|
The Hypertension Suite of Templates have been designed to make it possible to efficiently and excellently document the proper care of hypertension and to simultaneously provide the opportunity for healthcare providers to improve their understanding of the disease, while evaluating the quality of care they personally give to patients with hypertension. At present, over 50% of the patients who are treated by SETMA have a diagnosis of hypertension making its treatment a key element in our delivery of quality healthcare.
There is no condition which is not worsened by the concomitant presence of hypertension and there are few chronic conditions which are as devastating to the health and well being of a patient as that of elevated blood pressure. Finally, the complexity of the treatment of hypertension is compounded by the fact that so many special cases exist each of which requires different considerations for the proper treatment of high blood pressure.
On the other hand, few chronic conditions offer the promise as does the effective treatment of hypertension. The consequences of untreated hypertension are grave, but the results of effective control of hypertension are gratifying. However, the reality is that the overwhelming majority of patients with hypertension are inadequately treated.
It is for all of these reasons that SETMA's Hypertension Suite of Templates not only offers a tool for the documentation of the patient's hypertension treatment but also provides information, insight and algorithms for the analysis of a patient's blood pressure treatment and control in:
- The evaluation of secondary hypertension
- The presence of Dippers and Non-Dippers
- White Coat Syndrome and its cardiovascular risk
- Diabetes
- Depression
- The elderly
- Insulin Resistance
- Isolated Systolic Blood Pressure
- Kidney Disease
- Medication selection in dozens of comorbid conditions
The following is not only an explanation of how to use SETMA's Hypertension Suite of Templates, but it is also a structure for logically approaching the treatment of hypertension along with a wealth of information and insight about that treatment.
The Hypertension Suite of Templates can be accessed from:
AAA Home
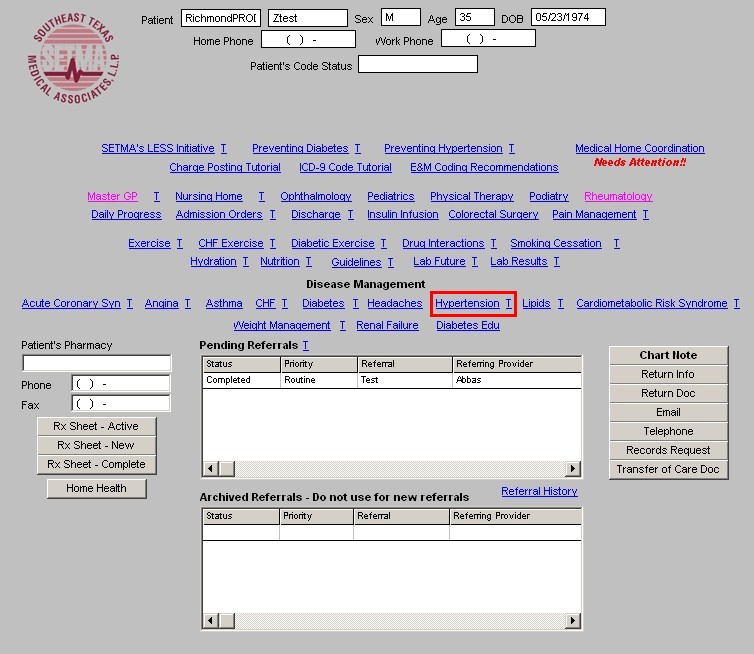
Main Tool Bar
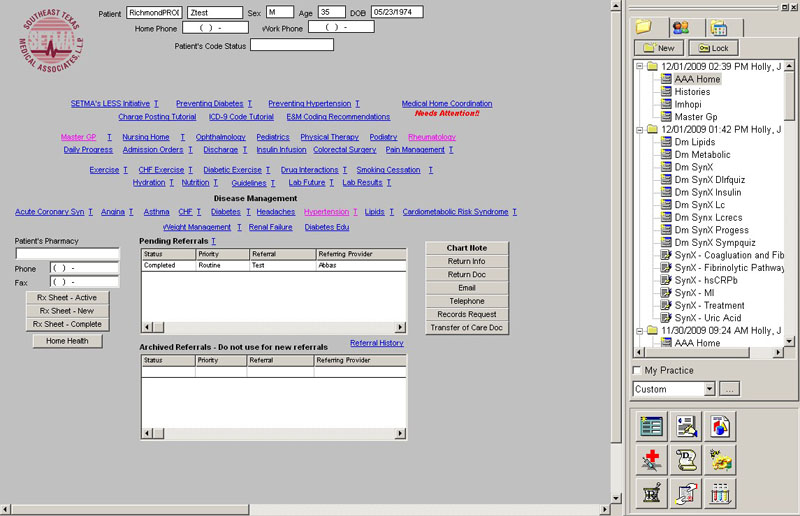
- When the Template button is clicked you will be presented with the preference list.
- If the Hypertension Master Template is listed as one of your preferences, select it.
- If it is not one of your preferences, select the All radio button and then scroll down until you find it in the list.
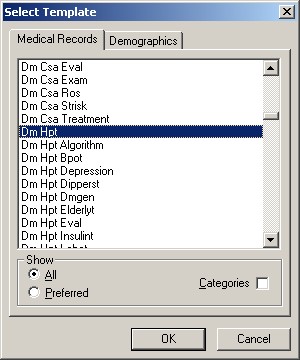
NOTE: For more on how to set up your preferences, Click Here
Other Disease Management Tools Hyperlinks
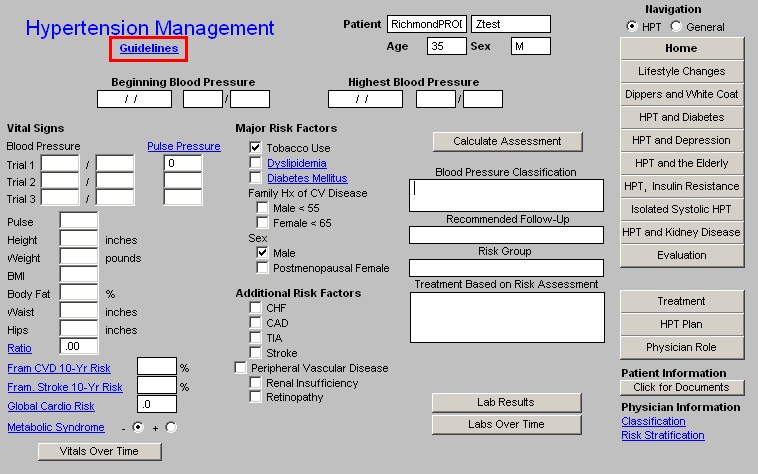
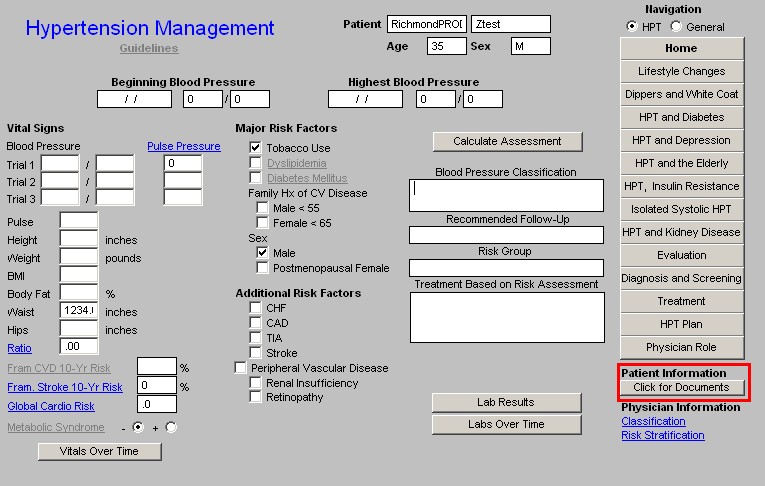
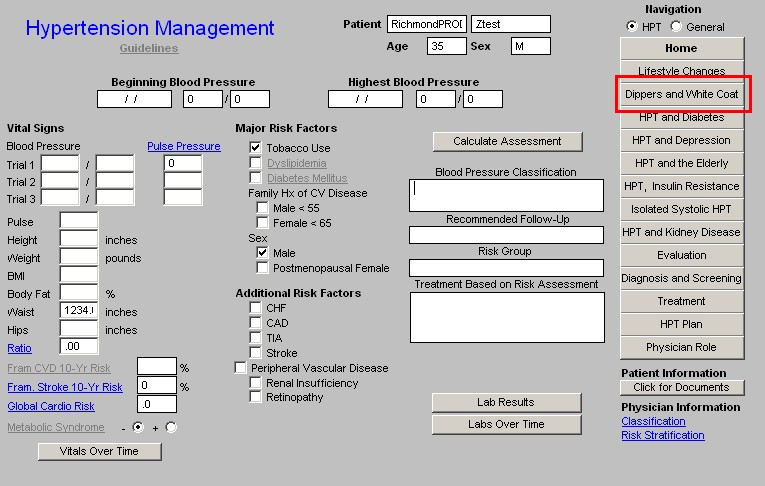
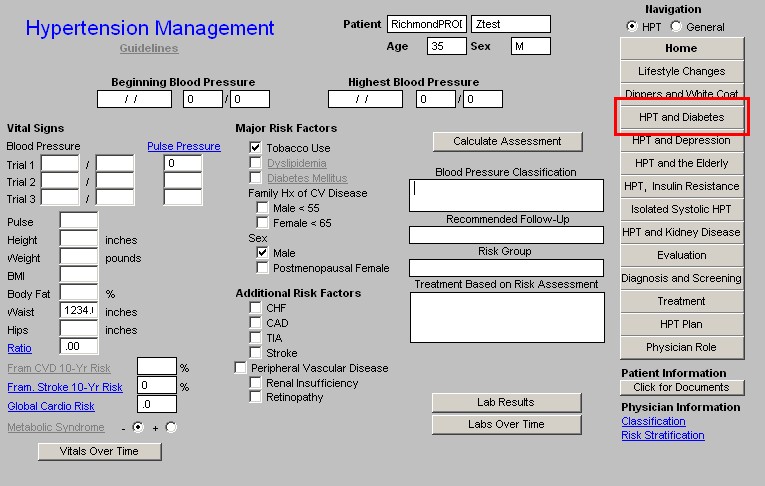
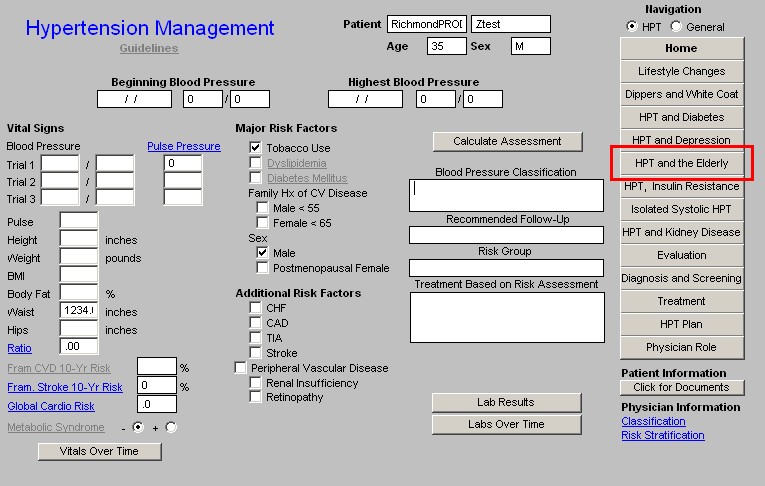
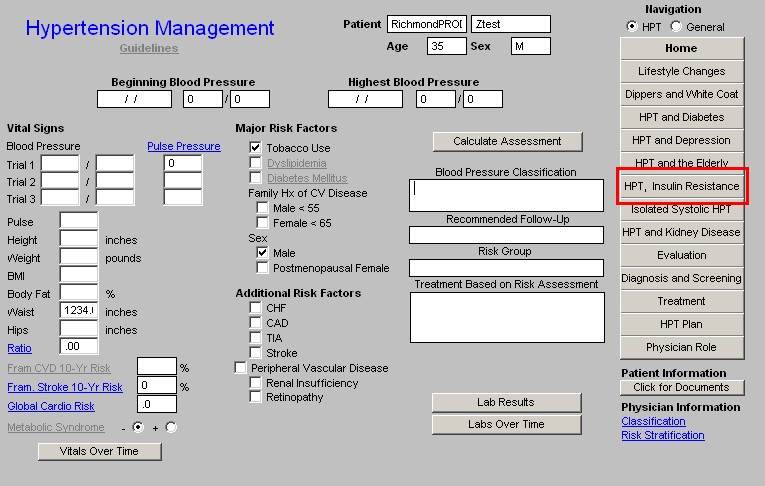
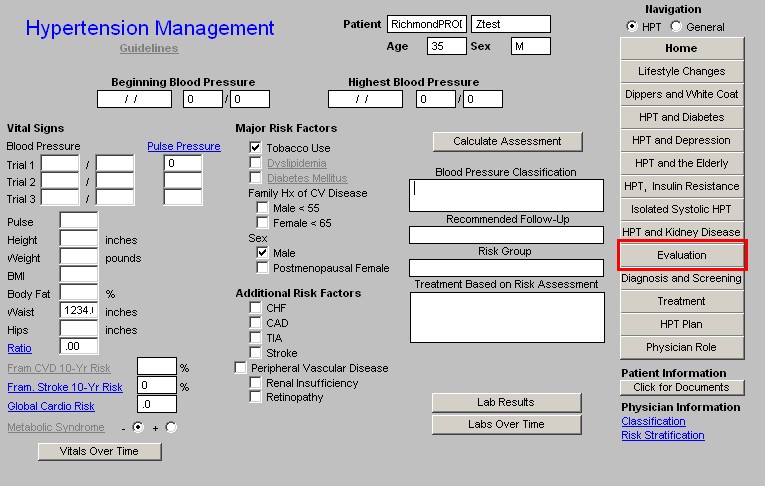
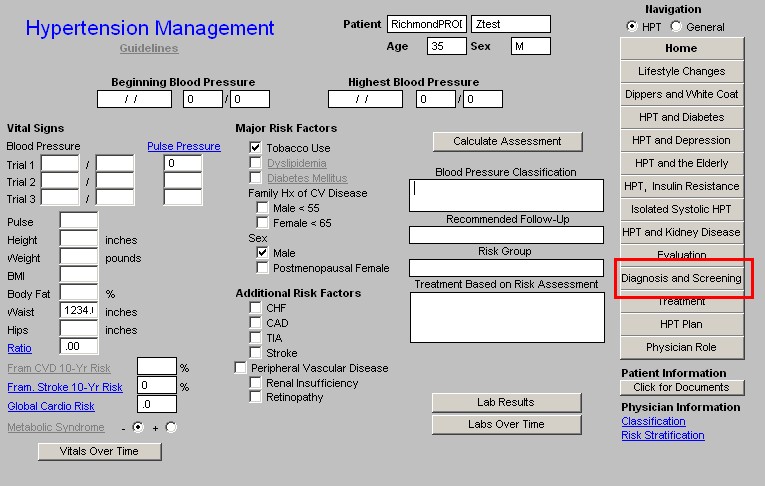
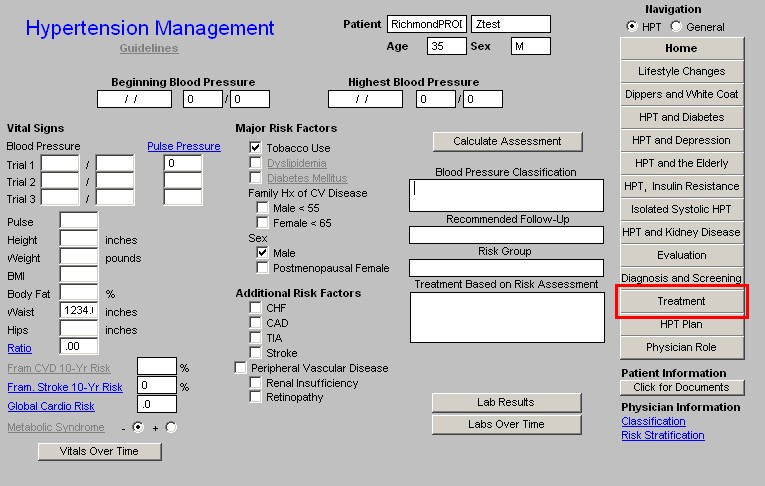
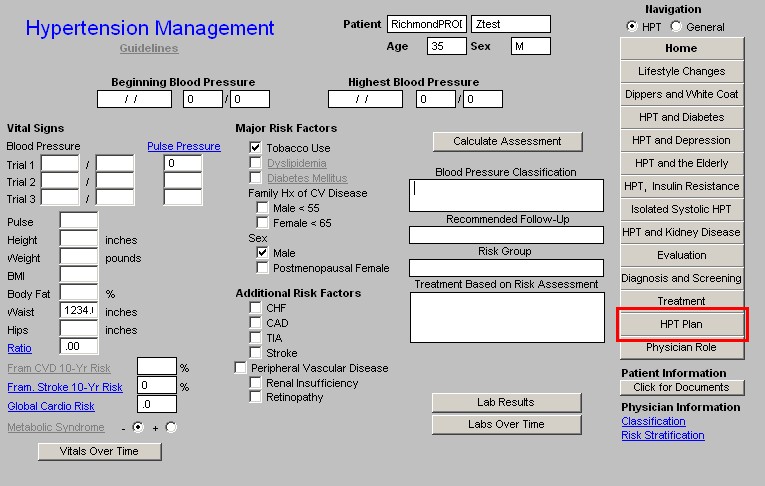
The Master Hypertension Template provides the entry point into the management of hypertension
Information at the top of the Master Hypertension Template
- Title
- Guidelines - this is a hyperlink which launches a list of General Hypertension Guidelines about blood pressure management. These are listed below.
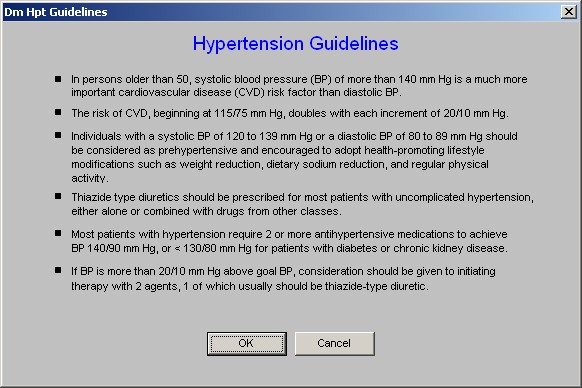
- The General Hypertension Guidelines provide the imperative for effective blood pressure control. The Guidelines state:
- In persons older than 50, systolic blood pressure (BP) of more than 140 mm Hg is a much more important cardiovascular disease (CVD) risk factor than diastolic BP.
- The risk of CVD, beginning at 115/75 mm Hg, doubles with each increment of 20/10 mm Hg.
- Individuals with a systolic BP of 120 to 139 mm Hg or a diastolic BP of 80 to 89 mm Hg should be considered as pre-hypertensive and encouraged to adopt health-promoting lifestyle modifications such as weight reduction, dietary sodium reduction, and regular physical activity.
- Thiazide type diuretics should be prescribed for most patients with uncomplicated hypertension, either alone or combined with drugs from other classes.
- Most patients with hypertension require 2 or more antihypertensive medications to achieve BP 140/90 mm Hg, or < 130/80 mm Hg for patients with diabetes or chronic kidney disease.
- If BP is more than 20/10 mm Hg above goal BP, consideration should be given to initiating therapy with 2 agents, 1 of which usually should be thiazide-type diuretic.
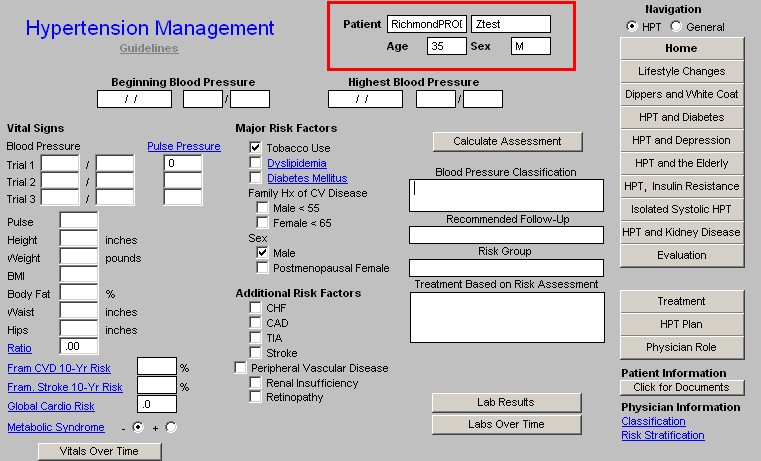
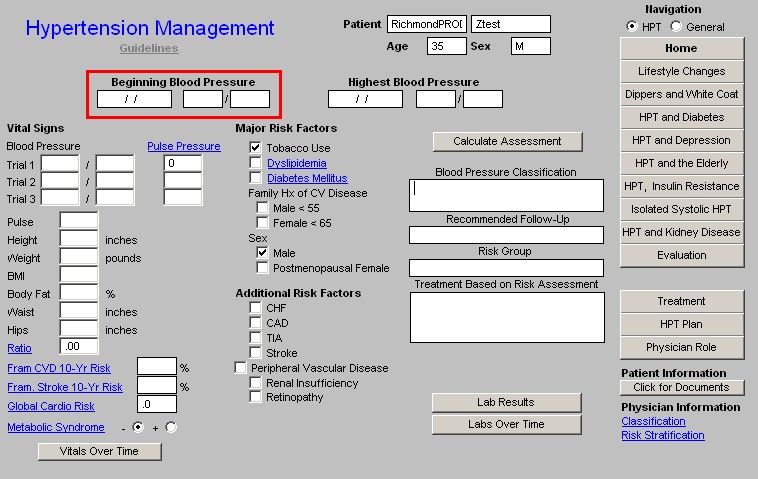
- Beginning Blood Pressure - this is the blood pressure from the first visit when the Master Hypertension Template was accessed, not the blood pressure from the first time the patient was seen by a SETMA Provider.
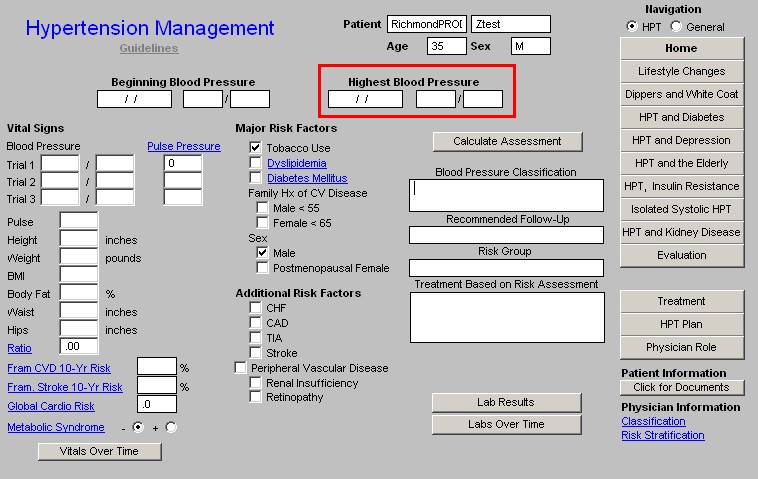
- Highest Blood Pressure - this is the highest blood pressure measured at a time when the Master Hypertension Template was accessed. If a higher blood pressure was recorded on a patient when the Master Hypertension Template was not accessed, it will not be recorded here.
Beneath the above information, the remainder of the Hypertension Master Template is organized into four columns:
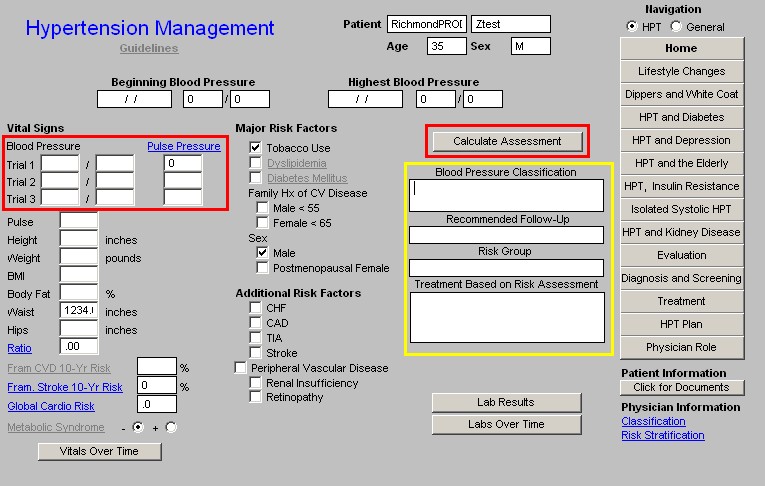
Column 1 -
Vital signs
- Blood Pressure
- Trial 1
- Trial 2
- Trial 3
- Pulse
- Height
- Weight
- BMI
- Body Fat
- Waist
- Hips
- Ratio
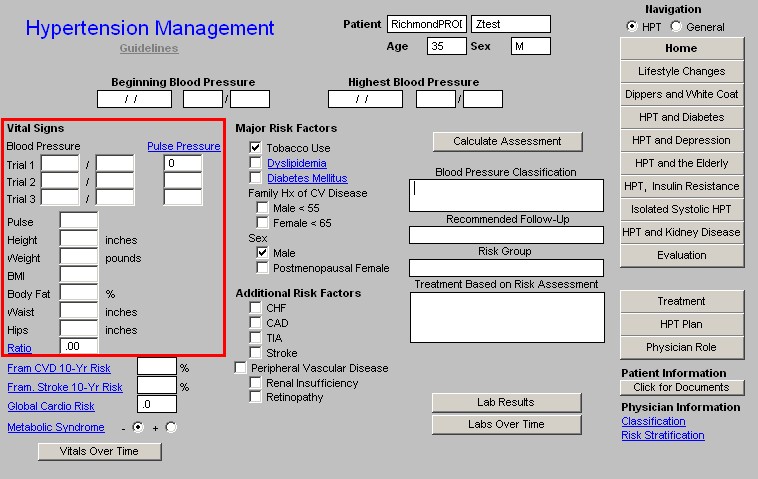
Fram CVD 10-Yr Risk - this is a hyperlink which takes you to the Framingham Risk Template where the Cardiovascular and Stroke Risk are calculated from the Framingham Data and where the Global Cardio Risk is also calculated. The results of all three are displayed here. This enables a provider to address the cardiovascular and cerebrovasculer risk burden carried by the patient and thus to design a treatment program based on that risk.
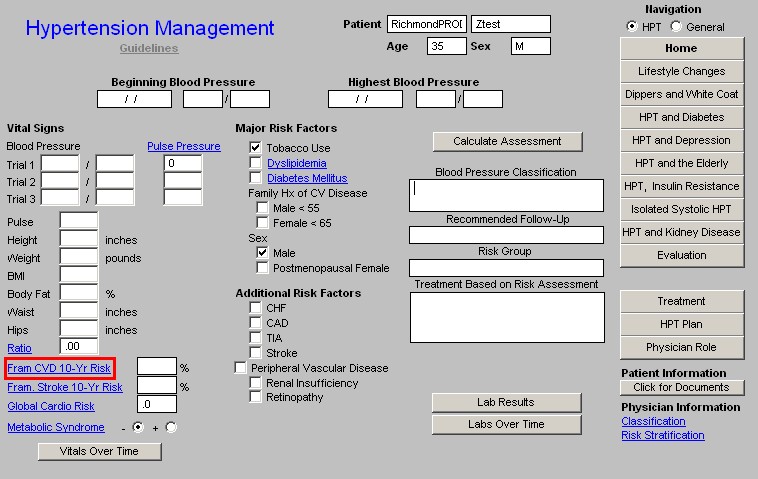
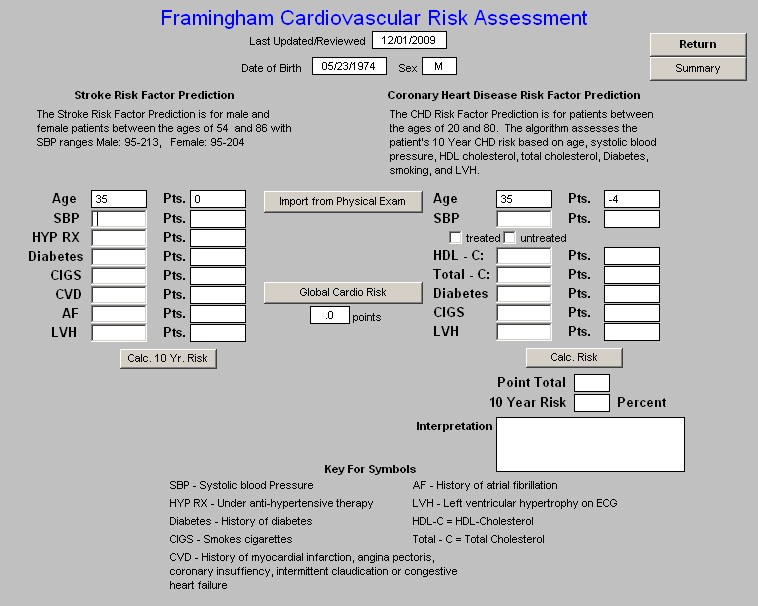
Fram. Stroke 10-Yr Risk - same as above.
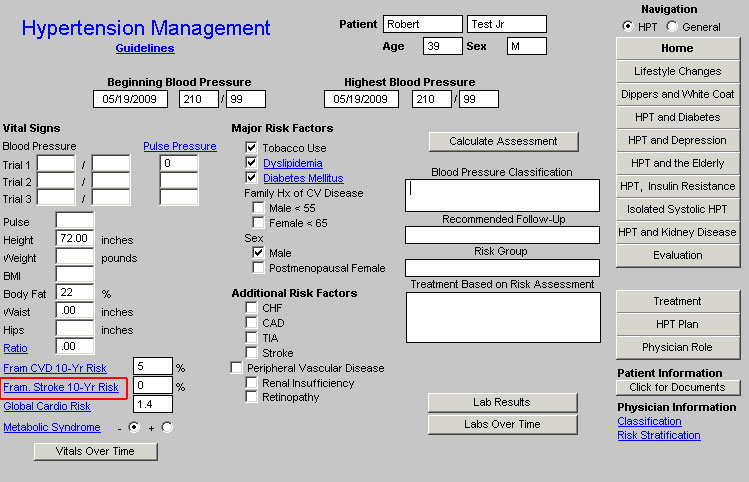
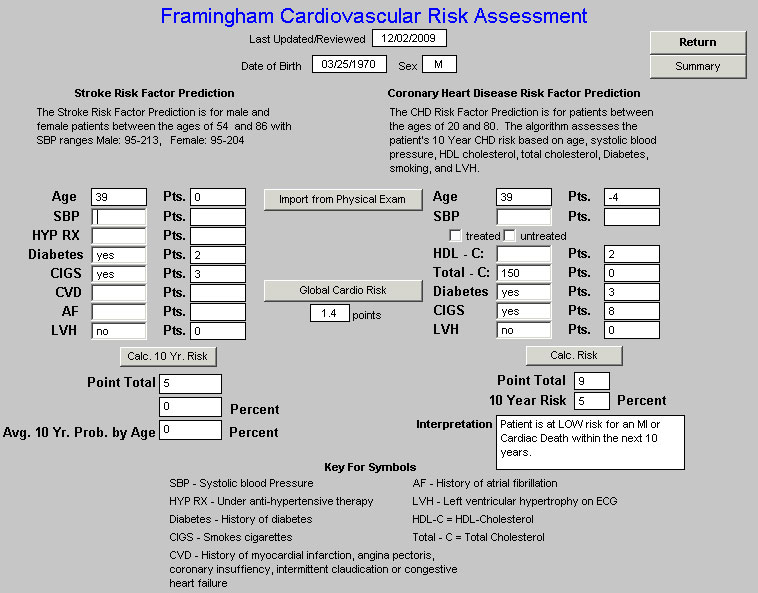
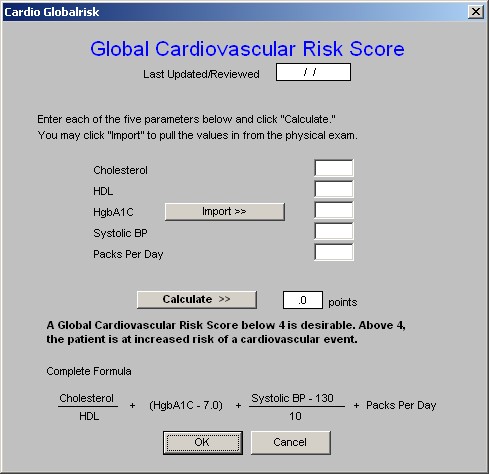
Global Cardio Risk - this is a new risk calculation based on the Framingham data but without the non-modifiable risk factors - age, sex, etc - included in the equation. A score of 4 or more represents an increased cardiovascular risk.
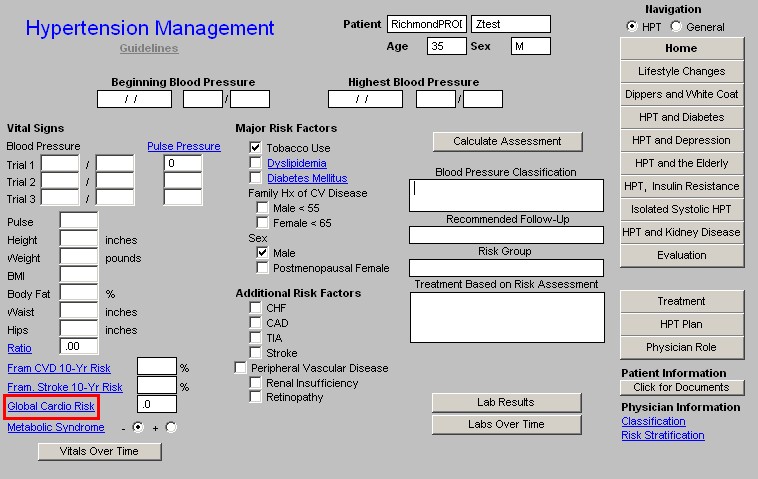
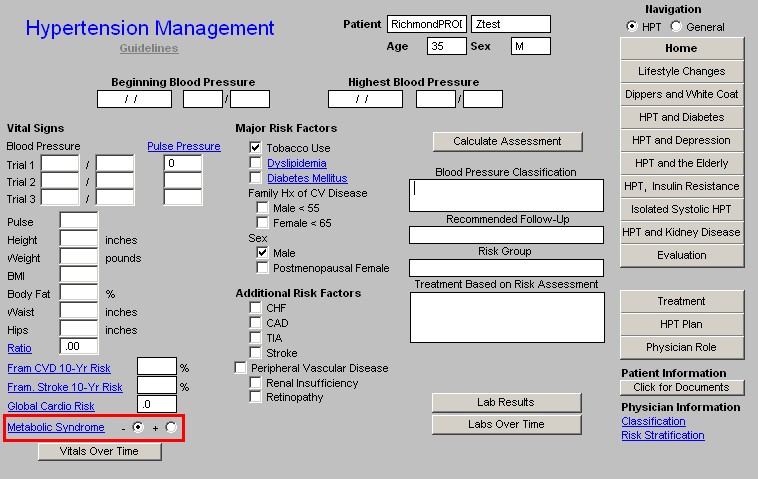
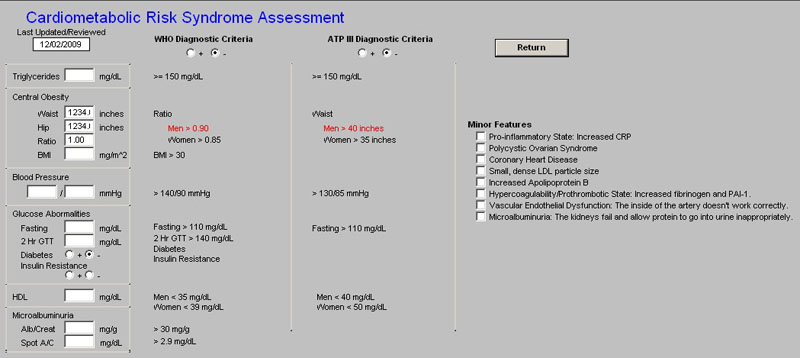
Metabolic Syndrome
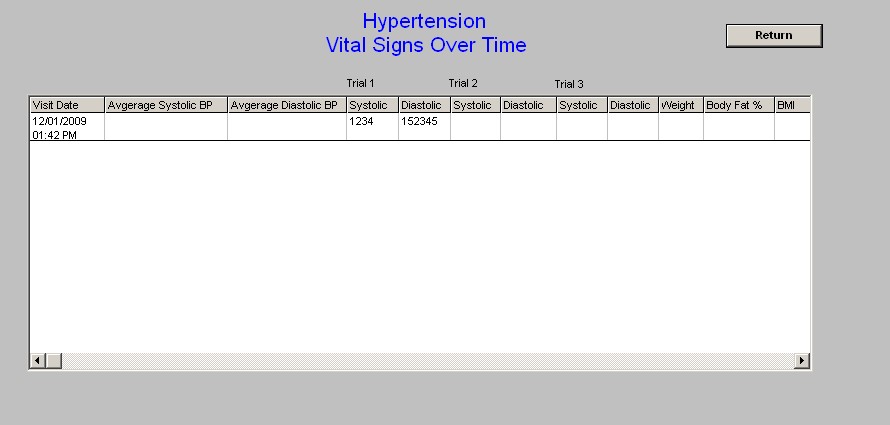
Vitals over Time - this function displays the vital signs over time. This is a very useful tool to look at patterns and possible seasonal changes in blood pressure, etc.
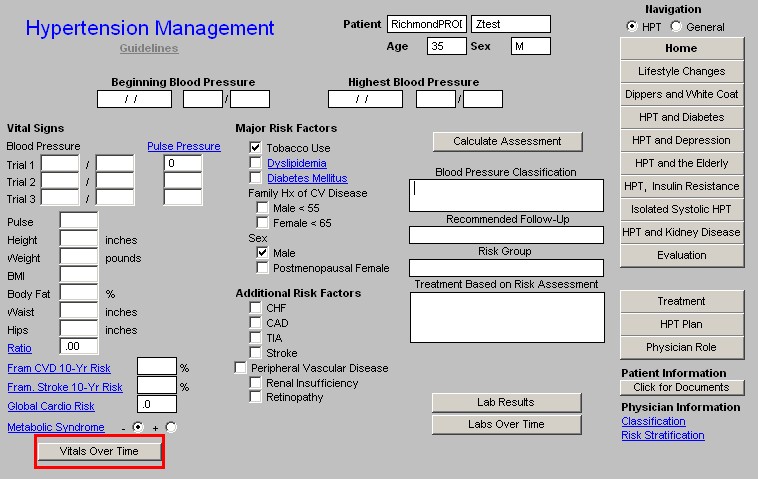
Column 2 --
Major Risk Factors (Cardiovascular Disease Risk)
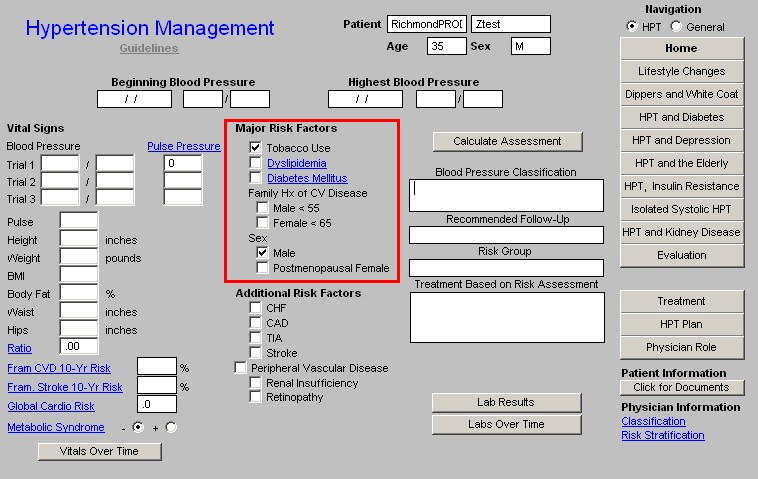
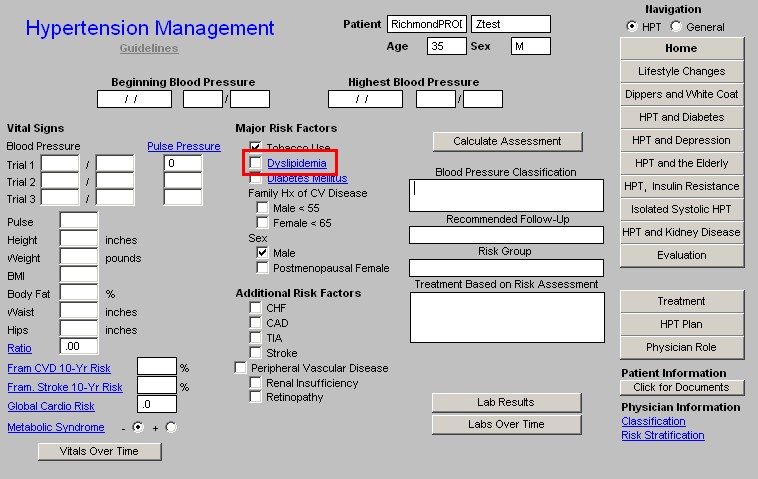
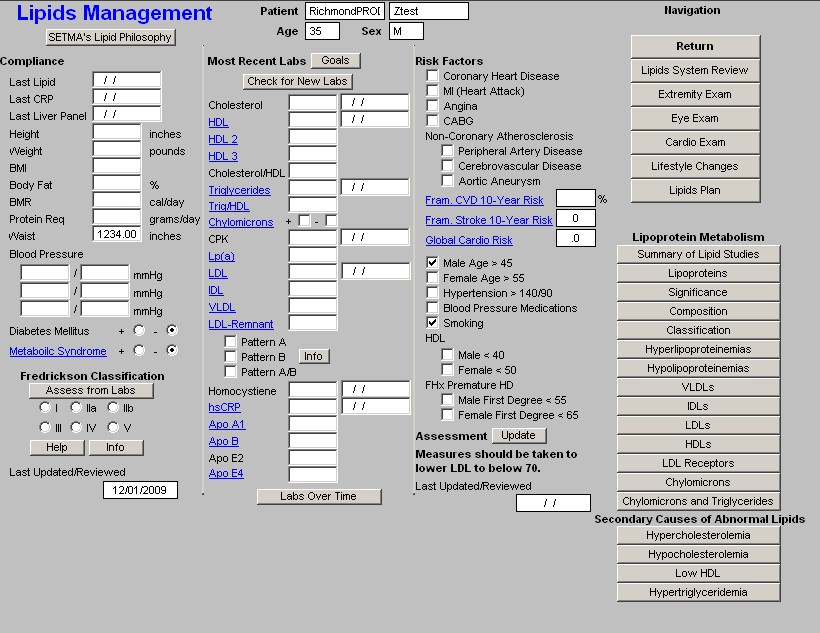
Depressing the Dyslipidemia button launches the Lipid Management Suite of Templates beginning with the Master Lipid Management Template. For more information on the Master Lipid Template, Click Here.
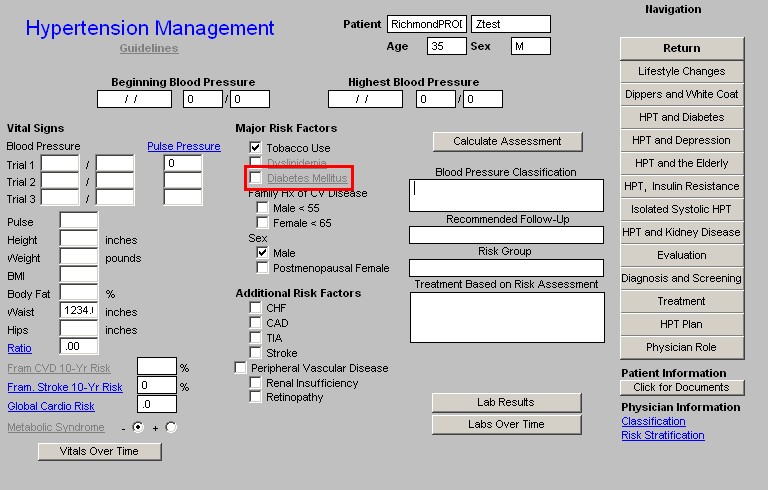
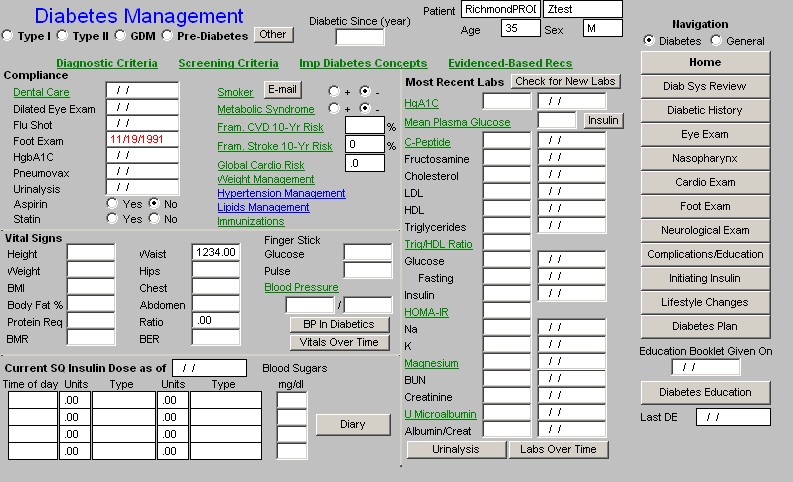
Depressing the Diabetes Mellitus Button launches the Diabetes Suite of Templates beginning with the Master Diabetes Management Template. For more information on the Master Diabetes Management Template, Click Here.
- Family History of CV Disease
- Male < 55
- Female < 65
- Sex
- Male
- Postmenopausal Female
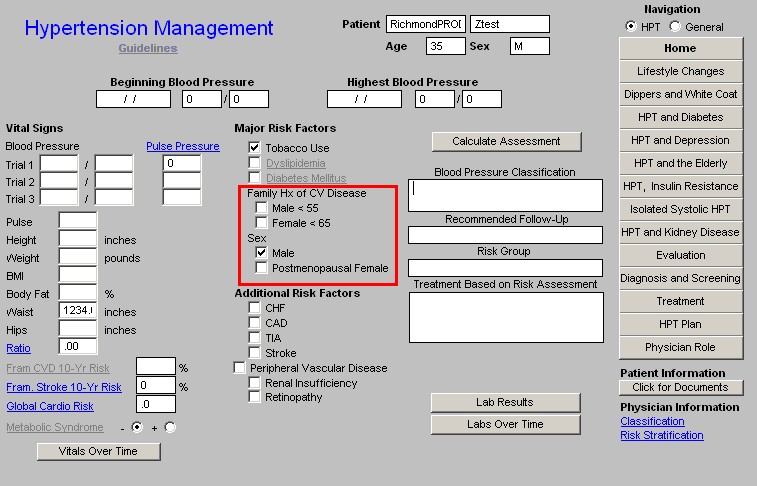
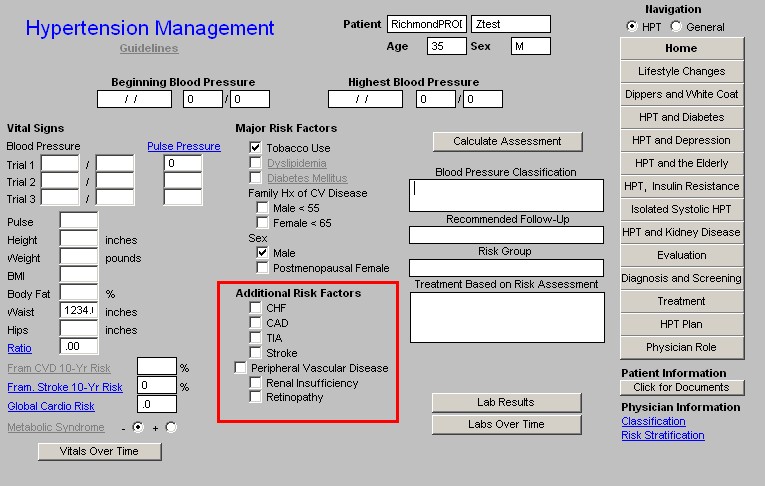
Additional Risk Factors -- The presence of any of these risk factors increases the cardiovascular risk burden carried by a patient and therefore increases the imperative for lowering the blood pressure.
- CHF
- CAD
- TIA
- Stroke
- Peripheral Vascular Disease
- Renal Insufficiency
- Retinopathy
Column 3 -
Calculate Assessment - when this button is depressed the following calculations are automatically made and displayed in the boxes named hypertension classification, recommended follow-up, risk group and treatment recommendation based on this risk assessment.
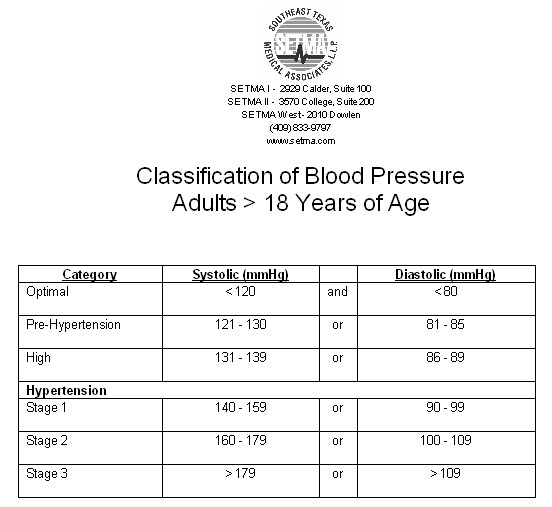
- Blood Pressure Classification - This indicate the risk associated with certain levels of blood pressure.
- Recommended Follow-up - This indicates how soon the patient should be seen for this blood pressure classification.
- Risk Group - This classification provides a risk stratification for determining the treatment of the patient. The Risk Group is determined by the factors listed in the document entitled "Risk Stratification" which is launched from the button of that name at the bottom right of this template.
- Treatment Based on Risk Assessment - Based on the Risk Group identified above, a treatment plan will be displayed. This will range from lifestyle modifications to drug therapy.
Note: For details see the Risk Stratification section below.
Lab Results - when this button is depressed, a pop-up is launched which has the following laboratory values displayed.
- Na
- K
- BUN
- Creatinine
- Ca
- Mg
- Ca/Mg - this ratio reflects the possible presence of a prothrombotic condition in a patient. Calcium promotes blood clotting, while Magnesium inhibits platelet aggregation. If the Ca/Mg ratio is above 5, the patient is likely to have a prothrombotic condition. This ratio is most often regulated by increasing the Magnesium level rather than decreasing the Calcium levels in the blood.
- Glucose
- Fasting Glucose
- Insulin
- HOMA-IR - Homeostasis Model Assessment of Insulin Resistance. This is a calculated value based on the fasting plasma glucose and the fasting insulin. The calculation is done automatically when these two values are present in NextGen's laboratory module. If this value is greater than 2, the patient is insulin resistant.
- MS Strip
- Microalbumin - as with diabetic nephropathy, so with hypertensive renal disease, urinary protein is the earliest indicator of renal damange.
- Uric Acid - increased uric acid is associated with a prothrombic state as well.
- Cholesterol
- HDL
- LDL
- Triglycerides
- Trig/HDL - if this ratio is over 2, the patient is probably insulin resistant.
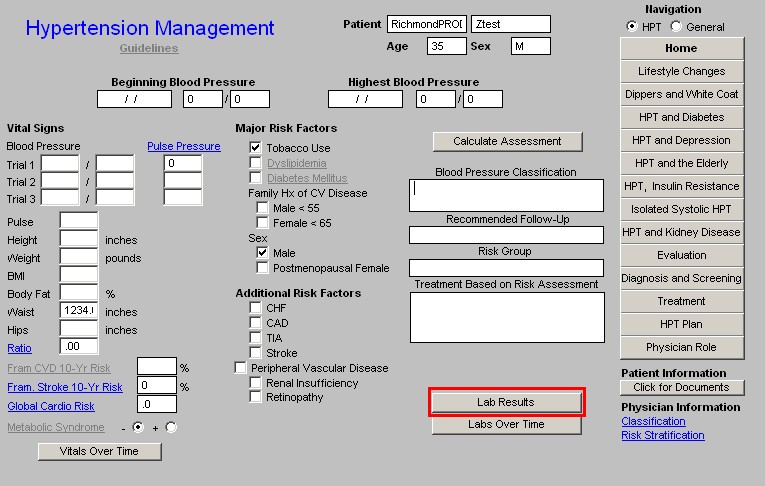
Labs Over Time - when this button is depressed, the "Hypertension Labs Over Time" template is launched.
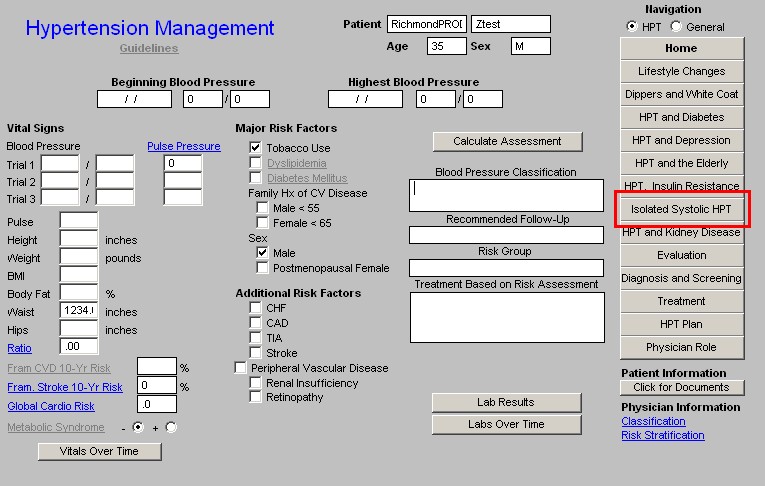
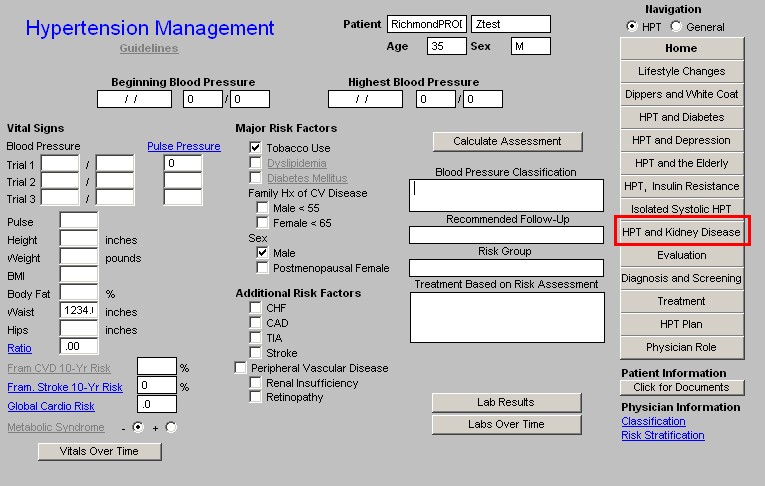
Column 4 -
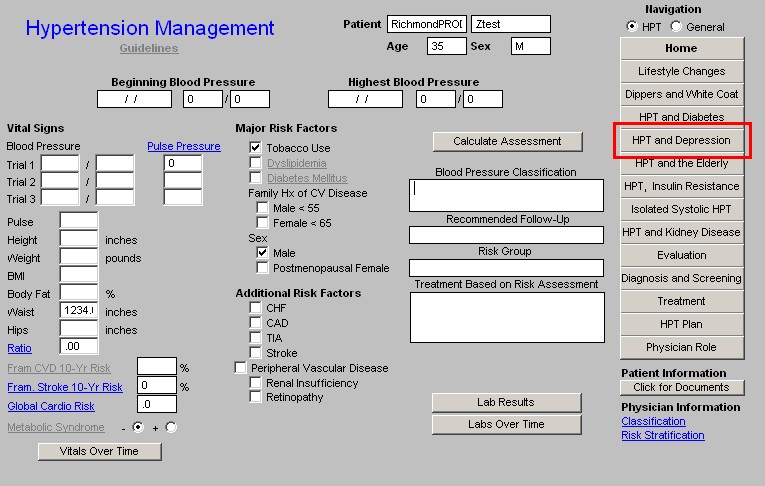
Navigation Buttons - there are two lists of navigation buttons which are displayed depending upon which of two boxes are checked:
Below are listed the templates which are displayed when each is checked in turn:
HPT - if this box is checked the templates which are specific to the disease management of the patient with hypertension are displayed:
- Home
- Lifestyle Changes
- Dippers and White Coat
- HPT and Diabetes
- HPT and Depression
- HPT and the Elderly
- HPT, Insulin Resistance
- Isolated Systolic HPT
- HPT and Kidney Disease
- Evaluation
- Diagnosis and Screening
- Treatment
- HPT Plan
- Physician Role
General - if this box is checked the templates which are drawn from the Master GP Suite of templates are displayed. Their use with the Hypertension Suite allows a patient's entire encounter to be documented from this suite, if no other issues are being addressed in this encounter.
- Return
- Chief/Chronic
- HPI
- Histories
- System Review
- Physical Exam
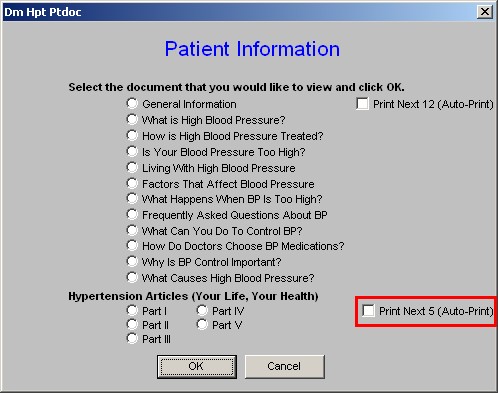
Beneath the navigation buttons are several patient information documents. When the button entitled "click for documents" is depressed the following list of documents appears.
The first twelve can be printed as a group and the last five can be printed as a group or they can be printed one at a time by following the instructions given.
- General Information
- What is High Blood Pressure?
- How is High Blood Pressure Treated?
- Is Your Blood Pressure too High?
- Living with High Blood Pressure
- Factors That Affect Blood Pressure
- What Happens When BP is Too High?
- Frequently Asked Questions About BP
- What Can You Do to Control BP?
- How Do Doctors Choose BP Medications?
- Why is BP Control Important?
- What Causes High Blood Pressure
The function entitled "Print Next 12 (auto-print)" prints the above 12 documents
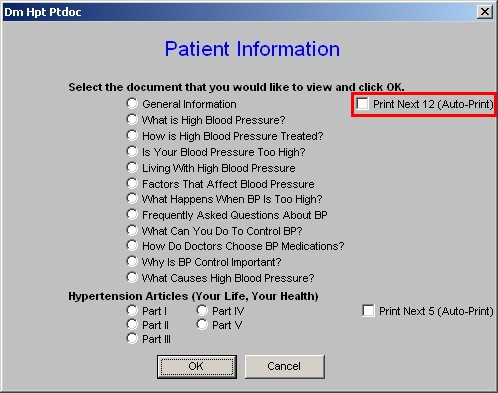
Hypertension Articles (Your Life, Your Health)
- Part 1
- Part II
- Part III
- Part IV
- Part V
The function entitled "Print Next 5 (auto print)" prints these five articles.
Physician Information - This is beneath the Patient Information function described above.
- Classification - this displays a table with the blood pressure classifications which are automatically calculated as described above.
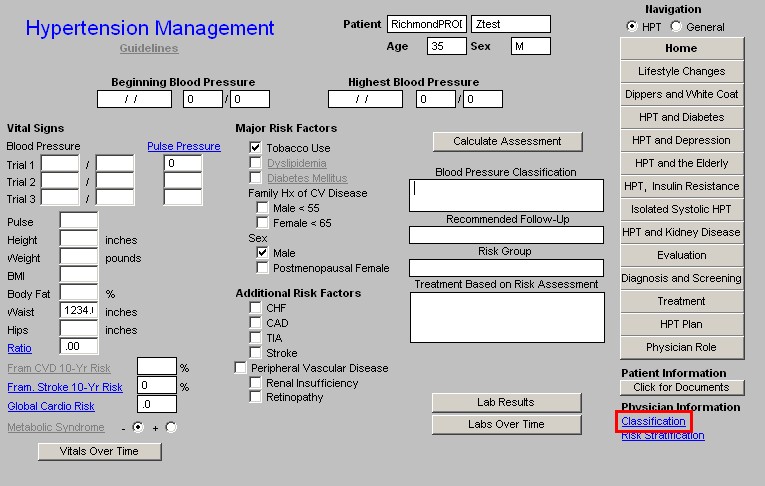
- Risk Stratification - this launches a document with a table which shows the calculation of the Risk Categories. In addition the following information is given:
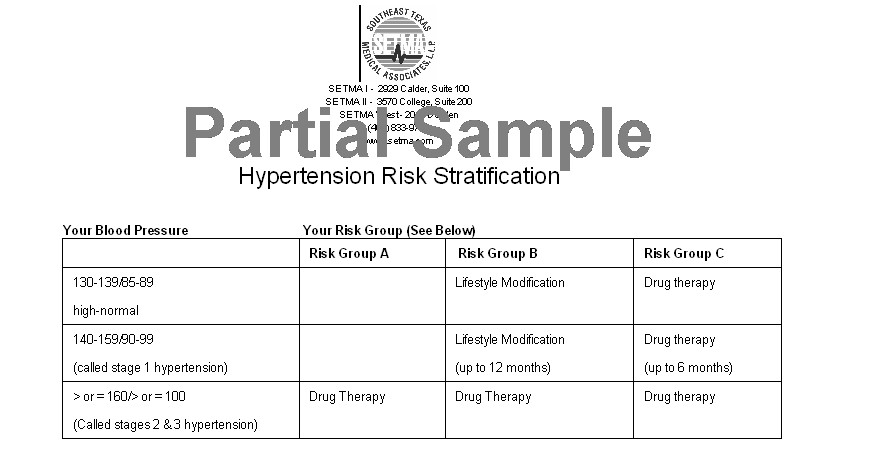
- Risk Group A
- No Risk Factors
- No Target Organ Damage
- No clinical cardiovascular disease
- Risk Group B
- At least 1 risk factor, not including Diabetes
- No target organ damage
- No clinical cardiovascular disease
- Risk Group C
- Target organ damage/clinical cardiovascular disease and/or Diabetes
- Other Risk Factors
- Risk Factors
- Tobacco use
- Dyslipidemia,
- Diabetes Mellitus,
- Sex (male and postmenopausal women),
- Family history of cardiovascular disease
- Target Organ Damage -
- LVH,
- CHF,
- CAD,
- Stroke,
- TIA,
- Peripheral Vascular Disease,
- Renal Insufficiency,
- Retinopathy
Lifestyle Changes Template
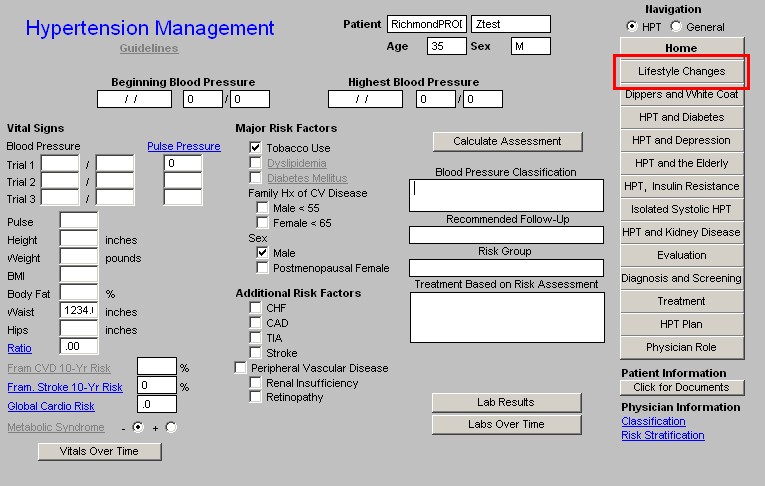
Lifestyle changes are the foundation of the treatment of virtually any chronic disease. On this template there are 12 Recommended Actions for the control and improvement of hypertension through lifestyle changes. The following describes how this template works.
- The 12 Recommended Actions are auto checked as they apply to anyone with hypertension or pre-hypertension.
- When this template is accessed, these recommended actions will appear on the Hypertension Follow-up Note which should be given to the patient each time they are treated or assessed for hypertension.
- The material described below on a Low Sodium Diet and the DASH Diet also automatically print with the Hypertension Follow-up Note.
- Those actions which have a proven effect on hypertension have a notation concerning the degree of improvement in systolic blood pressure which can be reasonably expected from that lifestyle action.
- The Blood Pressure reductions which can reasonably be expected from the 12 Recommended actions are:
- A 2-4 mmHg lowering from decreasing or eliminating alcohol use.
- A 5-20 mmHg lowering for every 20 pounds of weight loss.
- A 4-9 mmHg lowering from exercise
- A 2-8 mmHg lowering from a reduced salt intake
- A 8-14 mmHg lowering from following the DASH diet.
Contrast this with the fact that a single medication will generally provide a maximum of a 10 mmHg lowering of the systolic pressure.
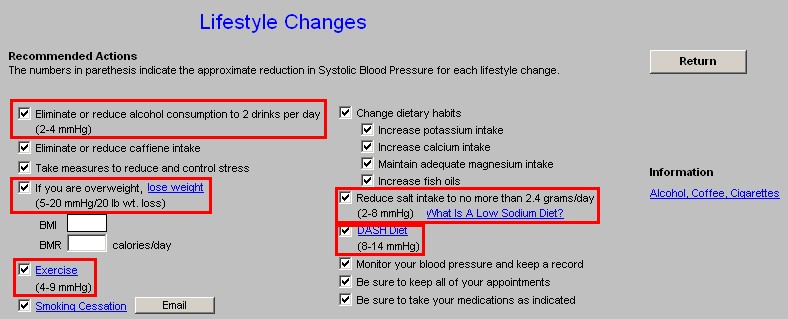
- The 12 Recommended Actions are:
- Eliminate or reduce alcohol consumption to 1 drink a day (2 - 4 mmHg)
- Eliminate or reduce caffeine intake.
- Take measures to reduce and control stress.
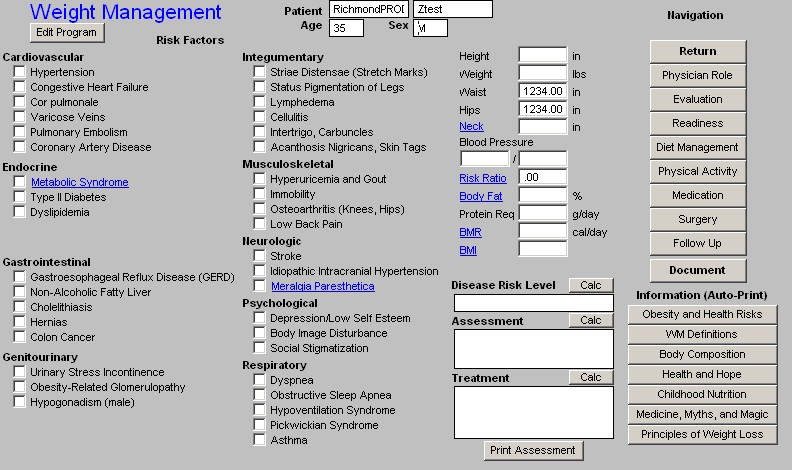
- If you are overweight, lose weight (5-20 mmHg/20 lb. wt. loss) -- there is also a hyperlink to SETMA's Weight Management Suite of Templates. And, there are boxes where the patient's BMI and BMR are automatically displayed.
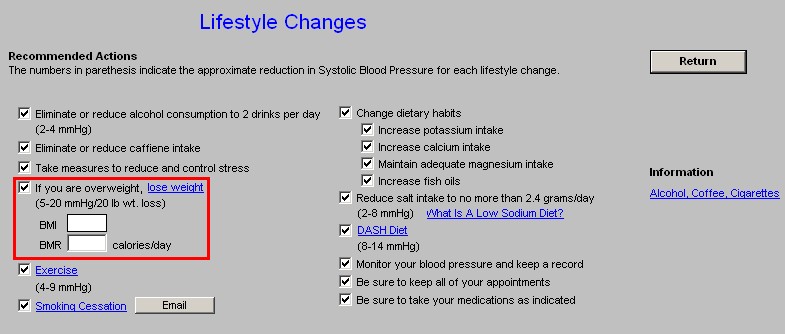
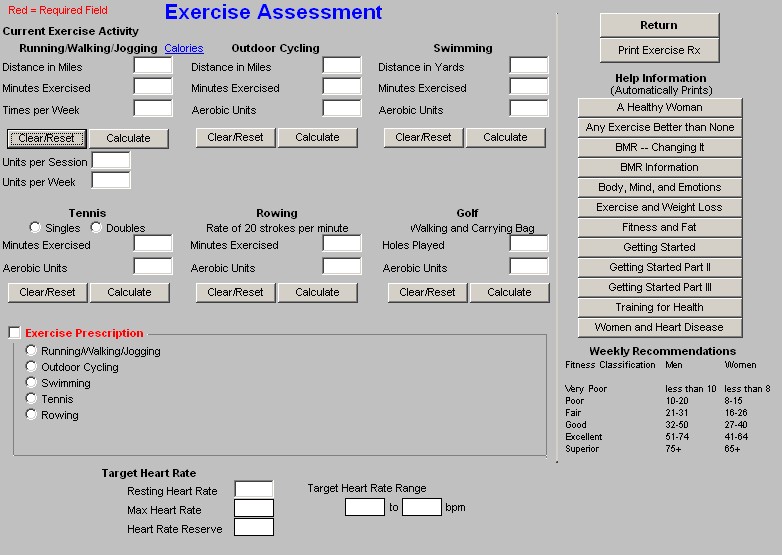
- Exercise (4-9 mmHg) - there is also a hyperlink to SETMA's Exercise template. For more information on the Exercise Prescription template, Click Here
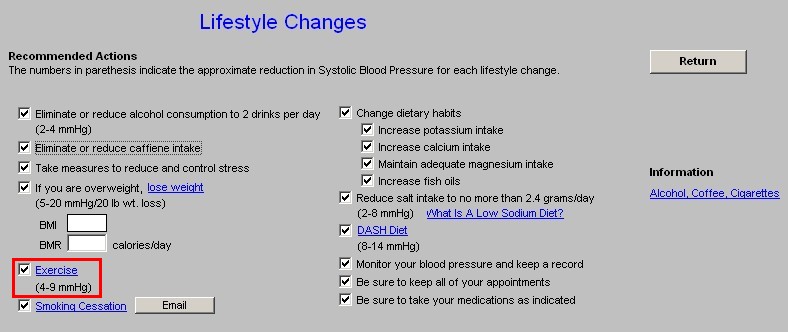
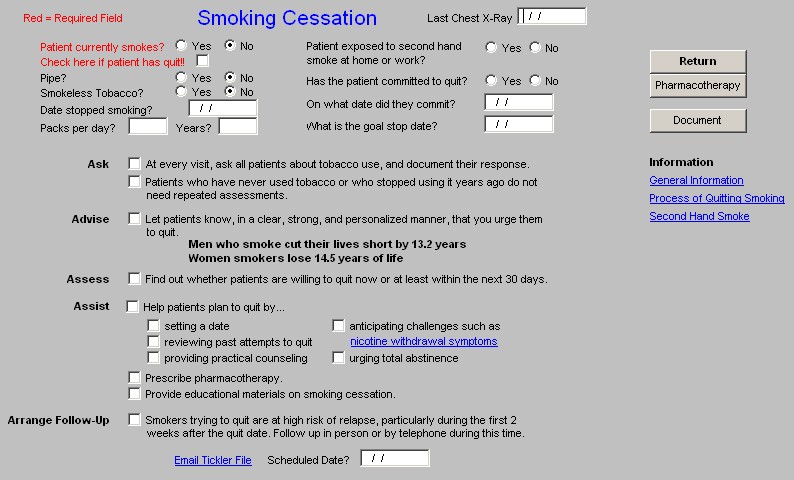
- Smoking Cessation - there is also a hyperlink to SETMA's Smoking Cessation Template and a button which launches an email for the creation of an electronic tickler file.
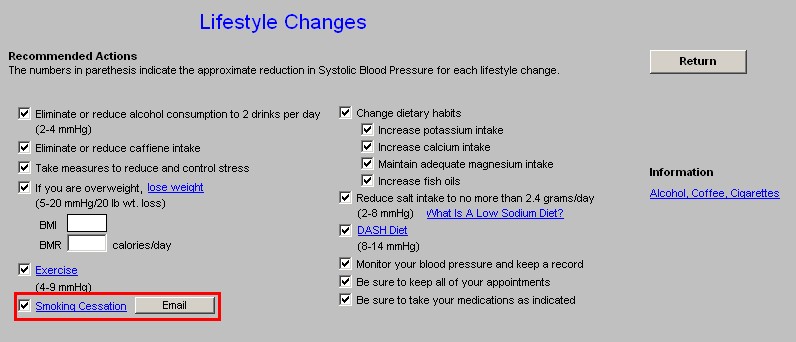
- Change Dietary habits
- Increase potassium intake
- Increase calcium intake
- Maintain adequate magnesium intake
- Increase fish oils
- Reduce Salt intake to no more than 2.4 grams/day (2-8 mmHg) - there is also a printable document entitled What is a low Sodium Diet?
- DASH Diet (8-14 mmHg) - there is also a hyperlink which prints an introduction to the DASH Diet - Dietary Approach to Stop Hypertension.
- Monitor your blood pressure and keep a record
- Be sure to keep all appointments
- Be sure to take your medications as indicated.
Information
A patient information document is launched and printed from this template entitled, "Alcohol, Coffee, Cigarettes."
Dippers and White Coat Syndrome Template
The concepts of "dipping," "non-dipping," and "white coat syndrome" are very important to the proper evaluation and treatment of hypertension. The frequent reviewing of the information on this template will help keep these principles in mind as patients are evaluated for decreasing their stroke risk.
There are four pop-ups on this template.
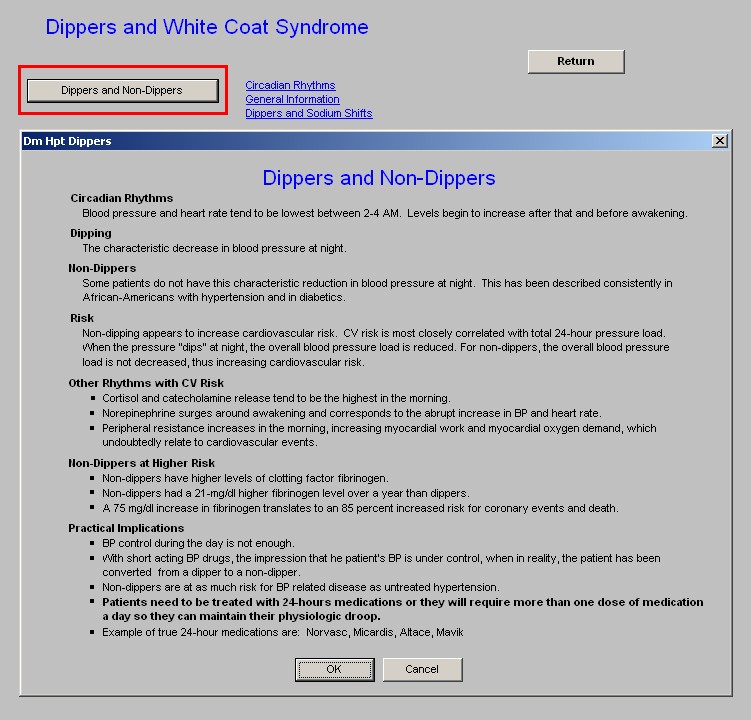
- Dippers and Non-Dippers - this addresses the very important physiological decreasing of blood pressure in the early morning hours. There three educational documents associated with this phenomenon: Circadian Rhythms, General Information, Dippers and Sodium Shifts. The pop-up displays the following information:
- Circadian Rhythms -- Blood pressure and heart rate tend to be lowest between 2-4 AM. Levels begin to increase after that and before awakening.
- Dipping -- The characteristic decrease in blood pressure at night.
- Non-Dippers -- Some patients do not have this characteristic reduction in blood pressure at night. This has been described consistently in African-Americans with hypertension and in diabetics.
- Risk
- Non-dipping appears to increase cardiovascular risk.
- CV risk is most closely correlated with total 24-hour pressure load.
- When the pressure "dips" at night, the overall blood pressure load is reduced.
- For non-dippers, the overall blood pressure load is not decreased, thus increasing cardiovascular risk.
- Other Rhythms with CV Risk
- Cortisol and catecholamine release tend to be the highest in the morning.
- Norepinephrine surges around awakening and corresponds to the abrupt increase in BP and heart rate.
- Peripheral resistance increases in the morning, increasing myocardial work and myocardial oxygen demand, which undoubtedly relate to cardiovascular events.
- Non-Dippers at Higher Risk
- Non-dippers have higher levels of clotting factor fibrinogen.
- Non-dippers had a 21-mg/dl higher fibrinogen level over a year than dippers.
- A 75 mg/dl increase in fibrinogen translates to an 85 percent increased risk for coronary events and death.
- Practical Implications
- BP control during the day is not enough.
- With short acting BP drugs, the impression that he patient's BP is under control, when in reality, the patient has been converted from a dipper to a non-dipper.
- Non-dippers are at as much risk for BP related disease as untreated hypertension.
- Patients need to be treated with 24-hours medications or they will require more than one dose of medication a day so they can maintain their physiologic droop.
- Example of true 24-hour medications are: Norvasc, Micardis, Altace, Mavik
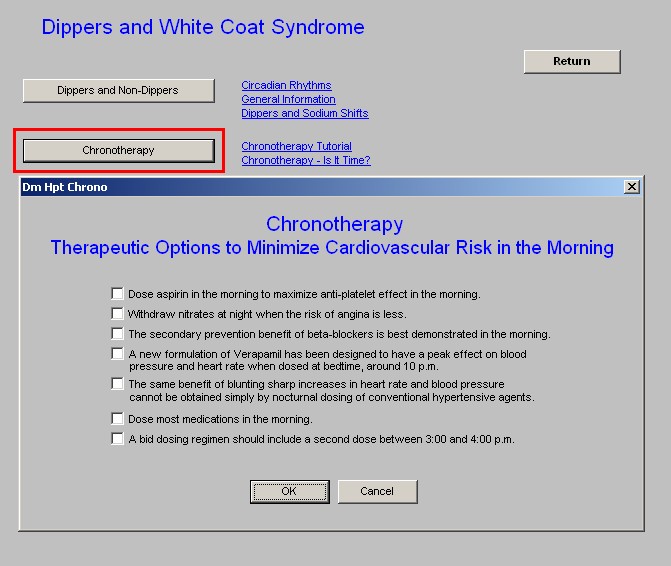
- Chronotherapy - the subtitle of this pop-up is "Therapeutic Options to Minimize Cardiovascular Risk." The seven facts about the "timing" of medication administration to improve its beneficial effects is an introduction to the large field of chronotherapy. This pop-up has two documents associated with it: Chronotherapy: A Tutorial and Chronotherapy: Is it Time?
- Chronotherapy
- Therapeutic Options to Minimize Cardiovascular Risk in the Morning
- Dose aspirin in the morning to maximize anti-platelet effect in the morning.
- Withdraw nitrates at night when the risk of angina is less.
- The secondary prevention benefit of beta-blockers is best demonstrated in the morning.
- A new formulation of Verapamil has been designed to have a peak effect on blood pressure and heart rate when dosed at bedtime, around 10 p.m.
- The same benefit of blunting sharp increases in heart rate and blood pressure cannot be obtained simply by nocturnal dosing of conventional hypertensive agents.
- Dose most medications in the morning.
- A bid dosing regimen should include a second dose between 3:00 and 4:00 p.m.
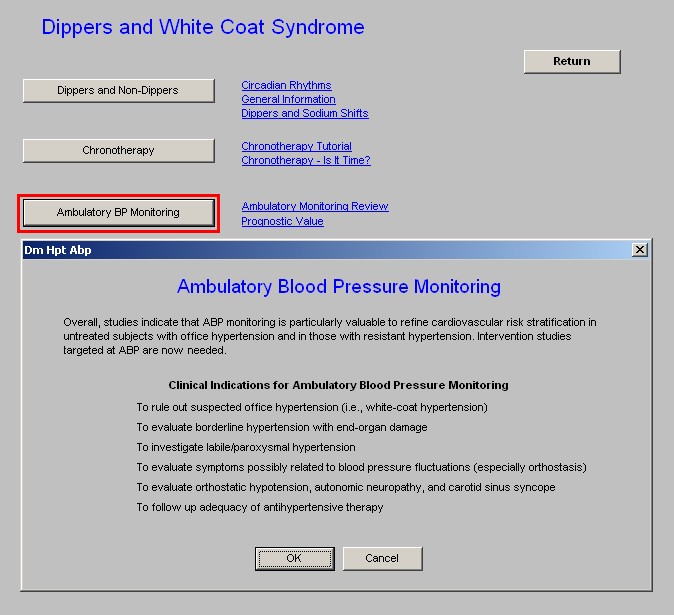
- Ambulatory BP Monitoring - the following information appears on this pop-up. Two documents are associated with this pop-up: Ambulatory Monitoring Review and Prognostic Value.
Overall, studies indicate that ABP monitoring is particularly valuable to refine cardiovascular risk stratification in untreated subjects with office hypertension and in those with resistant hypertension. Intervention studies targeted at ABP are now needed.
- Clinical Indications for Ambulatory Blood Pressure Monitoring
- To rule out suspected office hypertension (i.e., white-coat hypertension)
- To evaluate borderline hypertension with end-organ damage
- To investigate labile/paroxysmal hypertension
- To evaluate symptoms possibly related to blood pressure fluctuations (especially orthostasis)
- To evaluate orthostatic hypotension, autonomic neuropathy, and carotid sinus syncope
- To follow up adequacy of antihypertensive therapy
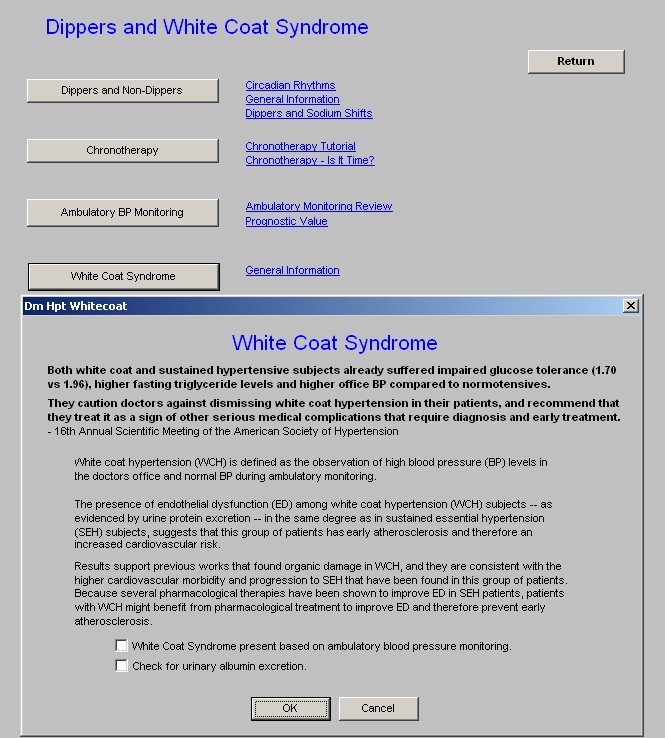
- White Coat Syndrome - the following information appears on this pop-up which is associated with a document entitled, General Information. Healthcare providers are cautioned about dismissing patients with "white coat syndrome" as it increases cardiovascular risk.
- Both white coat and sustained hypertensive subjects already suffered impaired glucose tolerance (1.70 vs 1.96), higher fasting triglyceride levels and higher office BP compared to normotensives.
- They caution doctors against dismissing white coat hypertension in their patients, and recommend that they treat it as a sign of other serious medical complications that require diagnosis and early treatment.
- 16th Annual Scientific Meeting of the American Society of Hypertension
- White coat hypertension (WCH) is defined as the observation of high blood pressure (BP) levels in the doctors office and normal BP during ambulatory monitoring.
- The presence of endothelial dysfunction (ED) among white coat hypertension (WCH) subjects -- as evidenced by urine protein excretion -- in the same degree as in sustained essential hypertension (SEH) subjects, suggests that this group of patients has early atherosclerosis and therefore increased cardiovascular risk.
- Results support previous works that found organic damage in WCH, and they are consistent with the higher cardiovascular morbidity and progression to SEH that have been found in this group of patients. Because several pharmacological therapies have been shown to improve ED in SEH patients, patients with WCH might benefit from pharmacological treatment to improve ED and therefore prevent early atherosclerosis.
The following two are check boxes for further evaluation of the patient with suspicion of WCS:
- White Coat Syndrome present based on ambulatory blood pressure monitoring.
- Check for urinary albumin excretion.
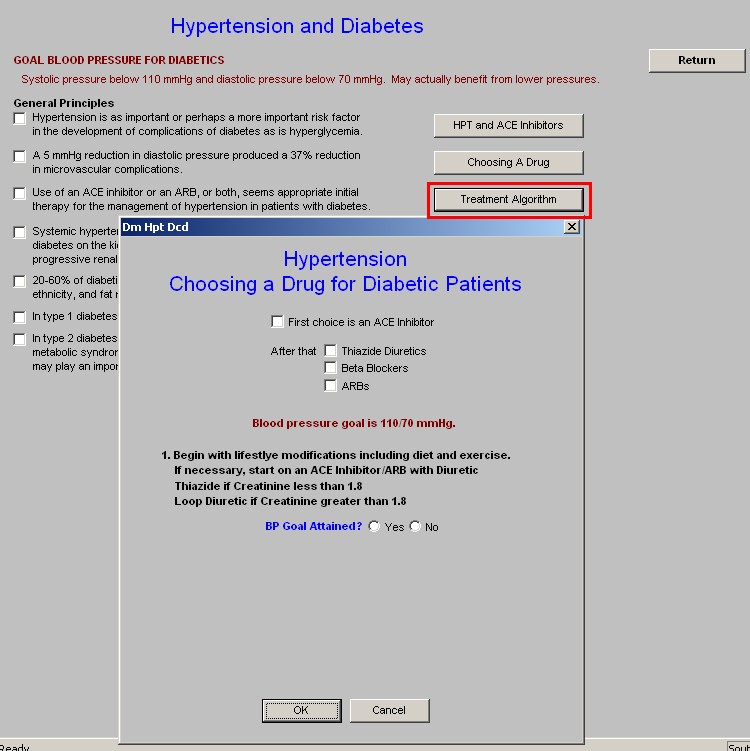
Hypertension and Diabetes Template
This template addresses the goals and principles of the treatment of hypertension in the patient with diabetes. Its review and the knowledge and use of the algorithms contained in it are key to the successful treatment of hypertension in the patient with diabetes.
When the Navigation button entitled HPT and Diabetes is depressed the following template is launched.
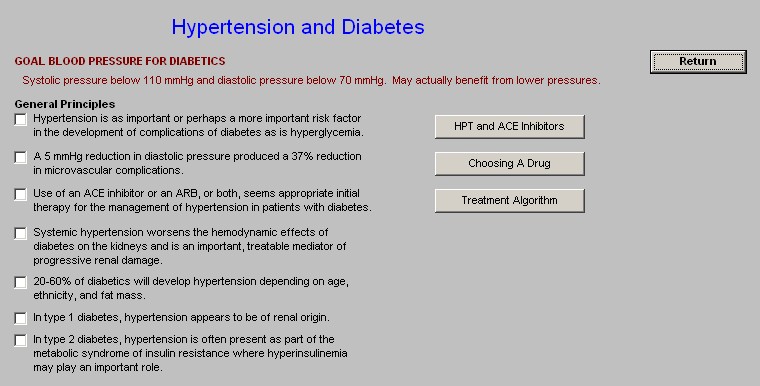
- Goal - 110/70 mm Hg
- General Principles
- Hypertension is as important or perhaps a more important risk factor in the development of complications of diabetes as is hyperglycemia.
- A 5 mmHg reduction in diastolic pressure produced a 37% reduction in microvascular complications.
- Use of an ACE inhibitor or ARB, or both, seems appropriate initial therapy for the management of hypertension in patients with diabetes.
- Systemic hypertension worsens the hemodynamic effects of diabetes on the kidneys and is an important, treatable mediator of progressive renal damage.
- 20-60% of diabetics will develop hypertension depending on age, ethnicity, and fat mass.
- In type 1 diabetes, hypertension appears to be of renal origin.
- In type 2 diabetes, hypertension is often present as part of the metabolic syndrome of insulin resistance where hyperinsulinemia may play an important role.
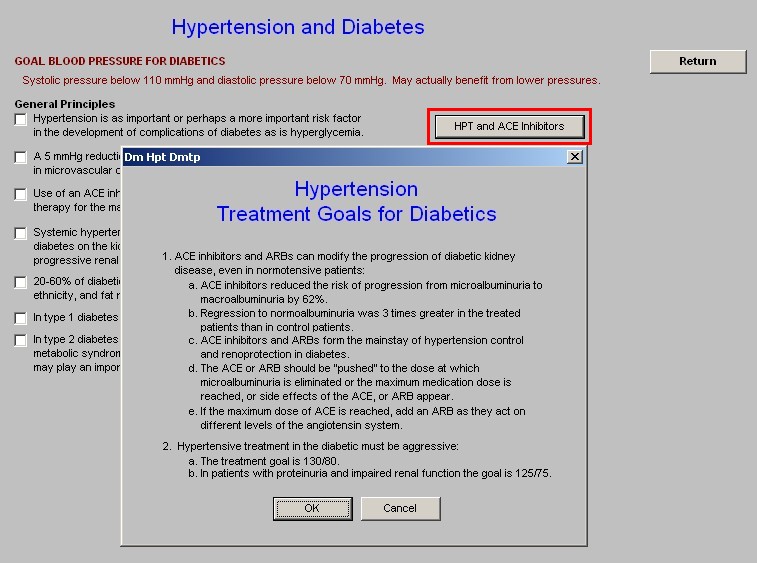
Three pop-ups appear on this template; they are:
- HPT and Ace Inhibitors - this pop-up displays the following information
Treatment Goals for Diabetics
- ACE inhibitors and ARBs can modify the progression of diabetic kidney disease, even in normotensive patients:
- ACE inhibitors reduced the risk of progression from microalbuminuria to macroalbuminuria by 62%.
- Regression to normoalbuminuria was 3 times greater in the treated patients than in control patients.
- ACE inhibitors and ARBs form the mainstay of hypertension control and renoprotection in diabetes.
- The ACE or ARB should be "pushed" to the dose at which microalbuminuria is eliminated or the maximum medication dose is reached, or side effects of the ACE, or ARB appear.
- If the maximum dose of ACE is reached, add an ARB as they act on different levels of the angiotensin system.
- Hypertensive treatment in the diabetic must be aggressive:
- The treatment goal is 130/80.
- In patients with proteinuria and impaired renal function the goal is 125/75.
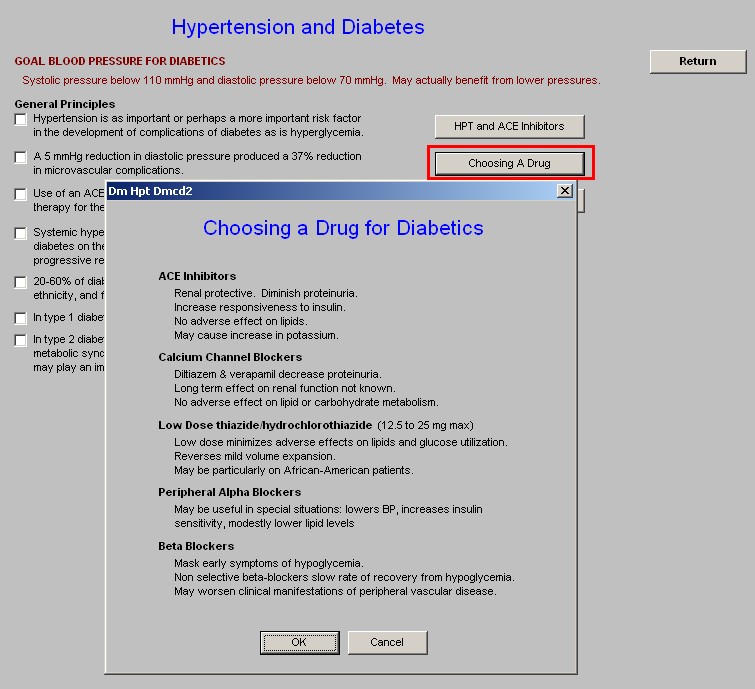
- Choosing a Drug - this pop-up displays the following information on five classes of antihypertensive medications:
- ACE Inhibitors
- Renal protective. Diminish proteinuria.
- Increase responsiveness to insulin.
- No adverse effect on lipids.
- May cause increase in potassium.
- Calcium Channel Blockers
- Diltiazem & verapamil decrease proteinuria.
- Long term effect on renal function not known.
- No adverse effect on lipid or carbohydrate metabolism.
- Low Dose thiazide/hydrochlorothiazide (12.5 to 25 mg max)
- Low dose minimizes adverse effects on lipids and glucose utilization.
- Reverses mild volume expansion.
- May be particularly on African-American patients.
- Peripheral Alpha Blockers
May be useful in special situations: lowers BP, increases insulin sensitivity, modestly lower lipid levels
- Beta Blockers
- Mask early symptoms of hypoglycemia.
- Non selective beta-blockers slow rate of recovery from Hypoglycemia.
- May worsen clinical manifestations of peripheral vascular disease.
- Treatment Algorithm - this pop-up displays information, "Hypertension: Choosing A Drug for Diabetic Patients."
- First Choice is an ACE-Inhibitor - there is a check box for selecting that option.
- After that
Thiazide Diuretics - there is a check box
Beta Blockers - there is a check box
ARBs - there is a check box
NOTE: Blood Pressure goal is 110/70 mmHg.
- Steps of treatment of hypertension in patients with diabetes
- Begin with lifestyle modifications including diet and exercise
- If necessary, start on an ACE Inhibitor/ARB with Diuretic
Thiazide if Creatinine less than 1.8
Loop Diuretic if Creatinine greater than 1.8
- BP Goal Attained? Yes? Stop; No? Proceed
- Add a long-acting nondihydrophyridine Calcium Channel Blocker such as Amlodipine or Norvasc
- BP Goal Attained? Yes? Stop; No? Proceed
- What is the patient's resting pulse? If above 84 -
- Add a Beta Blocker; if BP goal still not attained, refer to a hypertension specialist.
What is the patient's resting pulse? If below 84 -
- Add another subgroup of Calcium Channel Blockers. If BP still not attained, refer to a hypertension specialist.
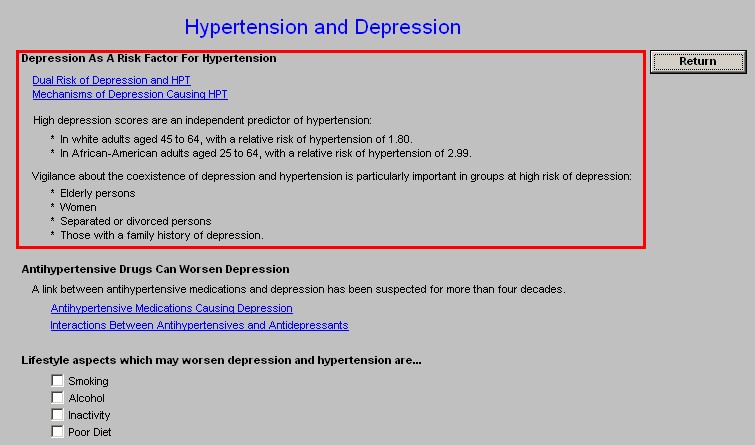
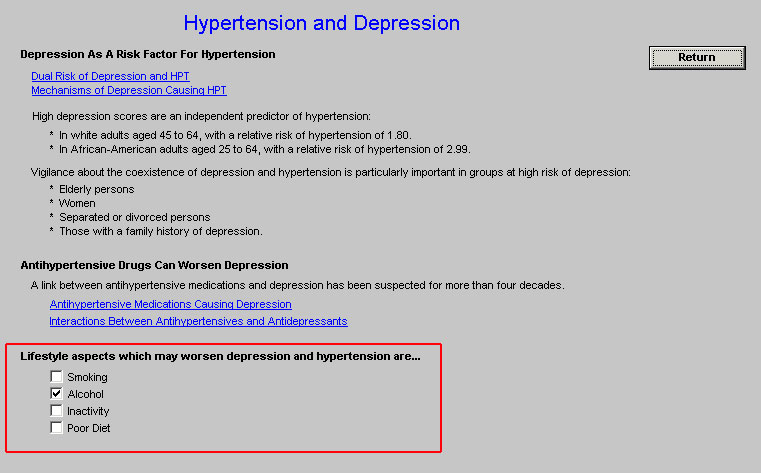
Hypertension and Depression Template
This template addresses the relationship between both conditions and between the impact which the treatment of one can have on the other. The treatment of hypertension in the elderly is often complicated by the presence of depression particularly since the medications for both conditions often interact with one another.
There are three sections to the information on this template:
- Depression As A Risk Factor for Hypertension
- Dual Risk of Depression and HPT
- Mechanisms of Depression Causing HPT
High depression scores are an independent predictor of hypertension
- Vigilance about the coexistence of depression and hypertension is particularly important in:
- Elderly patients
- Women
- Separate or divorced persons
- Those with a family history of depression
- Antihypertensive Drugs Can Worsen Depression
- A link between antihypertensive medications and depression has been suspected for more than four decades.
- Antihypertensive Medications Causing Depression
- Interactions Between Antihypertensives and Antidepressants
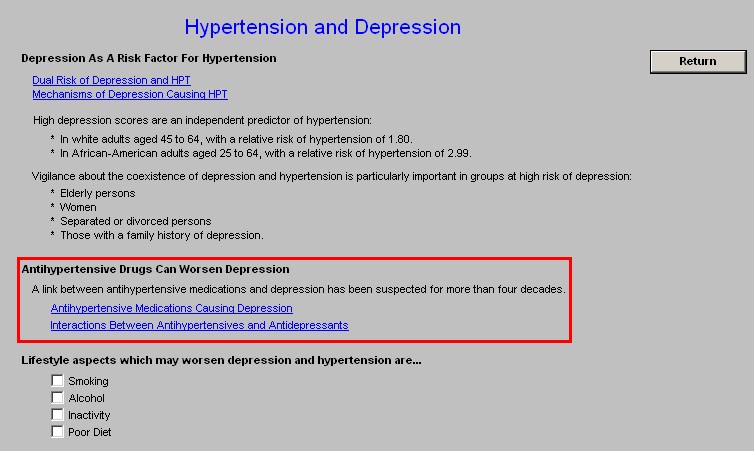
- Lifestyle Aspects Which May Worsen Depression and Hypertension
- Smoking
- Alcohol
- Inactivity
- Poor Diet
Hypertension and the Elderly Template
Blood pressure is a significant problem in the elderly, particularly when you realized that if you are 55 years of age and do not have hypertension, your lifetime risk of developing hypertension is 90%.. Controlling blood pressure, and particularly systolic blood pressure in the elderly, even those beyond 80 will decrease morbidity and mortality for cerebrovascular accidents and myocardial infarctions.
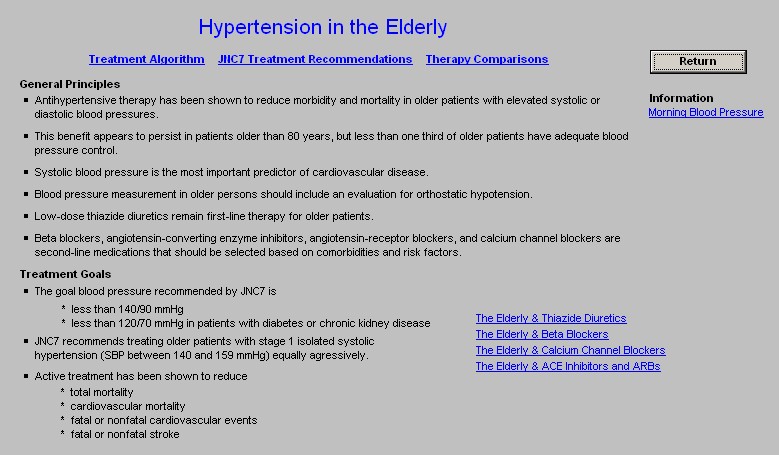
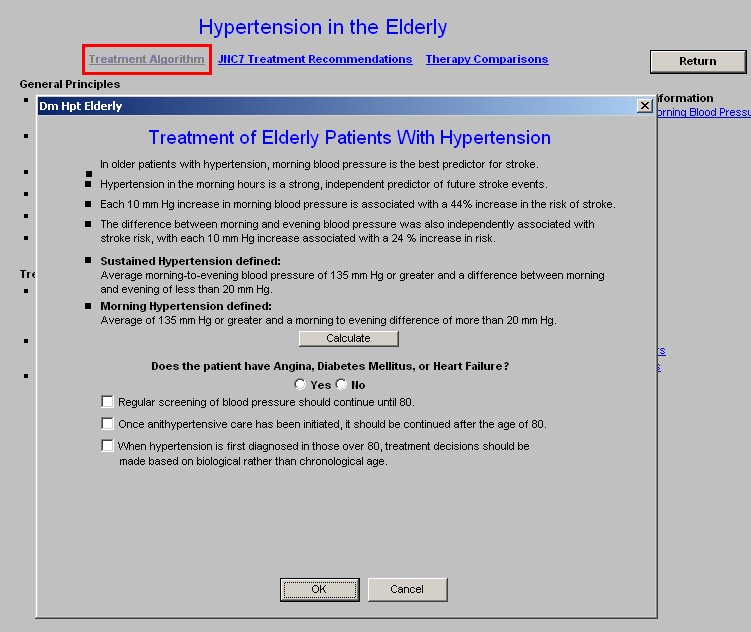
There are three pop-ups at the top of this template; they are:
- Treatment Algorithm - this pop-up displays the following information
Treatment of Elderly Patients with Hypertension
- In older patients with hypertension, morning blood pressure is the best predictor for stroke.
- Hypertension in the morning hours is a strong, independent predictor of future stroke events.
- Each 10 mm Hg increase in morning blood pressure is associated with a 44% increase in th risk of stroke.
- The difference between morning and evening blood pressure was also independently associated with stroke risk, with each 10 mm Hg increase associated with a 24$ increase in risk.
- Sustained Hypertension defined: -- Average morning-to-evening blood pressure of 135 mm Hg or greater and a difference between morning and evening of less than 20 mm Hg
- Morning Hypertension defined:-- Average of 135 mm Hg or greater and a morning to evening difference of more than 20 mm Hg. At this point on the Treatment of Elderly Patients with Hypertension algorithm there appears a button entitled Calculate.
- When depressed the Calculate button launches a pop-up with the following title Sustained vs. Morning Hypertension
- Enter the patient's average morning and evening blood pressure and lcikc calculate.
- In the box present the conclusion of morning or sustained blood pressure will appear.
A question is then asked: "Does the patient have angina, diabetes mellitus, or heart failure?" Yes/No
- Check boxes are then provided to guide the following:
- Regular screening of blood pressure should continue until 80.
- Once antihypertensive care has been initiated, it should be continued after the age of 80.
- When hypertension is first diagnoses in those over 80, treatment decisions should be made based on biological rather than chronological age.
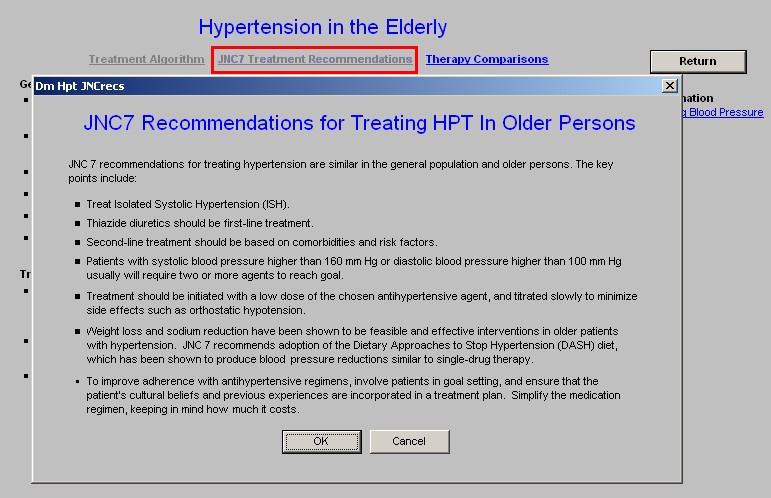
- JNC7 Treatment Recommendations - this pop-up displays the following principles of the treatment of hypertension in the elderly:
Note: JNC 7 recommendations for treating hypertension are similar in the general population and older persons. The key points include:
- Treat isolated systolic hypertension
- Thiazide diuretics should be first-line treatment.
- Second-line treatment should be based on comorbidites and risk factors.
- Patients with systolic blood pressure higher than 160 mm Hg or diastolic blood pressure higher than 100 mm Hg usually will require two or more agents to reach goal.
- Treatment should be initiated with a low dose of the hosen antihypertensive agent, and titrated slowly to minimize side effects such as orthostatic hypertension
- Weight loss and sodium reduction have been shown to be feasible and effective interventions in older patients with hypertension. JNC 7 recommends adoption fo the Dietary Approaches ot Stop Hypertension (DASH) diet, which has been show to produce blood pressure reductions similar to single-drug therapy.
- To improve adherence with antihypertensive regimens, involve patients in goal setting, and ensure that the patients' cultural beliefs and previous experiences are incorporated in a treatment plan. Simply the medication regimen, keeping in mind how much it costs.
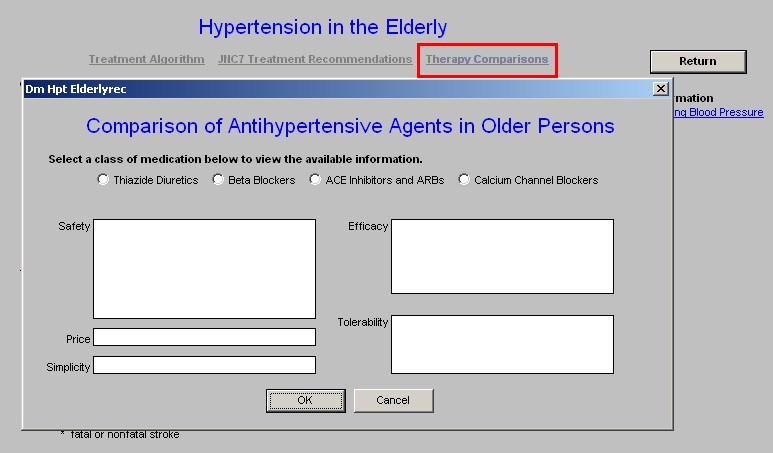
- Therapy Comparisons - this pop-up compares the safety, price and simplicity of use of four classes of medications in the elderly:
- Thiazide Diuretics,
- Beta Blockers,
- ACE Inhibitors and
- Calcium Channel Blockers.
The remainder of the template details General Principles and Goals of treatment in the elderly:
- General Principles:
- Antihypertensive therapy has shown to reduce morbidity and mortality older patients with elevated systolic and diastolic blood pressures
- This benefit appears to persist in patients older than 80 years, but less than one third of older patients have adequate pressure control.
- Systolic Blood pressure is the most important predictor of cardiovascular disease.
- Blood pressure measurement in older persons should include an evaluation for orthostatic hypotension.
- Low-dose thiazide diuretics remain first-line therapy for older patients
- Beta blockers, angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers and calcium channel blockers are second-line medications that should be selected based on comorbidities and risk factors.
- Treatment Goals
- The goal blood pressure recommended by JNC7 is:
- Less than 140/90 mmHg
- Less than 110/70 mmHg in patients with diabetes or chronic kidney disease.
- JNC 7 recommends treating older patents with stage 1 systolic hypertension (SBP between 140 and 150 mmHg) equally aggressively
- Active treatment has been shown to reduce
- Total mortality
- Cardiovascular mortality
- Fatal or nonfatal cardiovascular events
- Fatal or nonfatal stroke.
There is a series of four documents linked to this template; they are:
- The Elderly and Thiazide Diuretics
- The Elderly and Beta Blockers
- The Elderly and Calcium Channel Blockers
- The Elderly and Ace Inhibitors and ARBs
One last information document is launched from a link entitled, "Morning Blood Pressure." This document addresses the following concept "Early to Rise - Morning Blood Pressure Predicts Stroke."
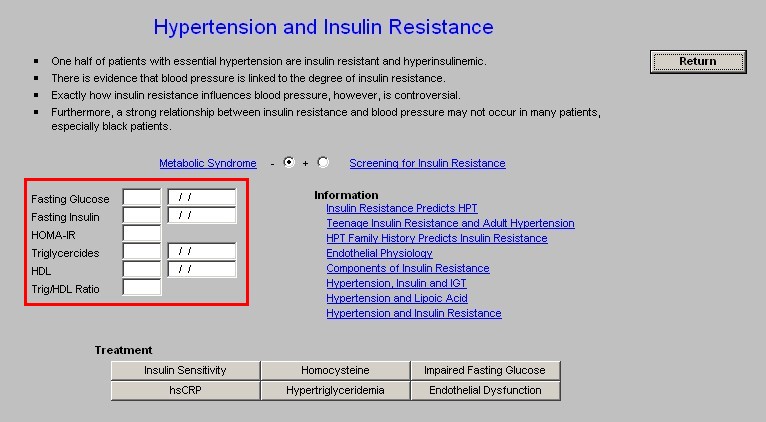
HPT, Insulin Resistance Template
In SETMA's Metabolic Syndrome Suite of Templates, on the Insulin Resistance Template, the following statements are made:
- Insulin resistance contributes to decreased renal function reserve and to the development of hypertension
- Insulin resistance is one of the causes of treatment-resistant essential hypertension
The medical literature is not unanimous in these conclusions at present but the association between insulin resistance and the other markers of the metabolic syndrome - obesity, dyslipidemia, hyperglycemia, renal damage as evidenced by microalbuminuria - all of which are both causes of and results of endothelium dysfunction, is strong. So much so, that in the face of treatment resistant hypertension, it is worthwhile to address the issue of insulin resistance and endothelium dysfunction.
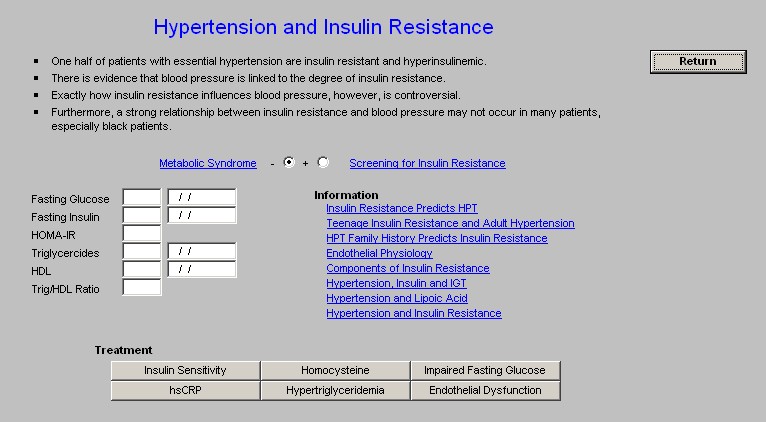
At the top of HPT, Insulin Resistance template are the following General Concepts:
- One half of patents with essential hypertension are insulin resistant and hyperinsulinemic.
- There is evidence that blood pressure is linked to the degree of insulin resistance.
- Exactly how insulin resistance influences blood pressure, however, is controversial.
- Furthermore, a strong relationship between insulin resistance and blood pressure may not occur in many patients, especially black patients.
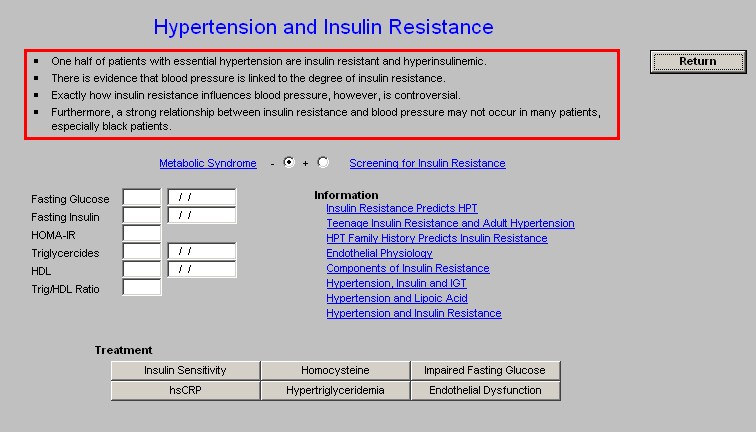
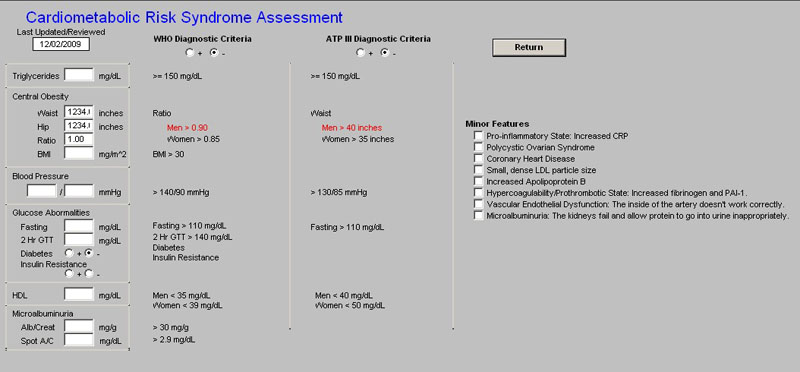
Beneath these principles is a link to the Metabolic Syndrome Assessment Template which results will populate the check boxes which display whether or not the patient has the metabolic syndrome.
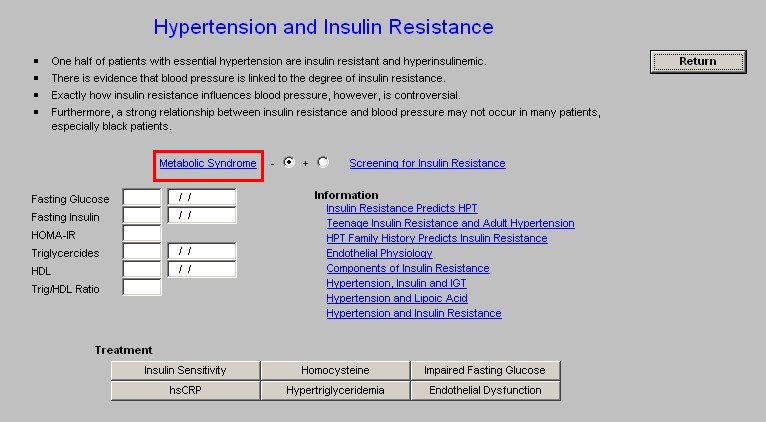
Next is a link to the Screening for Insulin Resistance template which is part of the Less Initiative.
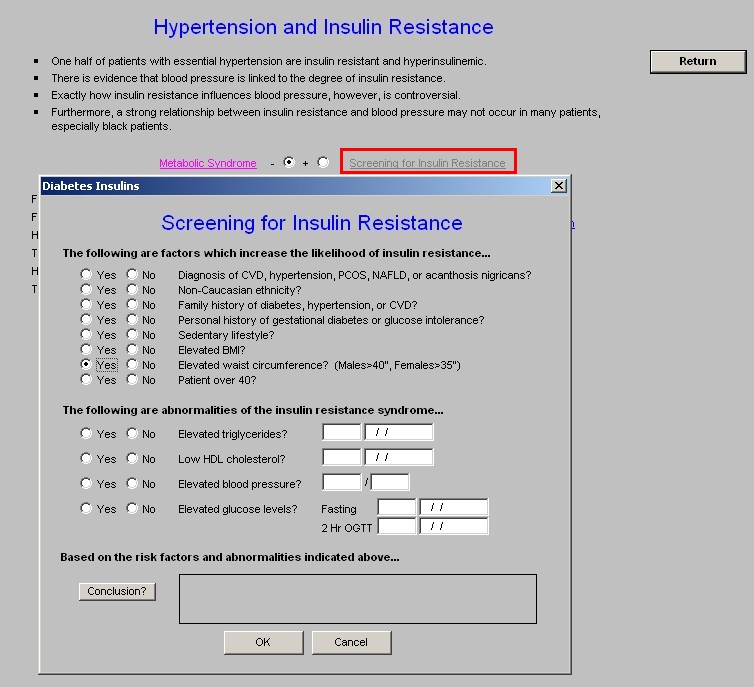
The elements of this template are automatically populated from the EMR data base. When the button entitled Conclusion? is depressed a summary of whether the patient is at risk for insulin resistance, and consequently the potential blood pressure problems associated with it, will appear.
The following laboratory values are then displayed:
- Fasting Glucose
- Fasting Insulin
- HOMA-IR - Homeostasis Model Assessment of Insulin Resistance. A value above 2 indicates insulin resistance.
- Triglycerides
- HDL
- Trig/HDL Ratio - a value above 2 for this ratio indicates Insulin Resistance.
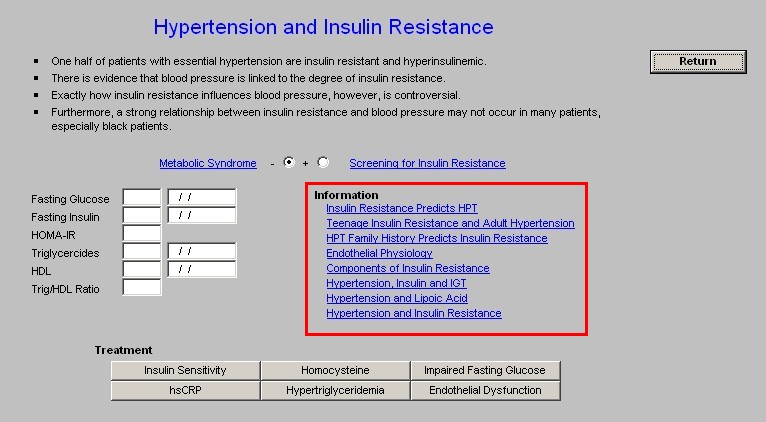
Beside the laboratory values are buttons which launch the following documents:
- Insulin Resistance Predicts HPT
- Teenage Insulin Resistance and Adult Hypertension
- HPT Family Hisory Predicts Insulin Resistance
- Endotehlial Physiology
- Components of Insulin Resistance
- Hypertension, Insulin and IGT
- Hypertension and Lipoic Acid
- Hypertension and Insulin Resistance
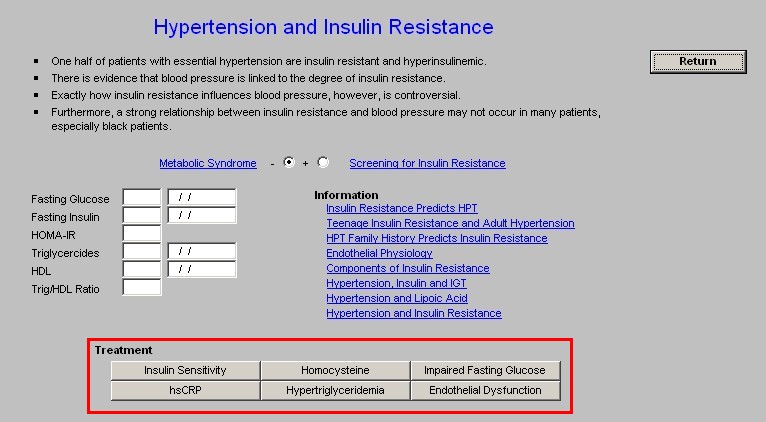
At the bottom of this template are six buttons which launch Treatment Recommendations for the following,( for details on these functions, which are self explanatory. see the tutorial for the Metabolic Syndrome Treatment Recommendations.):
- Insulin Sensitivity
- hsCRP
- Homocysteine
- Hypertriglyceridemia
- Impaired Fasting Glucose
- Endothelial Dysfunction
Isolated Systolic Hypertension Template
Perhaps the most under treated and damaging form of hypertension is Isolated Systolic Hypertension (ISH), particularly in the elderly. The key to ISH treatment is its recognition and diagnosis and the understanding of the increased cardiovascular and cerebrovascular risk associated with it.
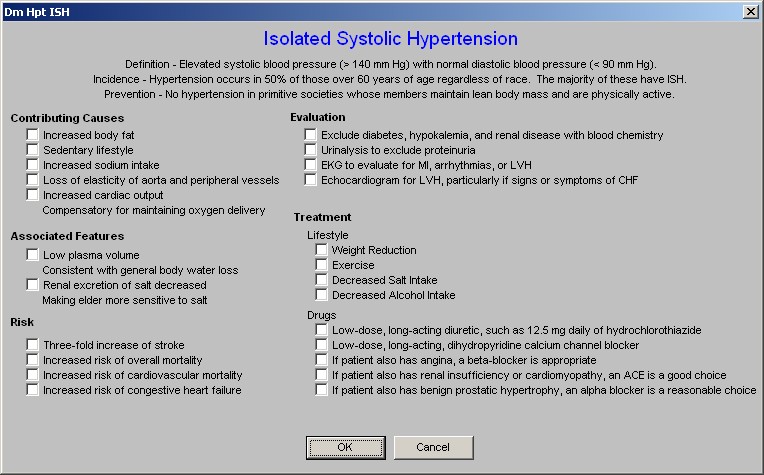
This template contains the following material:
- Definition - Elevated systolic blood pressure (> 140 mm Hg) with normal diastolic blood pressure (< 90 mm Hg).
- Incidence - Hypertension occurs in 50% of those over 60 years of age regardless of race. The majority of these have ISH.
- Prevention - No hypertension in primitive societies whose members maintain lean body mass and are physically active.
- Contributing Causes
- Increased body fat
- Sedentary lifestyle
- Increased sodium intake
- Loss of elasticity of aorta and peripheral vessels compensatory for maintaining oxygen delivery
- Associated Features
- Low plasma volume consistent with general body water loss
- Renal excretion of salt decreased making elder more sensitive to salt
- Risk
- Three-fold increase of stroke
- Increased risk of overall mortality
- Increased risk of cardiovascular mortality
- Increased risk of congestive heart failure
- Evaluation
- Exclude diabetes, hypokalemia, and renal disease with blood chemistry
- Urinalysis to exclude proteinuria
- EKG to evaluate for MI, arrhythmias, or LVH
- Echocardiogram for LVH, particularly if signs or symptoms of CHF
- Treatment
- Lifestyle
- Weight Reduction
- Exercise
- Decreased Salt Intake
- Decreased Alcohol Intake
- Drugs
- Low-dose, long-acting diuretic, such as 12.5 mg daily of hydrochlorothiazide
- Low-dose, long-acting, dihydropyridine calcium channel blocker
- If patient also has angina, a beta-blocker is appropriate
- If patient also has renal insufficiency or cardiomyopathy, an ACE is a good choice
- If patient also has benign prostatic hypertrophy, an alpha blocker is a reasonable choice
Hypertension and Kidney Disease Template
The association between hypertension in both primary and secondary conditions is well defined. The unique aspect of Kidney disease and hypertension is that hypertension can both be a cause of and a result of kidney disease.
This is a duplicate of the Hypertension template in the Renal Disease Suite of Templates. The template begins with the following concepts:
- High blood pressure can be either a cause or a consequence of chronic kidney disease.
- High blood pressure causes a faster decline in kidney disease and cardiovascular disease.
- Prevalence of high blood pressure is related to the level of GFR.
- Patients with chronic kidney disease have a high prevalence of high blood pressure even when GFR is only mildly reduced.
Mechanism of HBP in Kidney Disease - this launches a document which addresses this issue.
Beneath this link, there are boxes which document:
- Blood Pressure (this visit)
- Blood Pressure History (Hypertension Mgmt)
- Beginning Blood Pressure
- Highest Blood Pressure
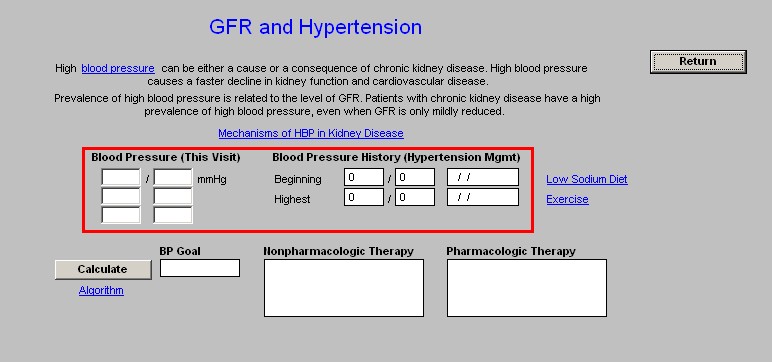
There is then a button entitled "Calculate" when depressed it fills in the following boxes:
- BP Goal
- Nonpharmacologic Therapy
- Pharmacologic Therapy
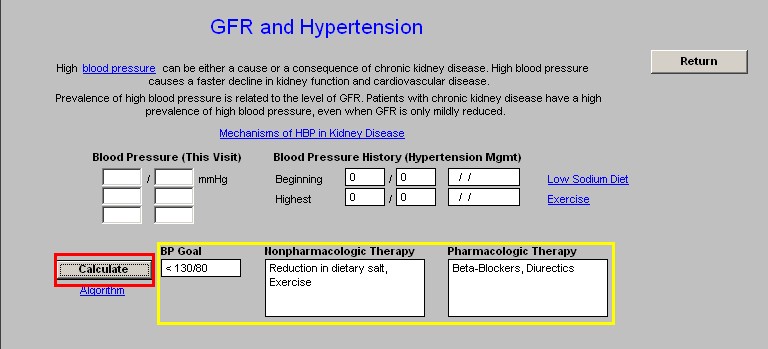
Algorithm - this button launches a pop-up which lists the National Kidney Foundation Blood Pressure Recommendations on the basis of which the above boxes are completed automatically.
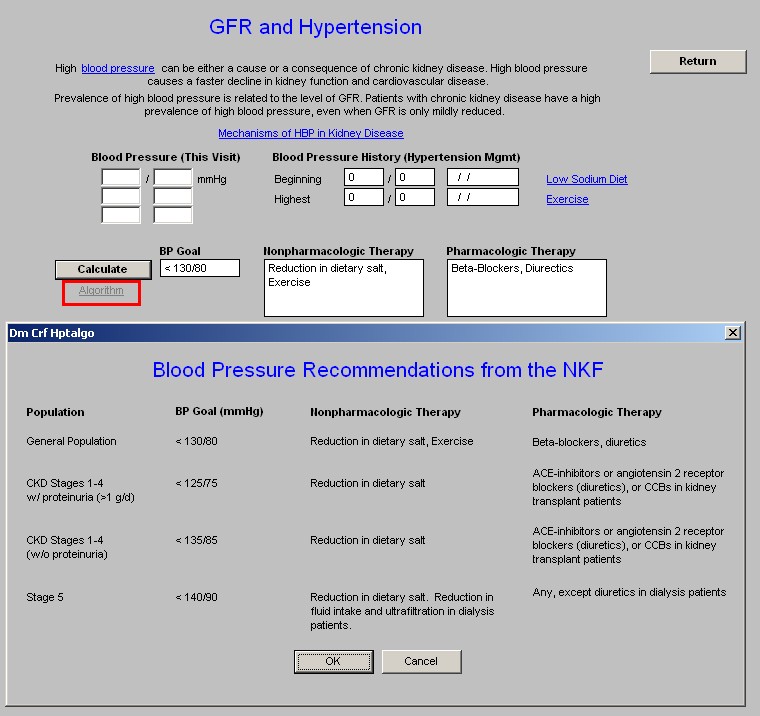
There are two links related to lifestyle changes which improve hypertension particularly in relationship to kidney disease; they are:
Evaluation Template
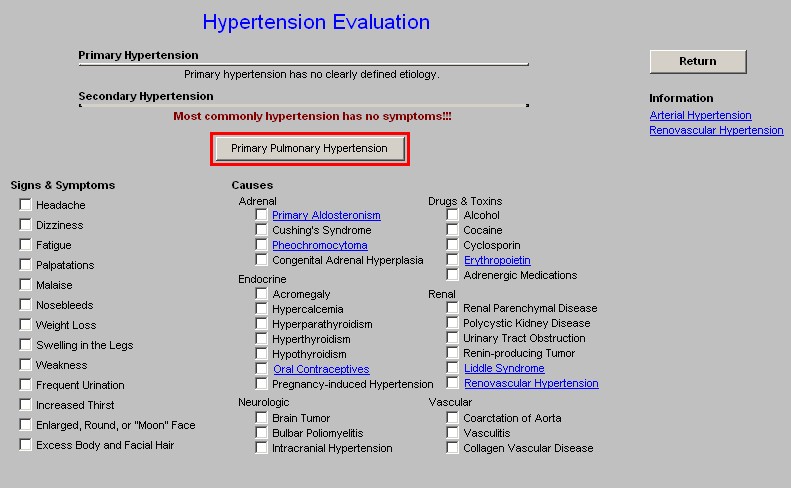
The Evaluation Template has the following content:
Displays the two major types of hypertension:
- Primary Hypertension - has no clearly defined etiology
- Secondary Hypertension - often has no symptoms
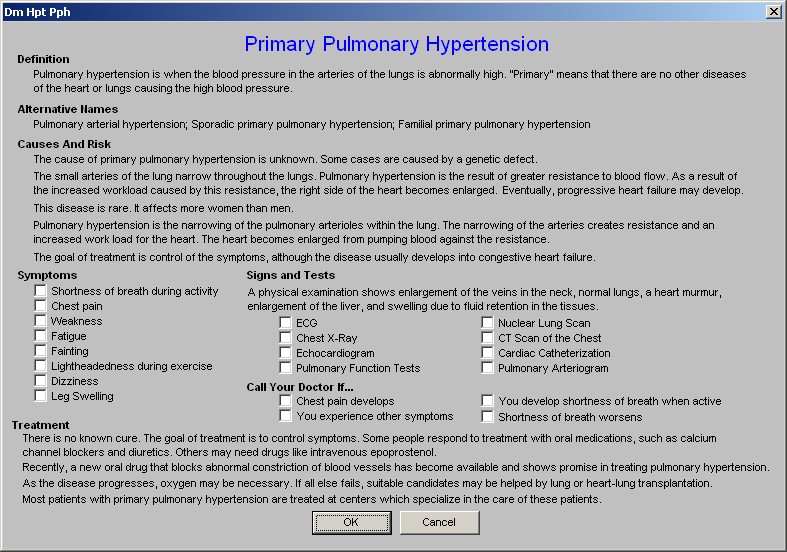
Just below this information is a button entitled "Primary Pulmonary Hypertension".
Primary Pulmonary Hypertension is not a part of systemic hypertension but is presented here because of the close association of the name.
- Definition -- Pulmonary hypertension is when the blood pressure in the arteries of the lungs is abnormally high. "Primary" means that there are no other diseases of the heart or lungs causing the high blood pressure.
- Alternative Names -- Pulmonary arterial hypertension; Sporadic primary pulmonary hypertension; Familial primary pulmonary hypertension
- Causes And Risk -- The cause of primary pulmonary hypertension is unknown. Some cases are caused by a genetic defect.
- The small arteries of the lung narrow throughout the lungs. Pulmonary hypertension is the result of greater resistance to blood flow. As a result of the increased workload caused by this resistance, the right side of the heart becomes enlarged.
- This disease is rare. It affects more women than men.
- Pulmonary hypertension is the narrowing of the pulmonary arterioles within the lung. The narrowing of the arteries creates resistance and an increased work load for the heart. The heart becomes enlarged from pumping blood against the resistance.
- The goal of treatment is control of the symptoms, although the disease usually develops into congestive heart failure.
- Symptoms
- Shortness of breath during activity
- Chest pain
- Weakness
- Fatigue
- Fainting
- Lightheadedness during exercise
- Dizziness
- Leg Swelling
- Signs and Tests
- A physical examination shows enlargement of the veins in the neck, normal lungs, a heart murmur, enlargement of the liver, and swelling due to fluid retention in the tissues.
- Tests
- ECG
- Chest X-Ray
- Echocardiogram
- Pulmonary Function Tests
- Nuclear Lung Scan
- CT Scan of the Chest
- Cardiac Catheterization
- Pulmonary Arteriogram
- Call Your Doctor If...
- Chest pain develops
- You develop shortness of breath when active
- Shortness of breath worsens
- You experience other symptoms
- Treatment
- There is no known cure. The goal of treatment is to control symptoms. Some people respond to treatment with oral medications, such as calcium channel blockers and diuretics. Others may need drugs like intravenous epoprostenol.
- Recently, a new oral drug that blocks abnormal constriction of blood vessels has become available and shows promise in treating pulmonary hypertension.
- As the disease progresses, oxygen may be necessary. If all else fails, suitable candidates may be helped by lung or heart-lung transplantation.
- Most patients with primary pulmonary hypertension are treated at centers which specialize in the care of these patients.
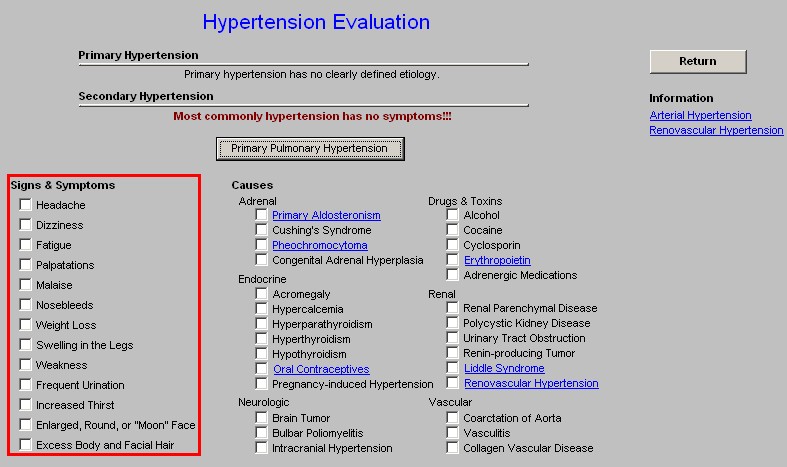
There are two series of checkboxes in the last section on the "Hypertension Evaluation" screen entitled "Signs & Symptoms" and "Causes". While most patients with hypertension have no signs or symptoms, these are sometimes associated with secondary hypertension:
Signs & Symptoms
- Headache
- Dizziness
- Fatigue
- Palpitations
- Malaise
- Nosebleeds
- Weight Loss
- Swelling in the legs
- Weakness
- Frequent Urination
- Increased Thirst
- Enlarged, Round, or "Moon" Face
- Excess Body and Facial Hair
Causes
- Adrenal
- Primary Aldosteronism
- Cushing's Syndrome
- Pheochromocytoma
- Congenital Adrenal Hyperplasia
- Endocrine
- Acromegaly
- Hypercalcemia
- Hyperparathyroidism
- Hypothyroidism
- Oral Contraceptives
- Pregnancy-induced hypertension
- Neurological
- Brain Tumor
- Bulbar Poliomyelitis
- Intracranial Hypertension
- Drugs and Toxins
- Alcohol
- Cocaine
- Cyclosporin
- Erythropoietin
- Adrenergic Medications
- Renal
- Renal Parenchymal Disease
- Polycystic Kidney Disease
- Urinary Tract Obstruction
- Renin-producing Tumor
- Liddle Syndrome
- Renovascular Hypertension
- Vascular
- Coarctation of Aorta
- Vasculitis
- Collagen Vascular Disease
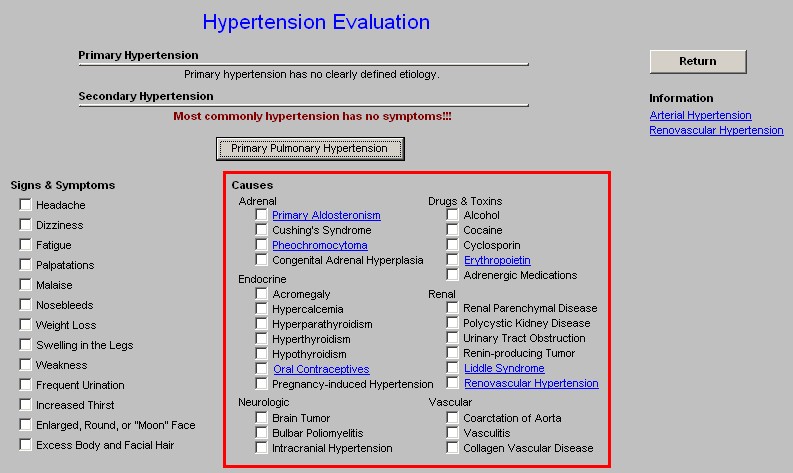
NOTE: All Causes listed in blue are linked to a detailed document describing that cause
At the right hand side of the Evaluation template is a Return button that takes you back to the Master Hypertension template and
Beneath the Return button are two Provider education documents
- Arterial Hypertension - this button launches a document entitled "Arterial Hypertension: Etiology and Pathogenesis."
- Renovascular Hypertension - this button launches a document entitled the same as the button.
Diagnosis and Screening Template
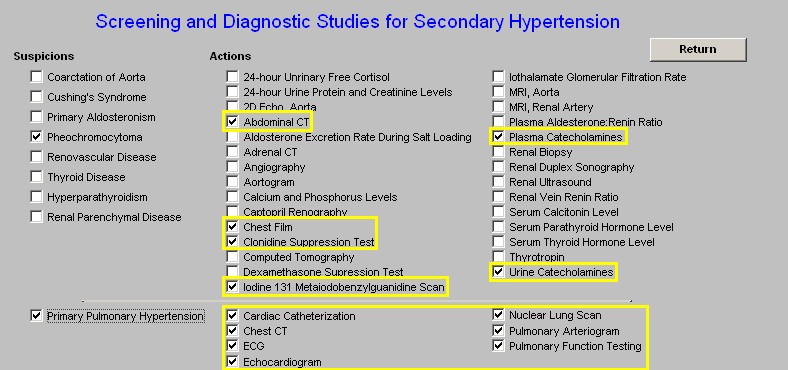
This template provides the ability for the provider to establish a plan for evaluating secondary forms of hypertension. In addition to identifying the most common causes of secondary hypertension, this template provides a tool to suggest the proper evaluation for patients with a suspected secondary cause of hypertension.
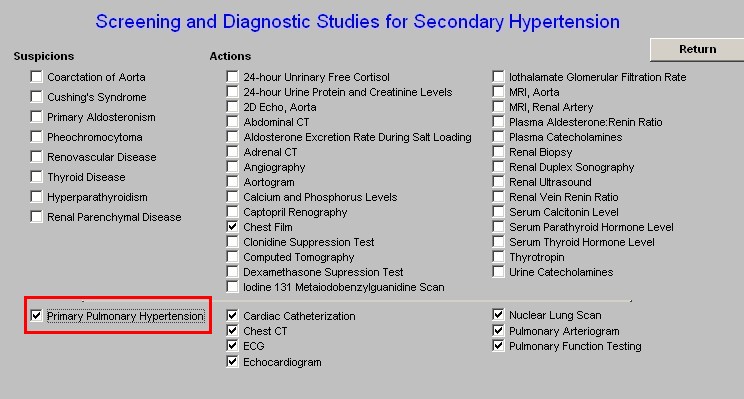
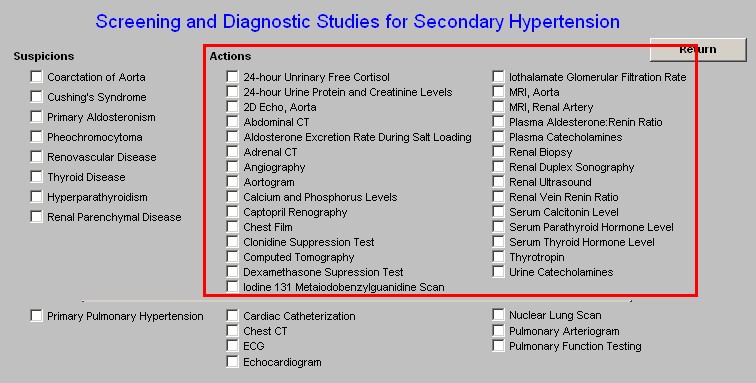
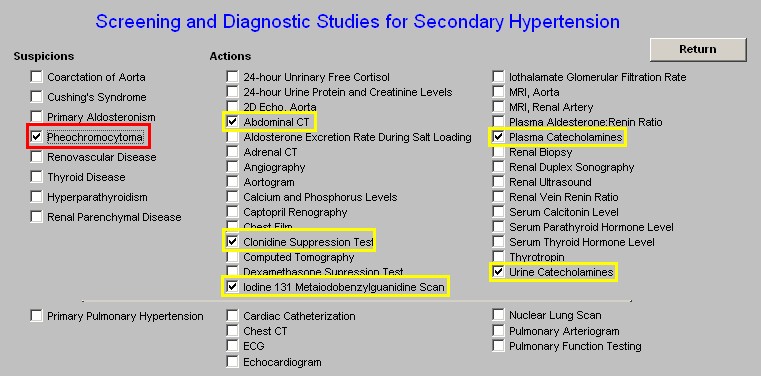
When the "Diagnosis and Screening" button is clicked, it will display an interactive function entitled "Screening and Diagnostic Studies for Secondary Hypertension." There are two sections on this part of the template, the first is "Suspicions" and the second is "Actions."
Suspicions
- Coaractation of the Aorta
- Cusingh's Syndrome
- Pheochromocytoma
- Renovascular Dsiease
- Thyroid Disease
- Hyperparathyroidism
- Renal Parenchymal Disease
There are check boxes in front of each of these causes of secondary hypertension. If you suspicion one of these conditions to be present, check the box in front of the condition and a list of actions recommended for the evaluation of that condition will be automatically selected.
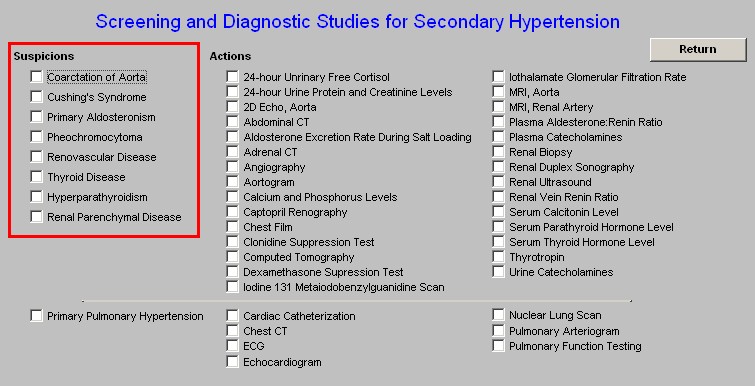
- Primary Pulmonary Hypertension - this is not pathophysiologically a part of hypertension but it is included here because it does result in hypertension in the pulmonary vasculature and it is an increasingly diagnosed condition.
Actions
- 24-hour urinary Free Cortisol
- 24-hour Urine Protein and Creatinine Levels
- 2D Echo, Aorta
- Abdominal CT
- Aldosterone Excretion Rate during Salt loading
- Adrenal CT
- Angiography
- Aortogram
- Calcium and Phosphorous Levels
- Captopril Renography
- Chest Film
- Clonidine Suppression Test
- Computed Tomography
- Dexamethasone Suppression Test
- Iodine 131 Metaiodobenzylguandine Scan
- Iothalamate Glomerular Filtration Rate
- MRI, Aorta
- MRI, Renal Artery
- Plasma Catecholamines
- Renal Biopsy
- Renal Duplex Sonography
- Renal Ultrasound
- Renal Vein Renin Ratio
- Serum Calcitonin Level
- Serum Parathyroid Hormone Level
- Thyrodropin
- Urine Catecholamines
- Cardiac Cauterization
- Chest CT
- ECG
- Echocardiogram
- Nuclear Lung Scan
- Pulmonary Arteriogram
- Pulmonary Function Testing
For instance, if you suspect a Pheochromocytoma, check the box beside that name and the following will automatically have the boxes beside them checked
- Abdominal CT
- Clonindine Suppression Test
- Iodine 131 Metaiodobenzyguanidine Scan
- Plasma Catecholamines
- Urine Catecholamines
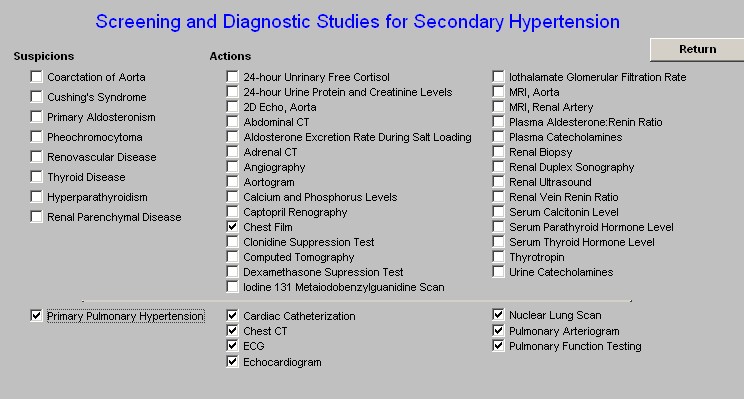
If you think the patient has Primary Pulmonary Hypertension, check the box beside that name and the following will automatically have the boxes beside them checked:
- Chest Film
- Chest CT
- ECG
- Echocardiogram
- Nuclear Lung Scan
- Pulmonary Arteriogram
- Pulmonary Function Testing
Treatment Template
This template pulls together many of the previously discussed principles of hypertension management.
The Hypertension Treatment Template addresses the following issues:
- You need one drug for every 10 mm Hg of systolic blood pressure reduction
- The vast majority of patients will need two, three or possibly four medications.
- Drugs that confer an additional cardiovascular benefit beyond direct blood pressure effects are particularly attractive options.
- Data from seven landmark trials found that between 2.5 and 4.0 antihypertensive agents were required to bring blood pressure to target.
Five steps to Hypertensive control
- Begin and/or continue lifestyle modifications
- Goal Blood pressure
Note that the goal blood pressure is lower in a patient with diabetes and renal disease: 110/70 or lower.
- Initial Drug Choice
Select one of the following (when one of the below is selected by checking in the box next to it), Recommended Drug(s) will appear on the template.
- Uncomplicated Hypertension
- Type 1 Diabetes w/proteinuria
- Heart Failure
- Isolated Systolic hypertension
- History of MI
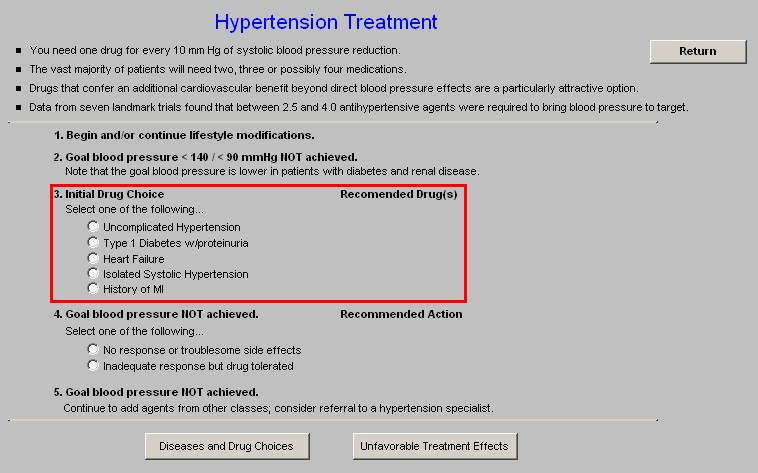
- Goal Blood pressure NOT achieved
Select one of the following
No response or troublesome side effects Inadequate response but drug tolerated
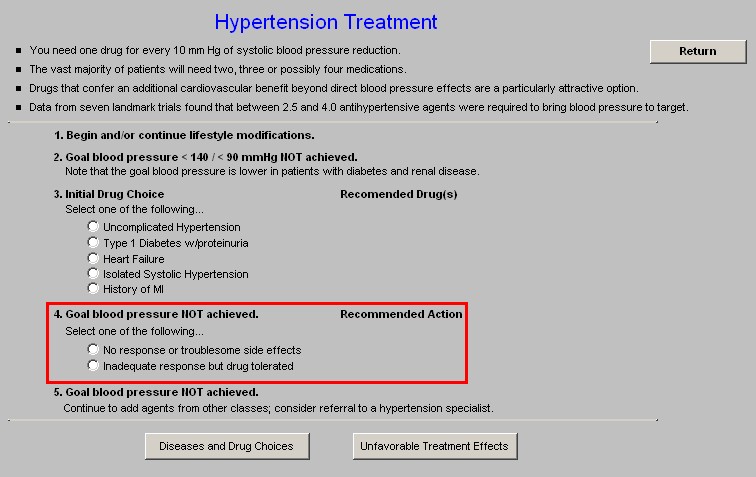
- Goal Blood Pressure NOT achieved
Continue to add agents from other classes, consider referral to a hypertension specialist.
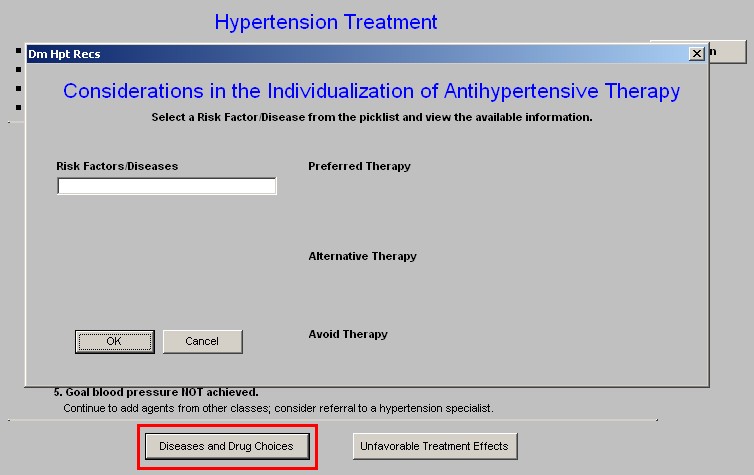
There are two pop-ups on this template:
- Diseases and Drug choices - there is a box which when accessed displays the following pick list. When one of the disease states is selected, the second box displays the optimal medicine for treating hypertension in this circumstance.
Risk/Factors Diseases
- African-American
- Angina
- Atrial Fibrilation
- Caucasian
- CHF
- Chronic Renal Failure
- Cough Caused by ACE Inhibitors
- Diabetes w/Nephropathy
- Diabetes w/o Nephropathy
- Diabetes w/o Nephropathy w/Systolic HPT
- Dyslipidemia
- History of MI
- Hyperkinetic Circulation
- Hypertension, Uncomplicated
- Impotence From Other Drugs
- Isolated Systolic Hypertension
- Left Ventricular Failure Due To Systolic Dysfunction
- Left Ventricular Hypertrophy
- Migraine Headaches
- Obesity
- Old Age
- Paroxysmal Supraventricular Tachycardia
- Peripheral Artery Disease
- Pregnancy
- Prostatism
- Proteinuria in Chronic Renal Disease
- Renal Disease
- Senile Tremor
- Systolic Dysfunction
- Youth
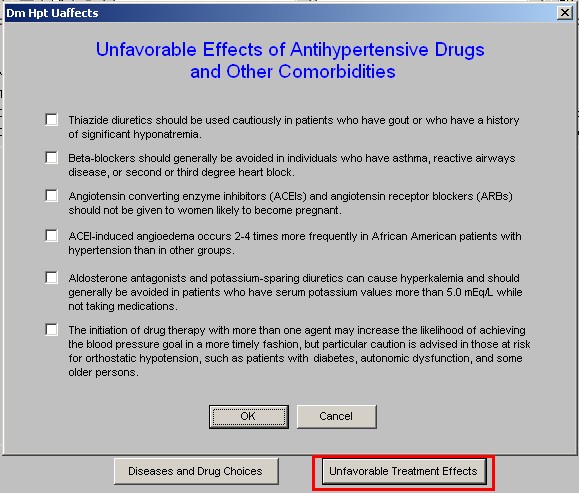
- Unfavorable Treatment Effects - this addresses side effects to hypertensive medications which are not desirable.
- Thiazide diuretics should be used cautiously in patients who have gout or who have a history of significant hyponatremia.
- Beta-blockers should generally be avoided in individuals who have asthma, reactive airways disease, or second or third degree heart block.
- Angiotensin converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) should not be given to women likely to become pregnant.
- ACEI-induced angioedema occurs 2-4 times more frequently in African American patients with hypertension than in other groups.
- Aldosterone antagonists and potassium-sparing diuretics can cause hyperkalemia and should generally be avoided in patients who have serum potassium values more than 5.0 mEq/L while not taking medications.
- The initiation of drug therapy with more than one agent may increase the likelihood of achieving the blood pressure goal in a more timely fashion, but particular caution is advised in those at risk for orthostatic hypotension, such as patients with older persons.
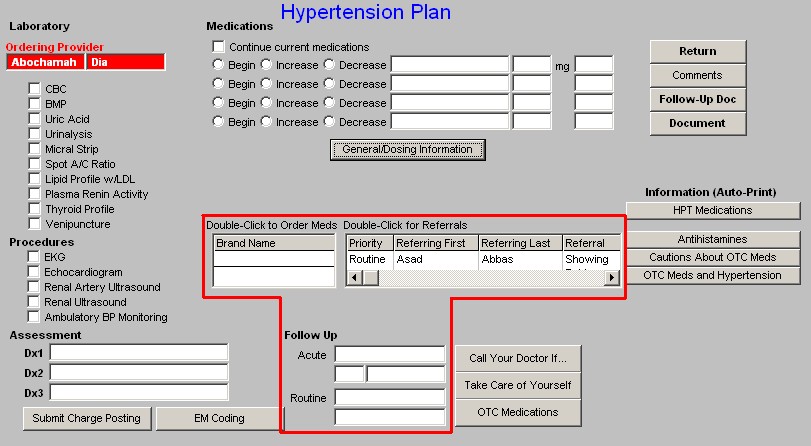
Hypertension Plan Template
This template facilitates the documentation of the plan which has been developed by the working through of the Hypertension Suite of Templates.
The Hypertension Plan Template is divided into three columns:
Column 1 -
Laboratory - these labs can be ordered from the Hypertension Plan Template and charge posted as well
- CBC
- BMP
- Uric Acid
- Urinalysis
- Micral Strip
- Spot A/C Ratio
- Lipid Profile
- Plasma Renin Activity
- Thyroid Profile
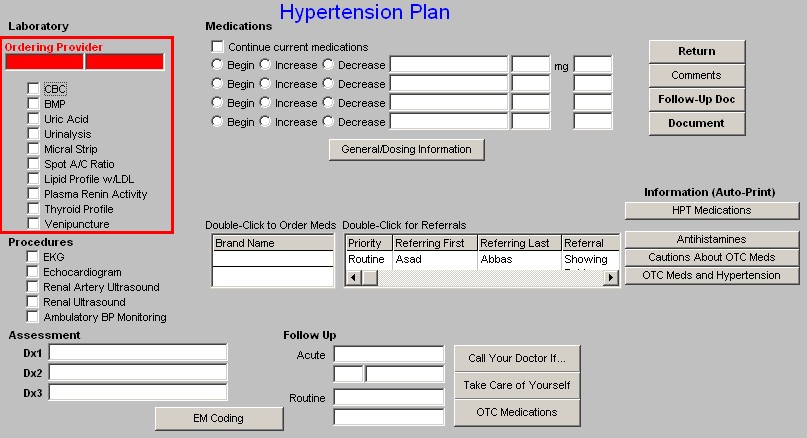
Procedures - these procedures and tests can be ordered and charge posted from the Hypertension Plan Template.
- EKG
- Echocardiogram
- Renal Artery Ultrasound
- Renal Ultrasound
- Ambulatory BP Monitoring
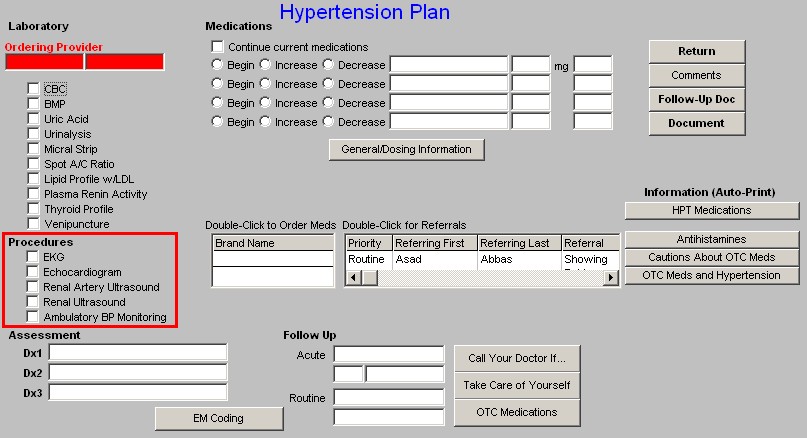
Assessment - this makes it possible to select the appropriate ICD-9 codes from the Hypertension Plan Template.
Dx1 - this first diagnosis box has a pick list made up only of hypertension ICD-9 Codes
DX2 - these next two have pick list made up of all of SETMA's ICD-9 codes
Dx3
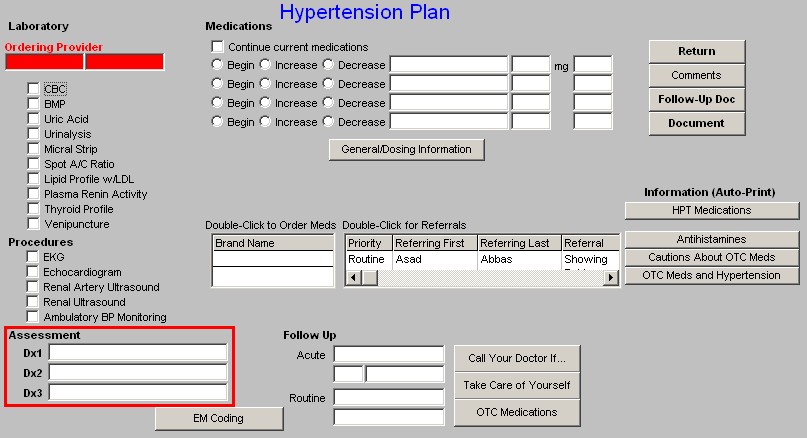
Submit Charge Posting - Once the Assessment is completed and the laboratory and procedures have been selected, depressing this buttion completes charge posting, sending the orders to the lab, x-ray, etc., and putting this data on the patient's chart note.
E & M Coding - This links the provider to the E&M Charge posting template. For more information on Charge posting go to Charge Posting Tutorial or E & M Coding go to E & M Coding.
Column 2 -
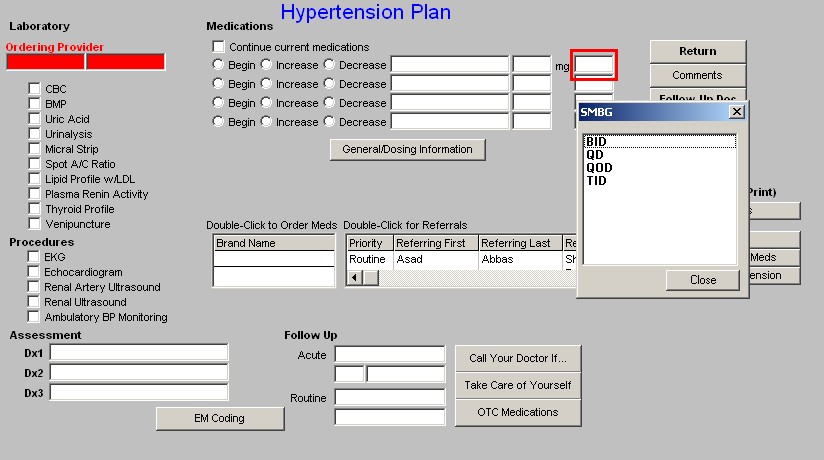
Medications -- There are four sets of boxes where medications can be added, increased, decreased. The pick list which is attached to these boxes is:
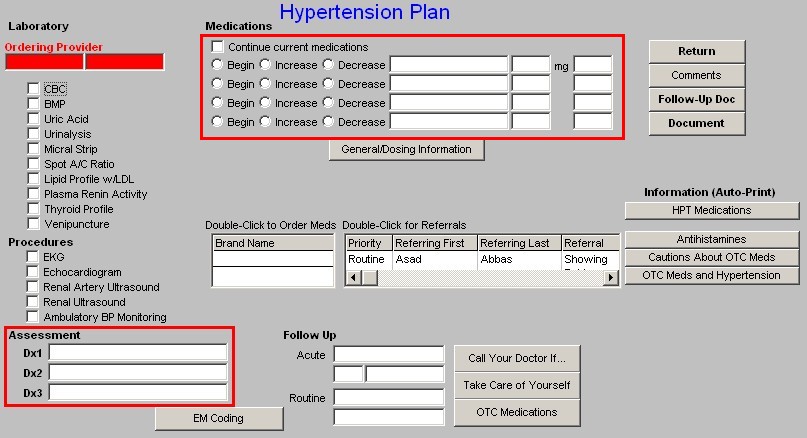
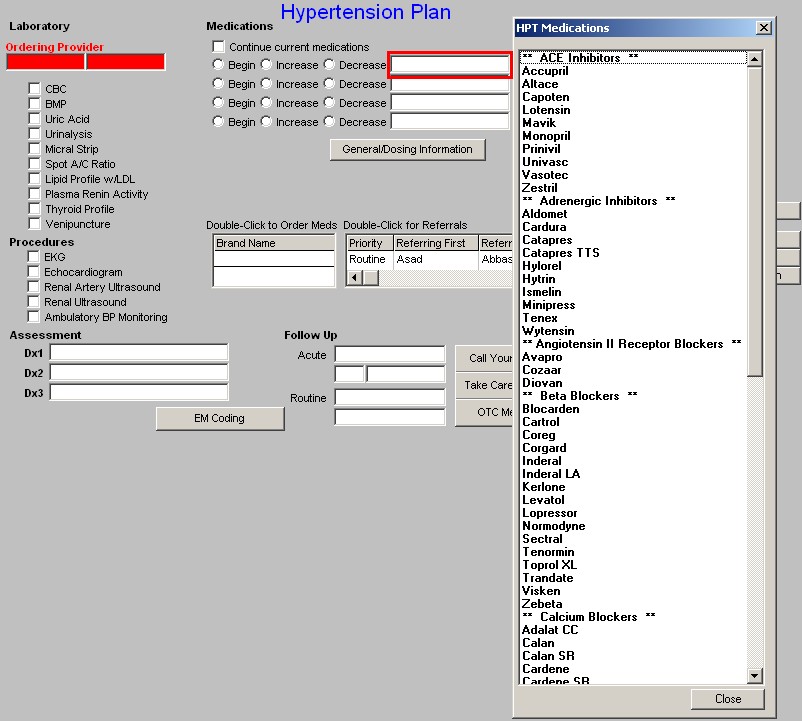
- ACE Inhibitors
- Accupril
- Altace
- Capoten
- Lotensin
- Mavik
- Monopril
- Prinivil
- Univasc
- Vasotec
- Zestril
- Adrenergic Inhibitors
- Aldomet
- Cardura
- Catapres
- Catapres TTS
- Hylorel
- Hytrin
- Ismelin
- Minipress
- Tenex
- Wytensin
- Angiotensin II Receptor Blockers
- Avapro
- Cozaar
- Diovan
- Beta Blockers
- Blocarden
- Cartrol
- Coreg
- Corgard
- Inderal
- Inderal LA
- Kerlone
- Levatol
- Lopressor
- Normodyne
- Sectral
- Tenormin
- Toprol XL
- Trandate
- Visken
- Zebeta
- Calcium Blockers
- Adalat CC
- Calan
- Calan SR
- Cardene
- Cardene SR
- Cardizem CD
- Cardizem SR
- Covera-HS
- Dilacor XR
- DynaCirc
- DynaCirc CR
- Isoptin
- Isoptin SR
- Norvasc
- Plendil
- Procardia XL
- Sular
- Tiazac
- Verelan
- Oral Diuretics
- Aldactazide-25
- Aldactazide-50
- Aldactone
- Bumex
- Damadex
- Diucardin
- Diuril
- Dyazide
- Dyrenium
- Edecrin
- Enduron
- Esidrix
- HydroDiuril
- Hygroton
- Lasix
- Lozol
- Maxzide
- Maxzide-25
- Microzide
- Midamor
- Moduretic
- Mykrox
- Naturetin
- Oretic
- Thalitone
- Zaroxolyn
- Vasodiltors
- Apresoline
- Loniten
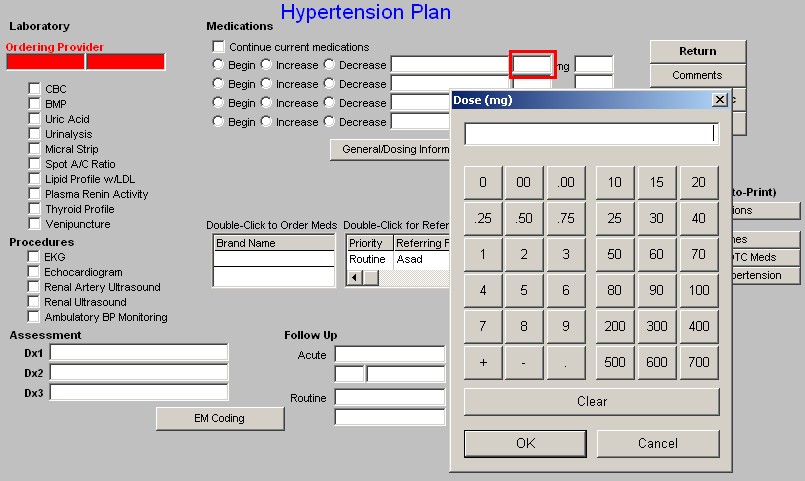
General/Dosing Information
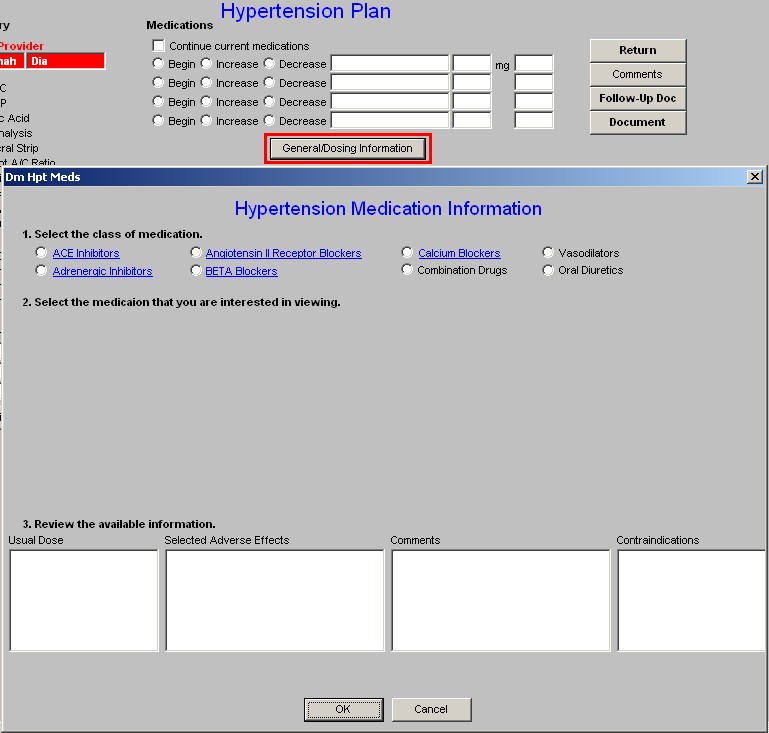
This is an electronic PDR where a class of drugs can be chosen from:
- Ace Inhibitors
- Adrenergic Inhibitors
- Angiotensin II Receptor Blockers
- Beta Blockers
- Calcium Blockers
- Combination Drugs
- Vasodilators
- Oral Diuretics
Once the class of drugs is chosen, the available drugs from that class are displayed. When you select one of those drugs by check the box beside it, the following information is displayed:
- Usual Dosage
- Selected Adverse Effects
- Comments
- Contraindications
Beneath this function are links to the:
- Medication Module
- Referrals Template
Follow-up
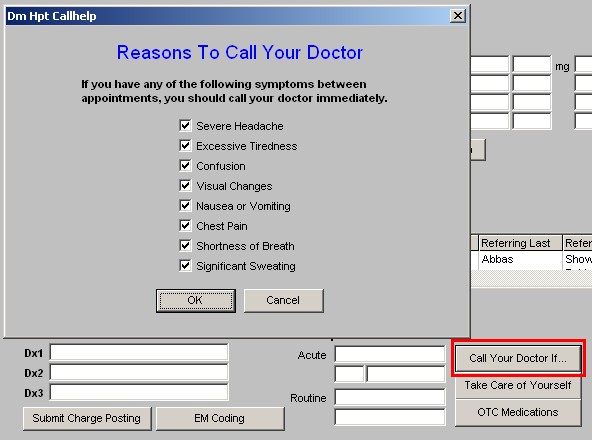
There are then three Pop-ups with the following content. Each of these prints on the Hypertension Follow-up Note automatically.
- Call Your Doctor if. -- If you have any of the following symptoms between appointments, you should call your doctor immediately.
- Severe Headache
- Excessive Tiredness
- Confusion
- Visual Changes
- Nausea or Vomiting
- Chest Pain
- Shortness of Breath
- Significant Sweating
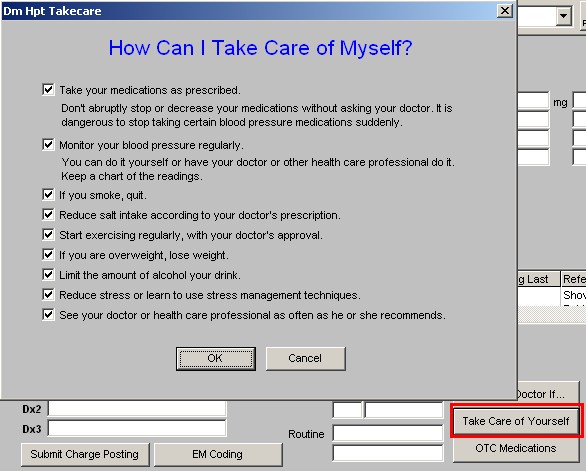
- How Can I Take Care of Myself?
- Take your medications as prescribed. -- Don't abruptly stop or decrease your medications without asking your doctor. It is dangerous to stop taking certain blood pressure medications suddenly.
- Monitor your blood pressure regularly. -- You can do it yourself or have your doctor or other health care professional do it. Keep a chart of the readings.
- If you smoke, quit.
- Reduce salt intake according to your doctor's prescription.
- Start exercising regularly, with your doctor's approval.
- If you are overweight, lose weight.
- Limit the amount of alcohol your drink.
- Reduce stress or learn to use stress management techniques.
- See your doctor or health care professional as often as he or she recommends.
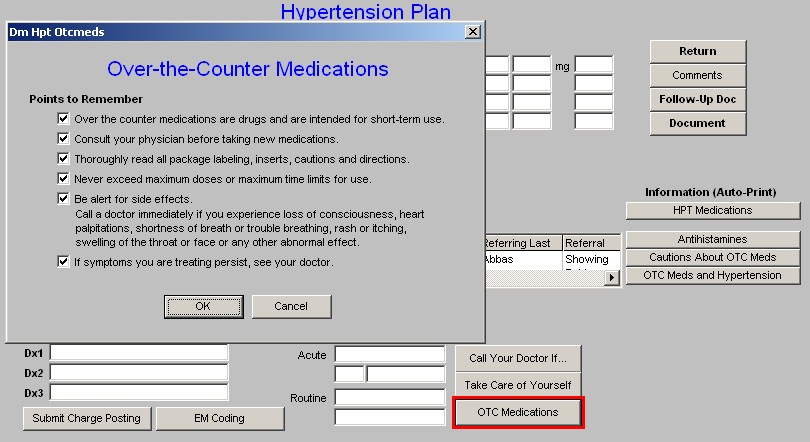
- Over-the-Counter Medications
Points to Remember
- Over the counter medications are drugs and are intended for short-term use.
- Consult your physician before taking new medications.
- Thoroughly read all package labeling, inserts, cautions and directions.
- Never exceed maximum doses or maximum time limits for use.
- Be alert for side effects.
- Call a doctor immediately if you experience loss of consciousness, heart palpitations, shortness of breath or trouble breathing, rash or itching, swelling of the throat or face or any other abnormal effect.
- If symptoms you are treating persist, see your doctor.
Column 3 -
- Return - this takes you back to the Hypertension Master Template.
- Comments - this allows for free text comments which do not logically fit anywhere else.
- Follow-up Doc - this creates the Hypertension Follow-up Document which should then be given to the patient.
- Document - this creates the Hypertension Chart Note
Information
- HPT Medications - when this button is depressed it launches a list of documents on the following medications, each of which can be printed.
- ACE Inhibitors and Angiotensin II Blockers
- Adrenergic Inhibitors
- Beta Blockers
- Calcium Channel Blockers
- Combination Drugs
- Oral Diuretics
- Vasodilators
- Antihistamines
- Cautions About OTC Meds
- OTC Meds and Hypertensions
Physician Role Template
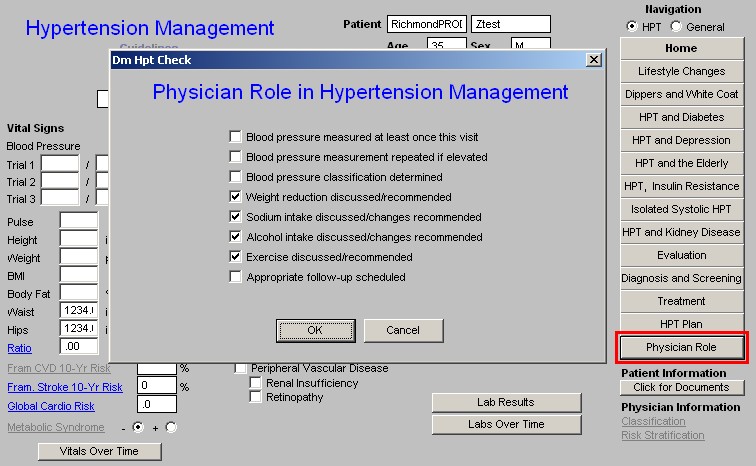
As the provider progresses through SETMA's Hypertension Suite of Templates, this template automatically collects the data points for the Physician Consortium for Performance Improvement Data for quality of care in hypertension management. A review of this template will allow a provider to see "how he/she is doing," as measured against a national standard of care in hypertensive management. The standard of excellence in the management of hypertension is measured on the following 8 data points.
Physician Role in Hypertension Management
- Blood pressure measured at least once this visit
- Blood pressure measurement repeated if elevated
- Blood pressure classification determined
- Weight reduction discussed/recommended
- Sodium intake discussed/changes recommended
- Alcohol intake discussed/changes recommended
- Exercise discussed/recommended
- Appropriate follow-up scheduled
The Physician Consortium for Performance Improvement
The Physician Consortium for Performance Improvement (Consortium) is a group of clinical and methodological experts convened by the AMA. The Consortium includes representatives from more than 60 national medical specialty and state medical societies, the Agency for Healthcare Research and Quality, and the Centers for Medicare and Medicaid Services.
The Consortium's vision is to fulfill the responsibility of physicians to patient care, public health, and safety by:
- becoming the leading source organization for evidence-based clinical performance measures and outcomes reporting tools for physicians; and
- ensuring that all components of the medical profession have a leadership role in all national forums seeking to evaluate the quality of patient care.
The Consortium's mission is to improve patient health and safety by:
- identifying and developing evidence-based clinical performance measures that enhance quality of patient care and that foster accountability;
- promoting the implementation of effective and relevant clinical performance improvement activities; and
- advancing the science of clinical performance measurement and improvement.
The Consortium works to develop evidence-based clinical performance measures and clinical outcomes reporting tools to support physicians in quality improvement efforts.
The Consortium has published a number of disease management data sets which established quality of care measures with which physicians and other healthcare providers can measure their own performance.
|