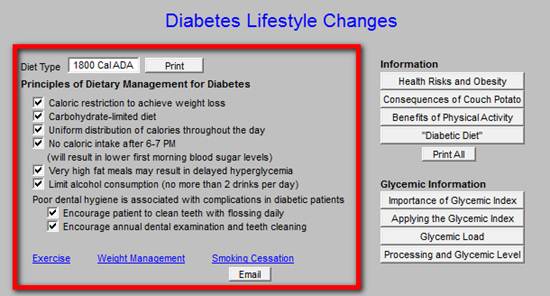
- Lifestyle Changes - there are two columns on this template
- Diet type - a space for the patient’s diet to be displayed.
- Principles of Dietary Management for Diabetes - Six Dietary principles which will help improve glycemic control
- Poor Dental Hygiene - documentation for encouraging the patient with diabetes to maintain their dental health.
- Across the Bottom there are hyperlinks to:
- Exercise
- Weight Management
- Smoking Cessation with an e-mail button for sending an electronic tickler file for smoking cessation.
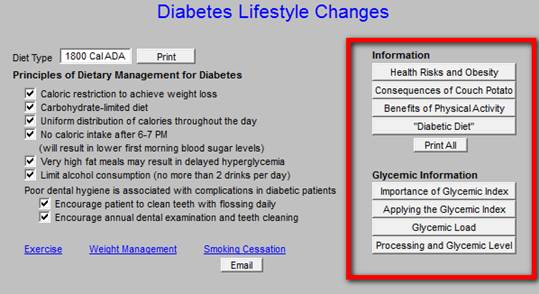
- Health Risk and Obesity
- Consequences of Couch Potato
- Benefits of Physical Activity
- “Diabetic Diet”
- Print All of the above Button
- Glycemic Information for Patient
- Importance of Glycemic Index
- Applying the Glycemic Index
- Glycemic Load
- Processing Food and Glycemic Index
- Button to print all four articles
- Diabetes Plan - this is discussed below
- Education Bulletin Given on - this is the last date that SETMA’s Diabetes Education Booklet was given.
- Diabetes Education Button - this launches the Diabetes Education Template.
- Last Diabetes Education - this indicates when the patient last attended Diabetes Education classes.
Diabetes Plan Template
Because of its importance, this is discussed as a separate section.
At the top of the template are:
- Title Bar
- Menu Bar
- Top Tool Bar
- Title of the Template
For more information on the NextGen Toolbar, Click Here.
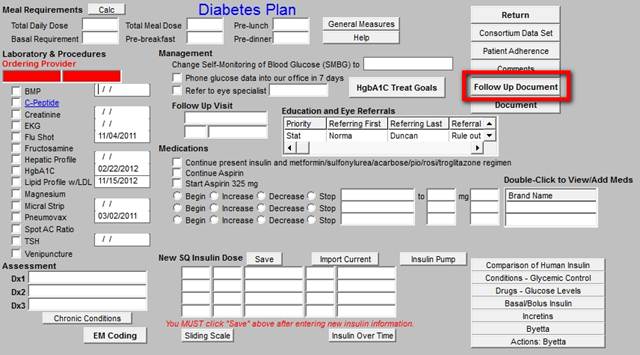
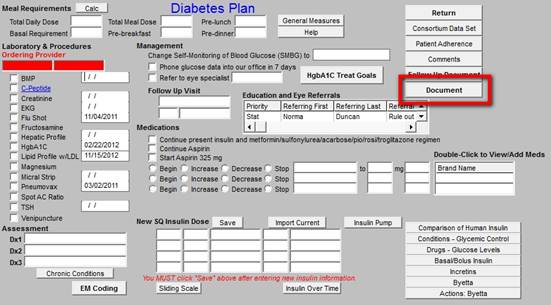
To the far right of the Diabetes Plan Template are:
- Navigation Button to take you back to Diabetes Master Template
- Consortium Data Set - discussed earlier
- Patient compliance - discussed earlier
- Comments - a place to add additional comments if needed
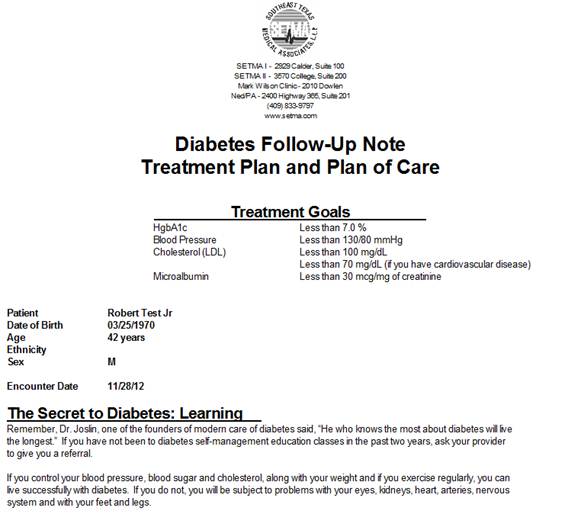
- Follow-up Document - a button to launch the production of a follow-up note which should be given to the patient at every visit. The follow-up note gives the patient key information about how to take care of themselves, about their most recent lab results and about their medications.
- Document - this button will generate the Diabetes Chart Note
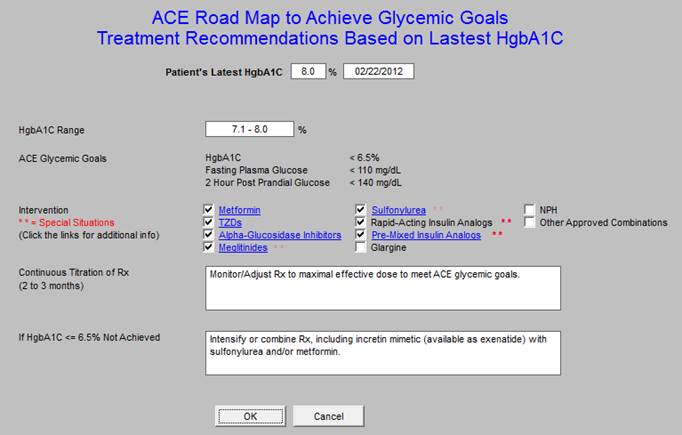
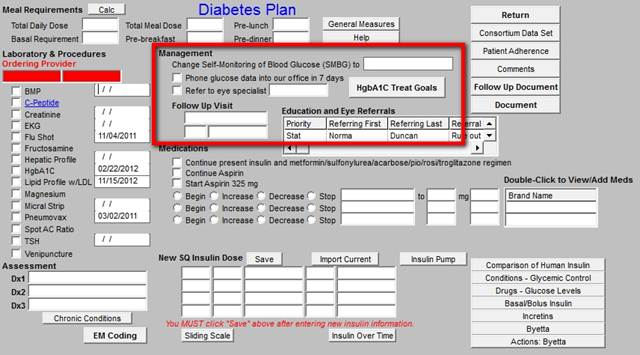
ACE Roadmap to Achieve Glycemic Goals, Treatment Recommendations Based on Latest HGA1c
When the diabetes plan template is deployed and if the HbA1c is not to goal, a pop-up will automatically appear which is entitled ACE Roadmap to Achieve Glycemic Goals, Treatment Recommendations Based on Latest HGA1c.
The following screen shot of the Diabetes Plan shows the button to launch this function outlined in red.
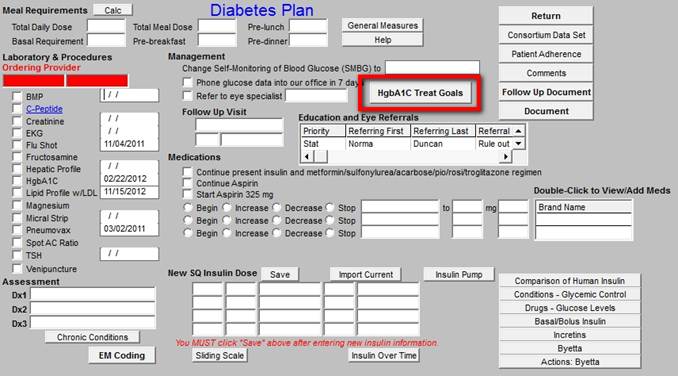
The pop-up can be launched automatically if the HbA1c is not to goal or it can be launched by clicking the button entitled, HbA1c Treat Goal. The ACE is the American College of Endocrinology.
The navigation buttons on the Disables Plan are outlined in red.
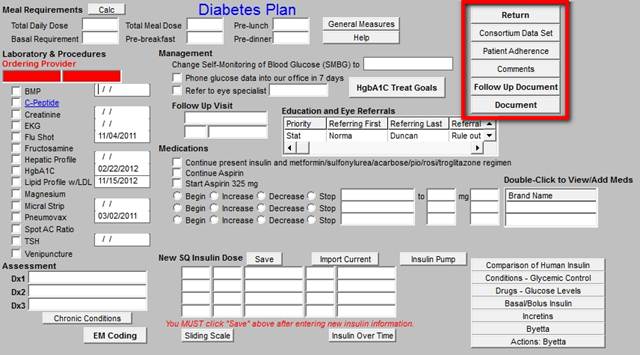
From Top to Bottom, the Diabetes Plan Template is organized into three sections. Top Section:
- This is titled Meal Requirements (Insulin)
When the New Subq Insulin Dose is completed at the bottom of the screen and the “save” button” is depressed, the following information about the patient’s insulin is automatically generated. This prints on the follow-up note which you will give to the patient.
- Total Daily Dose
- Basal Requirements
- Total Meal Dose
- Pre-breakfast
- Pre-lunch
- Pre-dinner
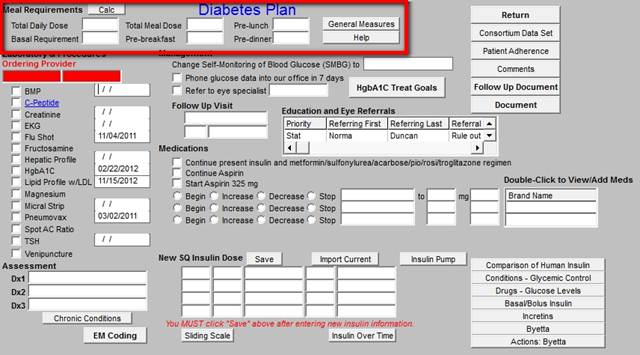
- General Measures -- This launches a pop-up with the ability to order:
- Home glucose monitoring
- Exercise
- Reduce Weight
- Follow ADA Diet
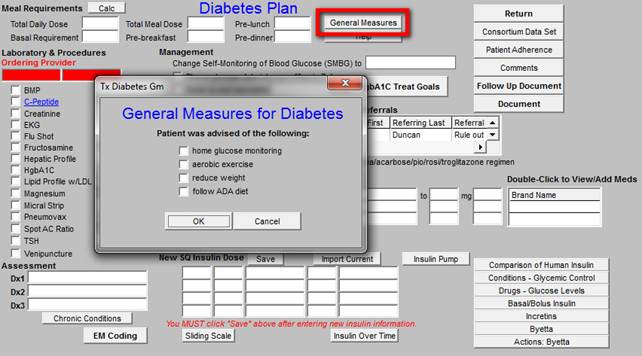
Any of these that are checked will print on the chart follow-up note which you will give to the patient.
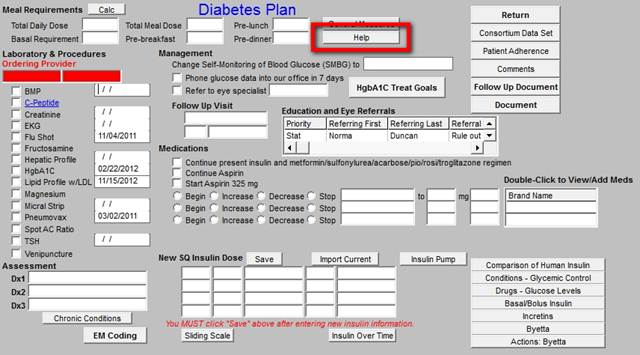
- Help - this launches a pop-up entitled “Strategies for Achieving Glycemic Control in Type 2 Diabetes”
The Middle Section contains:
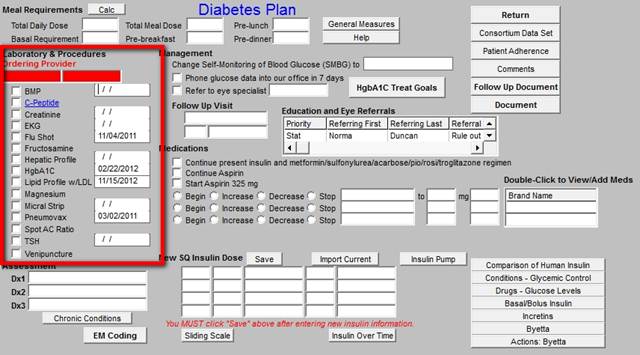
- Laboratory and Procedures - it is possible to charge post these studies from the Diabetes Plan Template. The process is simple:
- Add the diagnosis to the Assessment box below
- Check the boxes by the tests you wish to order
- Click the “Submit Labs” box in the bottom section of this template.
The tests and procedures which can be ordered from the Diabetes Plan template are:
- BMP
- C-Peptide
- EKG
- Flu Shot
- Fructosamine
- Hepatic Profile
- Magnesium
- Microalbumin
- Pneumovax
- Spot AC Ratio
- TSH
- Venipuncture
- Change Self-monitoring of Glucose to (SMBG) - there is a box with a pick list which allows the following choices: QD, QID, QOD, BID.
- Phone Glucose data into our office in 7 days - there is a check box to activate this so that it prints on the follow-up note.
- Refer to Eye Specialist - when the box next to this function is checked, it allows you to select an Ophthalmologist. In the next line is the referral template can be accessed by double clicking in the space to complete the eye referral.
- Follow-up visit - patients with diabetes ought to be seen at a minimum of three times a year.
- Medications - check boxes are present which allows you to document instructions to:
- Continue present insulin and metformin etc.
- Continue Aspirin
- Start Aspirin 325 mg
- Begin, Increase Decrease
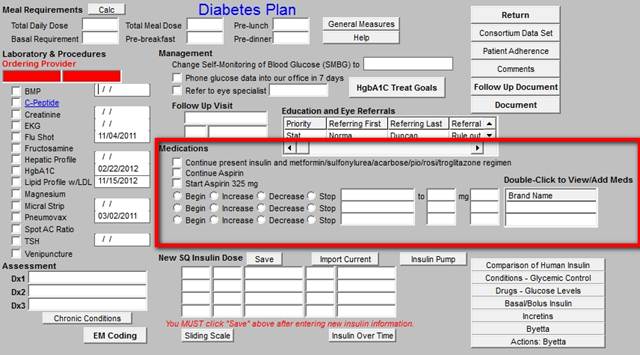
NOTE: For more information on using the Medication Module, Click Here
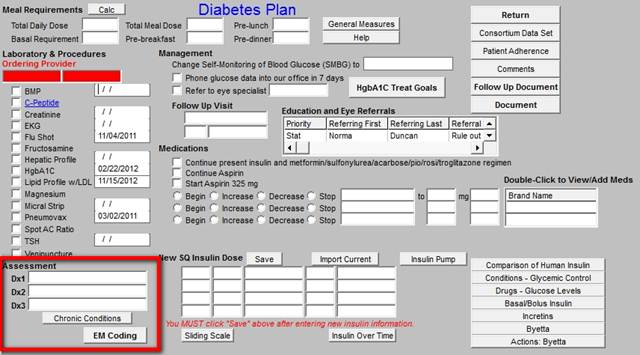
The bottom section of the template contains:
- Three boxes for diagnoses; the top box only has Diabetes ICD-9 codes attached.
- Chronic Conditions - a button which launches the patient’s chronic condition
- Submit Labs - a button which submits the lab requests to the lab and the charges to charge posting.
- EM Coding
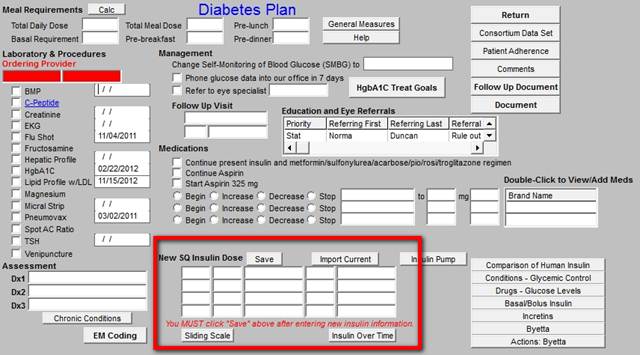
- Import Current - this moves the insulin dosing which is displayed on the Master Diabetes Template to the Plan Template
- Save - once any changes are made, this button saves the new insulin dosing and places it in the basal and meal categories at the top of the Diabetes Plan Template.
- Sliding Scale - this allows a sliding scale to be selected based on the patient’s insulin sensitivity.
- Insulin over time - this allows you to view the insulin dosing over time.
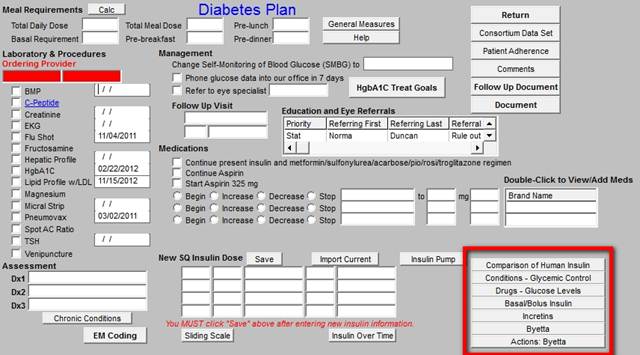
- Printable Provider Education Materials on:
- Comparison of human insulins
- Conditions - Glycemic Control
- Drugs - Glucose Levels
- Basal/Bolus Insulins
- Incretins
- Actions Byetta
The last action is to create the Diabetes Follow-up Note, which is the Diabetes Treatment Plan and Plan of Care, and to give it to the patient and then to create the Diabetes Chart Note.
Analytics and Diabetes
From the work documented in the Diabetes Disease Management Tool, the following analytics can be done.
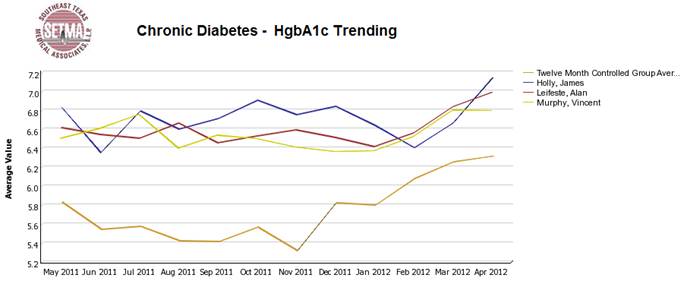
Through this longitudinal display, in 2009, we discovered that our patients who were well controlled all year were often losing their control of diabetes in October, November and December. We then did further audits to see if they were being seen less often and being tested less often and they were. In 2010, in September, we sent letters to all 7,000+ patients with diabetes alerting to this fact. We indicated we wanted them to enjoy holiday celebrations but to maintain their exercise and dietary discretion. We had them sign a contract to be seen twice in those three months and to be tested twice. In 2011, our audit showed that this phenomenon had disappeared.
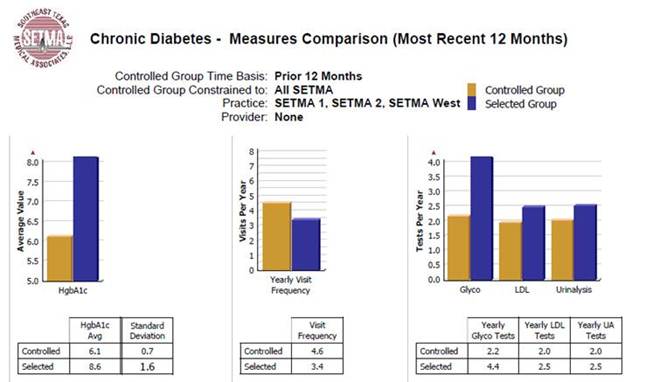
The above compares the standard deviation of our controlled patients with diabetes (gold) and that of the uncontrolled. We established our goal to be .7 for our diabetes populations. We discovered that our controlled patients were seen 1.2 times more often. This is statistically significant and we saw an opportunity to improve the control of all of our patients by making sure that all patients with diabetes had 4-5 visits a year.
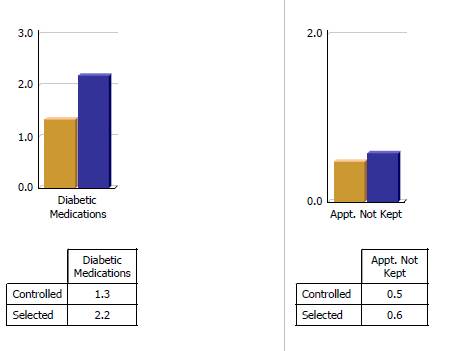
No leverage points for improvement were found in the data above. (the controlled are gold and are patients with diabetes treated to goal and the selected are the uncontrolled patients in purple)
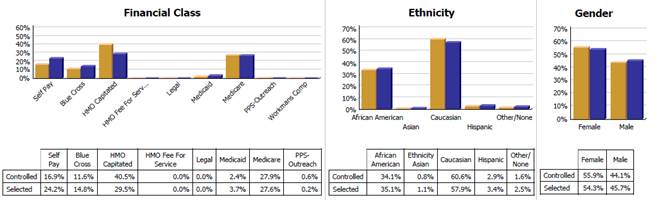
From the above, we found that our HMO capitated patients who have a zero office co-pay are treated more effectively than Fee-for-Service Medicare allowing the inference that the cost of care for the FFS Medicare patients is a barrier to the effectiveness of care in that when that barrier is removed in a similar population that the care improves. We were able to see that for diabetes we had eliminated ethnic disparities of care.
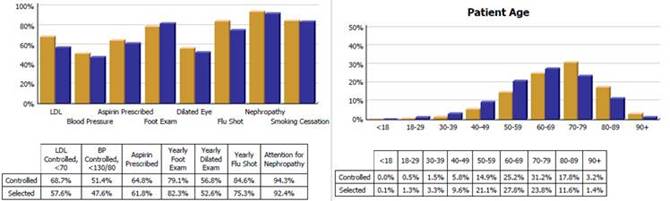
From the above profile, we were able to see that our older patients have better control of diabetes than our younger patients. Concerned that this might reflect co-morbidities rather than excellence of care, we tested the patients for malnutrition (pre-albumin), weight loss and appetite and found that they were not malnourished but were responding well to increased attention.
|