For many reasons, the long-term residential-care setting presents serious and unique challenges to excellence of care for patients who require such placement. Perhaps the most significant challenges are in the following areas:
SETMA’s commitment to dignified, personal and excellent care for all who require long-term-residential care, whether due to advanced age and infirmity, disability and infirmity, or other reasons, has resulted in the forming of a team of healthcare professionals to coordinate and deliver that care. This team is supported by a reference laboratory, mobile x-ray service and hospital-care team which provide a continuity of care between the outpatient, inpatient, and residential-care settings.
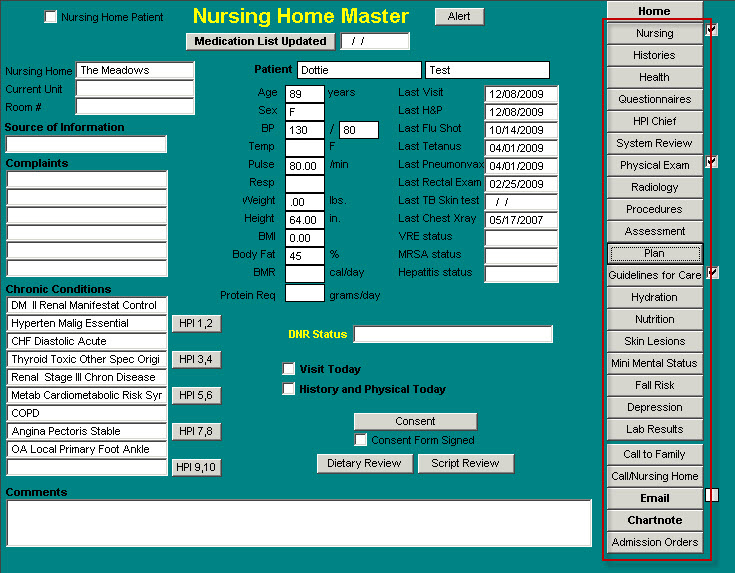
With this commitment SETMA has expanded the use of electronic patient records, and, electronic patient management, into the long-term residential-care setting. The Nursing Home Suite of Templates is the foundation of that expansion.
The Nursing Home Suite of Templates consists of:
- Master Nursing Home Template
- Nursing
- Histories
- Health
- Questionnaires
- HPI
- System Review
- Physical Exam
- Radiology
- Procedures
- Assessment
- Plan
- Guidelines for Care
- Hydration
- Nutrition
- Skin Lesions
- Mini Mental Status
- Fall Risk
- Depression
- Lab Results
- Call to Family
- Call/Nursing Home
- E-mail
- Chart note
- Admission Orders
Templates 2-15, 20 and 25 are discussed and dealt with elsewhere. Links to each of these are provided above to avoid redundancy in this tutorial. Please refer to those links for how to use those templates.
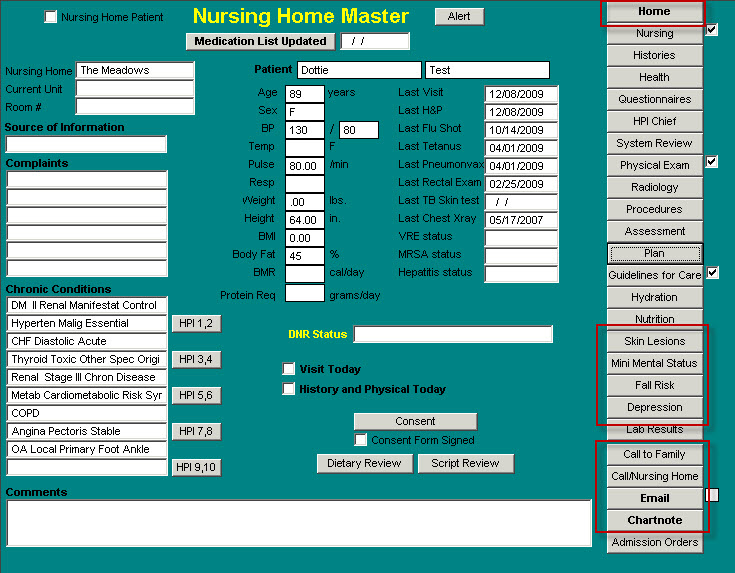
This tutorial will focus upon:
- Master Nursing Home
- Skin Lesions
- Mini Mental Status
- Fall Risk
- Depression
- Call to Family
- Call/Nursing Home
- E-mail
- Chart Note
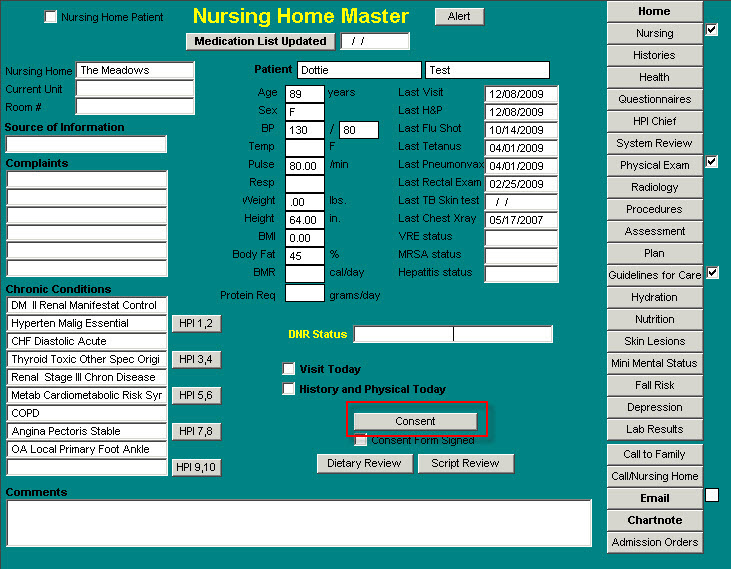
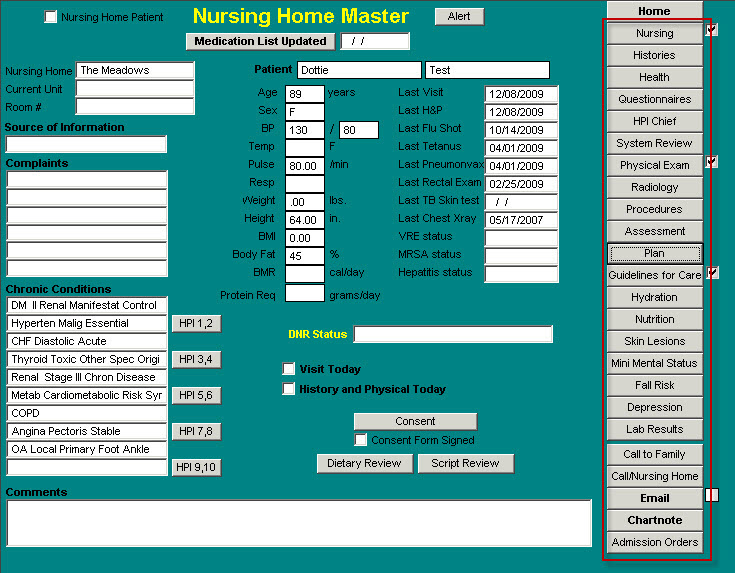
Master Nursing Home Template
At the top of the template are the following information and functions:
- A box for designating that this patient is a Nursing Home Patient – this is administrative and allows the querying of the system to evaluate the care of all patients in the nursing home.
- The title of the template
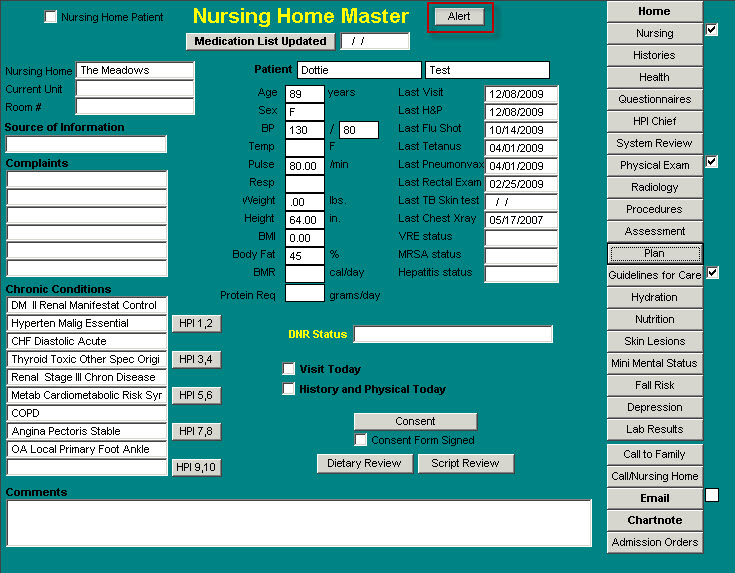
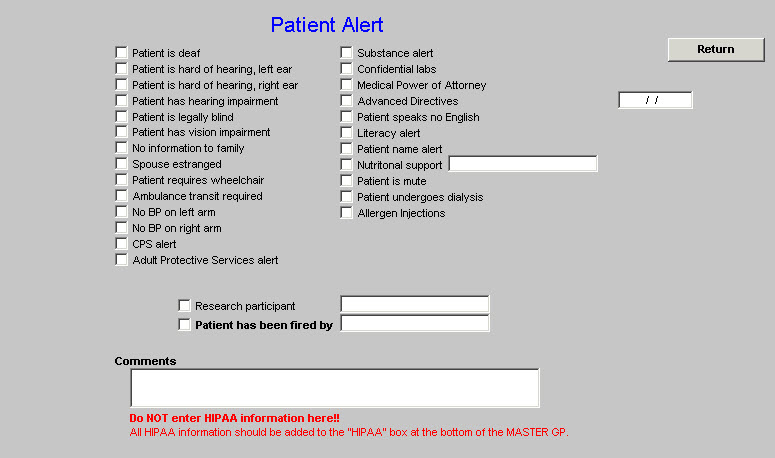
- Alert – this is a button which launches a template with a number of special circumstances which can be documented about this patient. Such as: patient is deaf,; patient is legally blind, etc.
Beneath the name of the template is a button entitled Medication List Updated. Next to this button is a date field. When this button is depressed, the current date appears in the date field.
One of the most important and complex tasks in long-term residential care is the maintaining of an accurate, up-to-date list of the current medications which the patient is receiving, while at the same time maintaining an accurate history of the patient’s medication use. This function allows the healthcare provider to know when the medication list was last updated so as to have some degree of confidence that the mediation list is complete and correct.
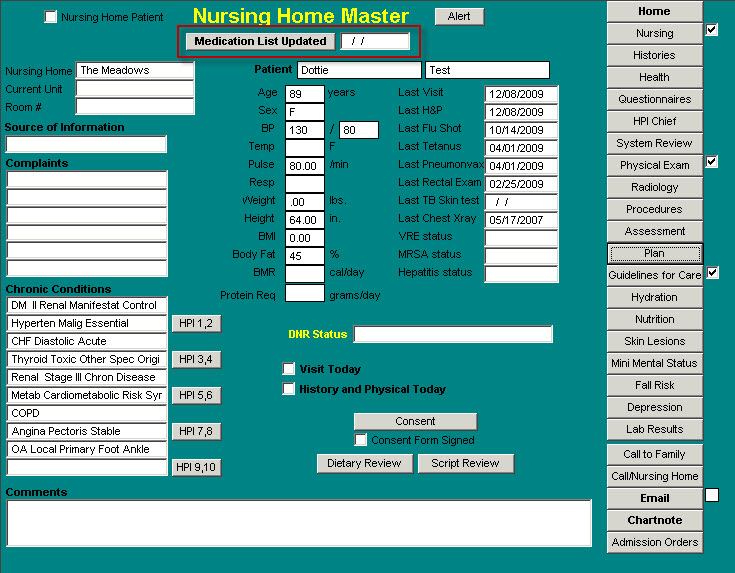
Beneath the Medication List Updated button is the patient’s name and to the left of that is the name of the Nursing Home, the Current Unit and the patient’s room number. The Current Unit addresses the type of unit, i.e., Alzheimer, Long Term Care, or Skilled Nursing Unit.
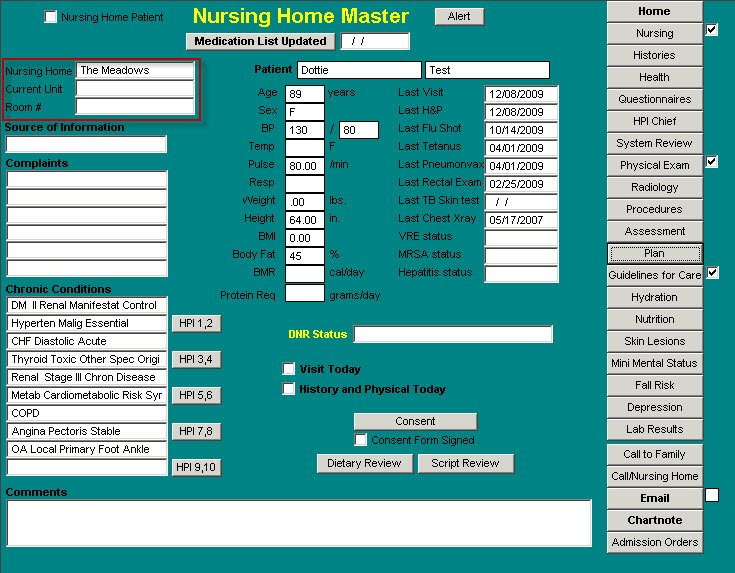
The Master Nursing Home Template is then divided into three sections vertically, with the middle section having two columns.
The left-hand section consists of:
- Source of Information – the options on the pick list are: Caregiver, family member, patient.
- Complaints – this is the same as the Chief Compliant on the Master GP. For information on how to complete this function see the Chief Compliant tutor.
- Chronic Conditions – for information on using the Chronic Conditions function see the tutorial on Chronic Conditions.
- Comments – this is a box for typing in free texts for information which does not easily fit into a structured field above.
The second section consists of:
Column 1 – Vital signs
Column 2 – a list of important information which is unique to the long-term care setting as to its need to be on the Master Template:
- Last Visit
- Last H&P
- Last Flu Shot
- Last Tetanus
- Last Pneumovax
- Last Rectal Exam
- Last TB Skin Test
- Last Chest X-ray
- VRE Status
- MRSA Status
- Hepatitis Status
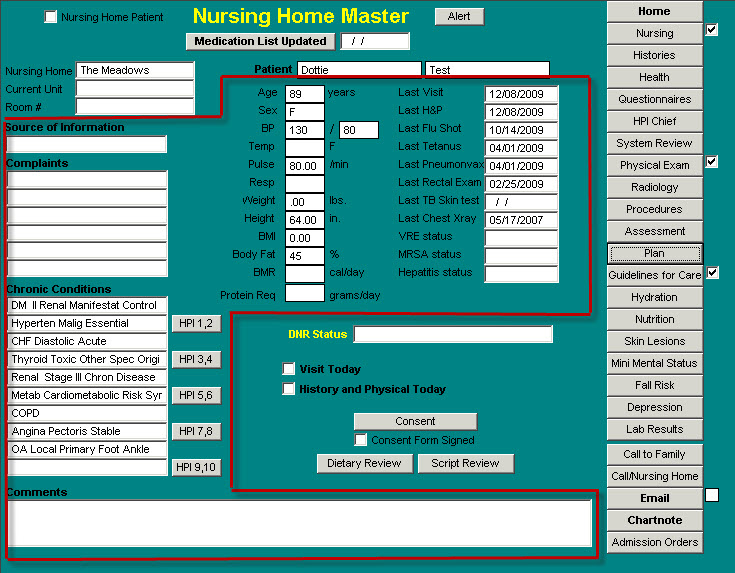
At the bottom of this second section are the following:
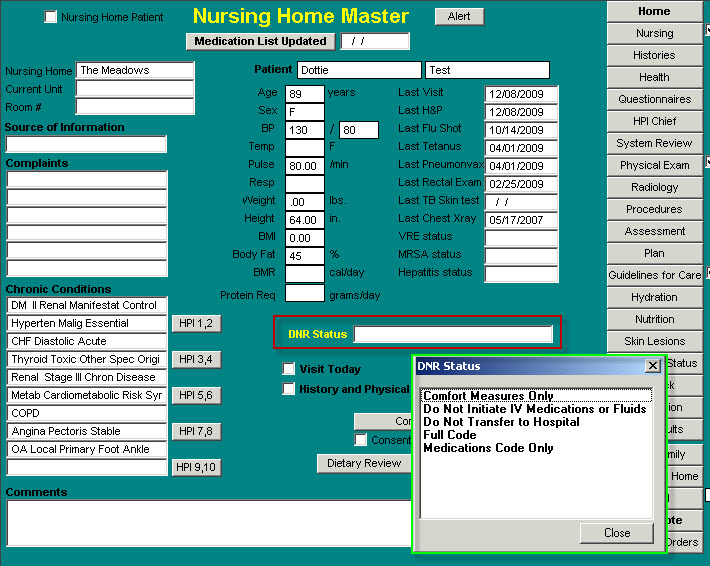
- DNR Status. – the following options are on the pick list
- Visit Today – this allows the provider to document that a visit was completed today. This updates the Last Visit function above.
- H&P Today – this allows the provider to document that a history and physical was completed today. This updates the Last H&P function above.
- Consent – for details see below
- Consent Form Signed – this allows the provider to document whether or not the patient and/or family has signed the Disclosure and Consent to Admission document. For an explanation of this document, see below.
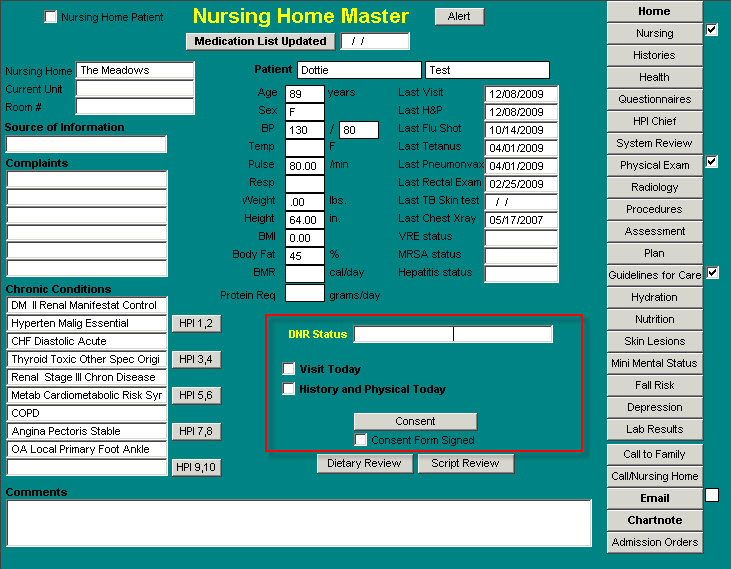
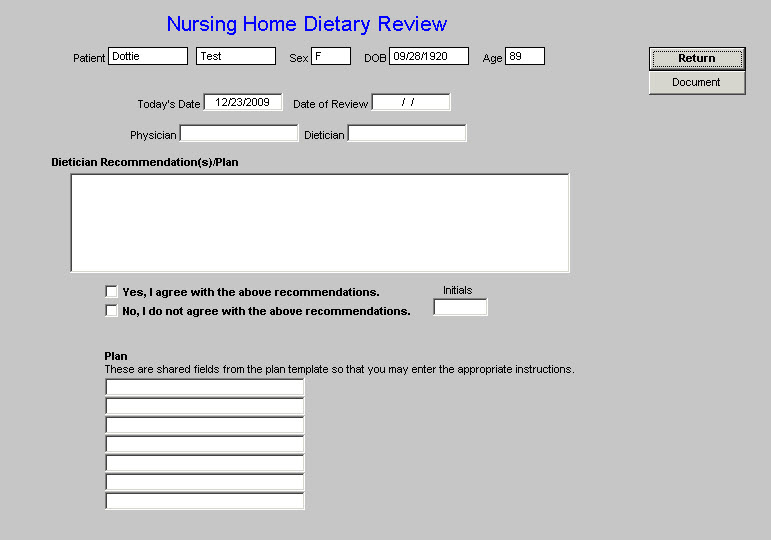
- Dietary Review – this template is entitled Nursing Home Dietary Review. This allows the provider to review the recommendations of the nursing home dietician and to print a document which can be placed on the patient’s chart with the details of that review.
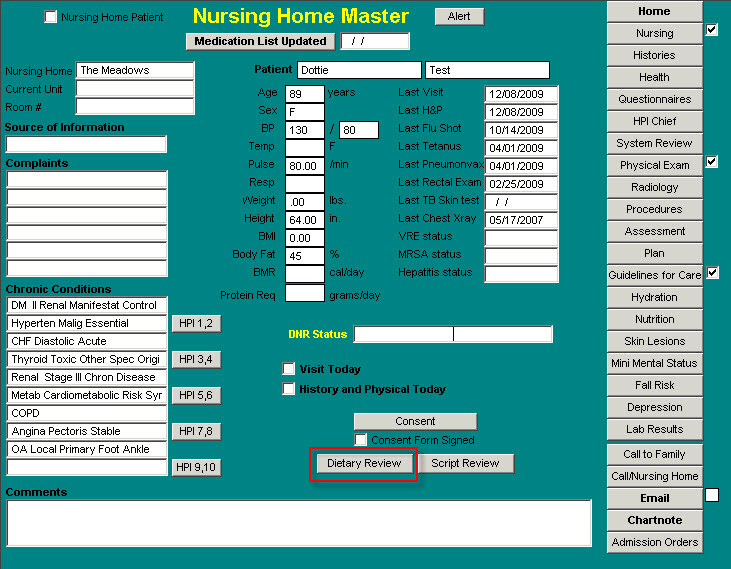
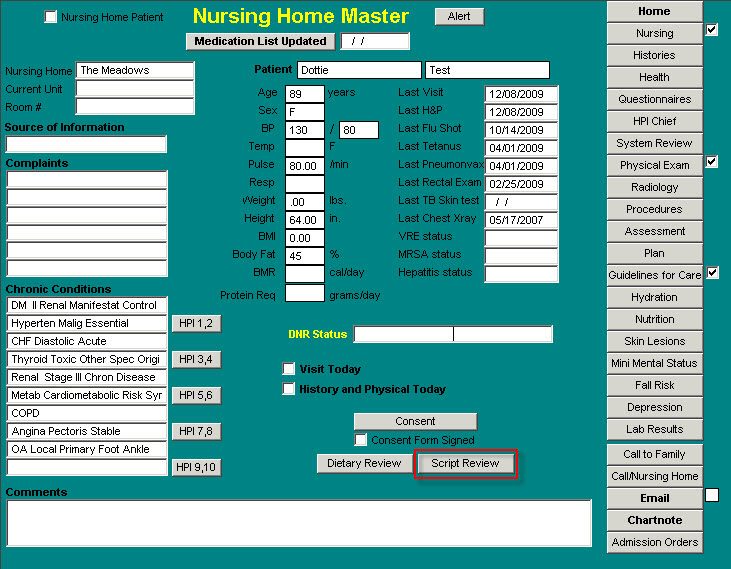
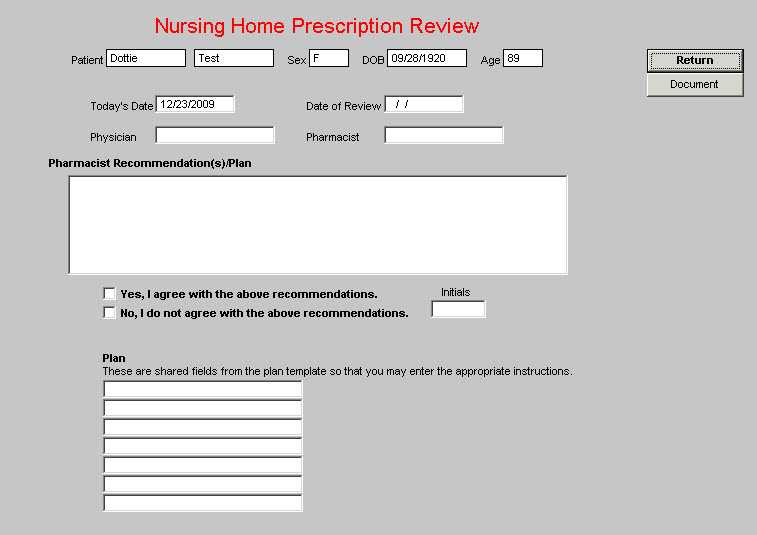
- Script Review – This template is entitled Nursing Home Prescription Review. This allows the provider to review the recommendations of the nursing home pharmacist and to print a document which can be placed on the patient’s chart with the details of that review.
The button discussed above entitled “Consent,” launches a template entitled “Disclosure and Consent to Admission.”
The template contains:
- The Patient’s Name
- Chronic Conditions
- Chief Complaints
- Dietary Review
- Other Conditions or changes that warrant admission to a Long-Term Care Facility
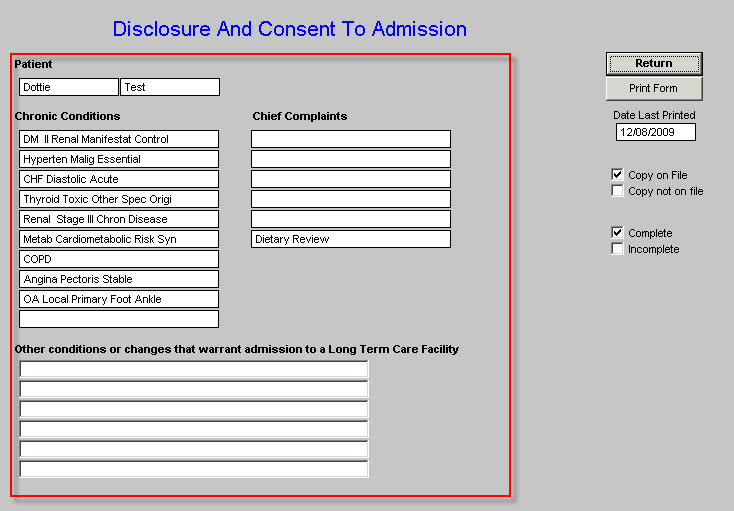
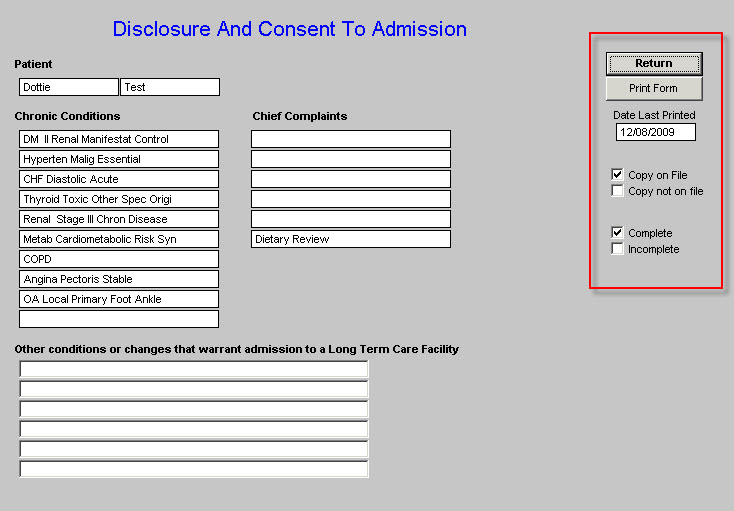
The Disclosure and Consent to Admission Template also has the following options for documentation:
- Print Form
- Date Last Printed
- Copy on File
- Copy Not on File
- Complete
- Incomplete
Once the nursing home admission history and physical examination is completed, this document should be generated and presented to the family and/or patient for signing. A signed copy should go to the Nursing Home,. to the Family and a signed copy should be scanned into the patient’s electronic medical record.
The Disclosure and Consent to Admission document has the following content. Attached to this text below will be the evaluation of the patient’s:
- Hydration status,
- Nutritional status,
- Fall risk assessment,
- Skin evaluation and
- Depression evaluation.
Text of the Form
DISCLOSURE AND CONSENT TO ADMISSION
To A Long Term Care Facility
This form must be completed after disclosure and consent is obtained by a physician.
It has been determined that (Patient’s Name) is no longer able to function without assistance in carrying out the activities of daily living. This deterioration is critical and has been caused by problems associated with aging, as well as the following acute and chronic medical diagnosis (list):
Patient’s Diagnoses will be automatically entered here
The patient is currently on the following medications:
Patient’s Medication list will be automatically entered here
Most of the medical conditions are irreversible and progressive, and the patient is not expected to survive these underlying medical conditions. In conjunction with pathological changes associated with aging and necessary treatment, the medical conditions may cause the following complications and problems:
Musculo-skeletal neurologic changes including weakness, loss of sensation, loss of motor function and mobility, loss of balance and fractures, paralysis, loss of bowel and bladder function, memory loss, confusion, inability to communicate, blood pressure problems, disorientation, weight loss, inability to swallow, depression, anxiety, hostility, aggressiveness, loss of appetite, dementia, hallucinations, pathological fractures, emboli, joint contractures, joint swelling, joint and muscle pain, degenerative changes, of the spine, head, neck, back and extremity pain, loss of consciousness, coma and death;
Cardiovascular changes including chest, back and extremity pain, skin lesions/wounds/ulcers, weakness, cardiac arrhythmias, congestive heart failure, heart attack, stroke, loss of consciousness, coma, weight loss, fluid and electrolyte imbalance, blood clots, emboli, thrombosis, occlusion of major small vessels ( aorta, major arteries to internal organs, brain periphery-extremities), difficulty breathing, aspiration, kidney damage, inability to repair damaged tissue, blood pressure problems and death;
Immunologic & hematologic changes including infections and repeated infections, antibiotic therapy and complications of resistance to antibiotics, loss of immune response, gastrointestinal disturbances, skin lesions/wounds/ulcers, loss of appetite, weight loss, skin reactions, inability to repair damaged tissue, fluid and electrolyte imbalance, connective tissue damage, difficulty breathing, anemia, kidney damage, adrenal gland dysfunction, coma and death;
Gastrointestinal and nutritional changes including inability to absorb nutrients, loss of immune response, infections and repeated infections, protein loss, inability to swallow, aspiration, choking, liver and pancreas dysfunction, weight loss, inability to repair damaged tissue, skin lesions/wounds/ulcers, gastrointestinal pain, fluid and electrolyte imbalance, esophageal-gastrointestinal lesions/ulcers, coma, diarrhea, constipation and fecal impaction, anemia, hemorrhage and death;
Pulmonary changes including pneumonia, infections and repeated infections, drug reaction, choking, hemorrhage, skin lesions/wounds/ulcers, bronchitis, heart problems, arrhythmias, lack of tissue oxygenation, inability to repair damaged tissue/heal, loss of appetite, weight loss, confusion, disorientation, brain damage, coma, death, and
There are inherent risks to being admitted to a facility that has an aging population:
The above enumerated problems are usually worsened, or may appear for the first time, after a patient moves into a new environment, especially a long term care facility, as that move is associated with the end of life. Withdrawal of familiar people and family also is associated with medical and psychological deterioration. Neither the resident nor responsible persons can expect the facility staff and physicians to replace the attention that only can be provided by family and those who are familiar with this patient. It is essential to the health of the resident that family be involved in his/her care and decisions.
The patient neither will be living in a private home nor cared for by a member of the family who is familiar with the resident. The standard of services in a long term care facility does not include one care provider for every patient. Staff will periodically monitor, observe and provide care and treatment based on physician orders. At times, the patient will be left alone.
When care and services are refused by the patient, they will not be forced upon the patient. Staff and physicians will not over-ride the patients will and choice.
This patient will be living in a community of people who also are aging and have the problems of aging which exposes the patient to communicable disease, unpredictable reactions from other residents and accidents.
The food and recipes are institutional, and it is important for the family to stay involved with nutrition, as loss of appetite commonly results from change and loss of familiar surroundings and people.
RELEASE AND WAIVER OF LIABILITY BY PATIENT
I have been fully informed and I understand that the physicians and medical practitioners who prescribe and provide medical treatment (including, but not limited to, the medical director, psychiatrists, dentists, optometrists, nurse practitioners and physicians assistants) are not employees, agents or representatives of the long term care facility, but are independent practitioners.
I understand that I have a choice of nursing home and long term care facilities to which I/the patient will be admitted.
In consideration for admission into the long term care facility, I hereby release Southeast Texas Medical Associates, L.L.P. (“SETMA”) and its staff, for all liability for personal injury or death that results from negligence or gross negligence in following the physicians and medical practitioners orders and instructions, and I also release SETMA and its staff from all liability for negligence and gross negligence that results in personal injury or death. I further release the physicians from liability for personal injury or death by negligence or gross negligence that results from following the physicians and medical practitioners orders and instructions, and from actions taken by employees of the long term care facility of my choice.
I have been fully informed and I understand that this release of liability is binding on me, my family, estate, heirs and assignees.
I certify that I have been informed of the contents of this document, that I have read it, or it has been read to me, it has been fully explained to me, and I have been given the opportunity to ask questions about the document, including the fact that I am releasing and waiving liability, and I have sufficient information to give this release and waiver of liability.
I understand that if any part of this release and waiver of liability should later be found void, voidable, or ineffective, the finding shall have no effect on the remainder, which shall remain in full force and effect.
Patient Signature Date
I understand that I have a choice of nursing home and long term care facilities to which I/the patient will be admitted.
I certify that I have been informed of the contents of this document, that I have read it or it has been read by me, it has been fully explained to me, and I have been given opportunity to ask questions about the document, my/the patients condition, long term care, care and treatment, associated risks and hazards involved, and I certify that no warranty or guarantee has been made to me, and I have sufficient information to give this consent to admission.
I hereby consent to admission of (Patient’s Name) to Southeast Texas Medical Associates, LLP.
Patient Signature Date
Master Nursing Home Right-hand Section
25 Navigation Buttons identified above.
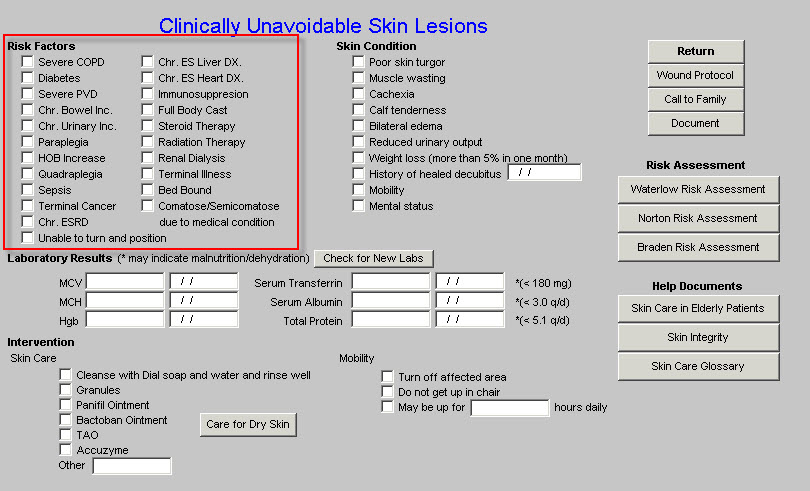
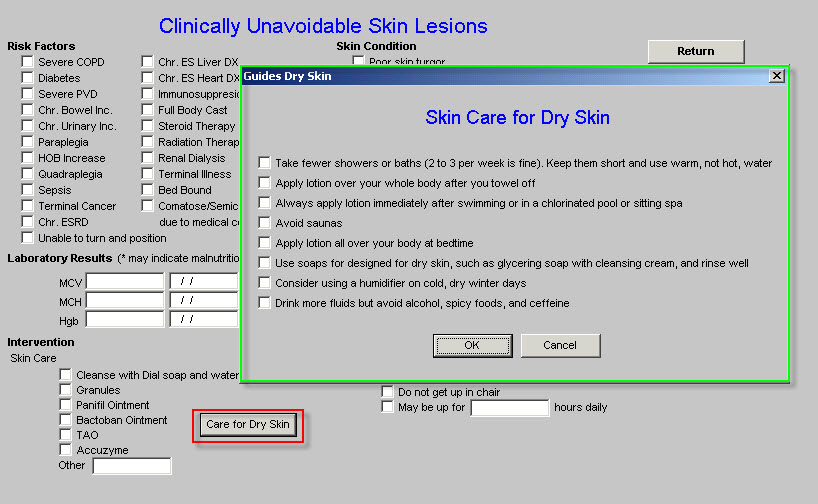
Skin Lesions Template
The next template which is unique to the Nursing Home Suite of Templates is Skin Lesions. The full name of the template is “Clinically Unavoidable Skin Lesions.”
Skin lesions are common in long-term care facilities, and often are unavoidable. This template helps identify the patients who are at risk of unavoidable skin lesions.
The template is organized into three vertical sections.
The left-hand section has two columns.
Risk Factors – 22 conditions are listed which contribute to the patient’s being at risk for “Clinically Unavoidable Skin Lesions.” These should be reviewed and any risk factors which apply to the patient should be documented by checking the box next to it. These are in demographic fields, which means that once they are checked, they remain checked in subsequent visits until they are unchecked.
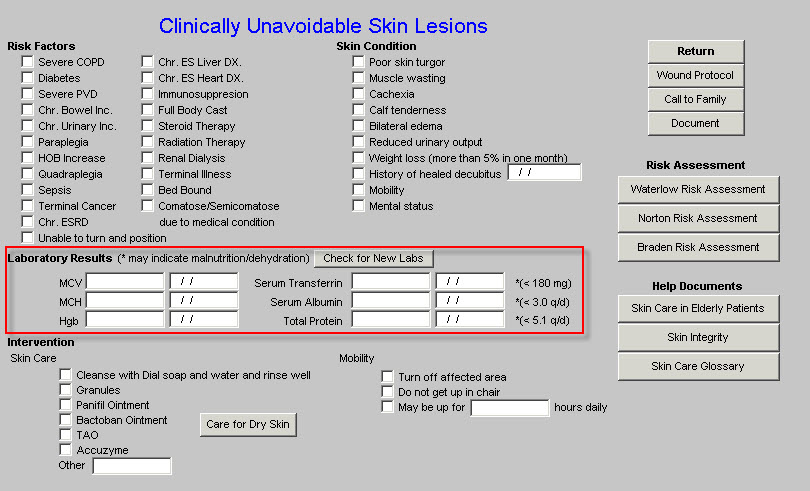
Laboratory Results –
There are six laboratory results here which impact the ability of the patient to heal wounds and/or which indicate the presence of chronic malnutrition which would prevent wound healing. There is a button entitled Check for New Lab which allows you to import the most recent lab values on this patient. Additional information on the patient’s nutritional status can be found on the Nutrition Template. To learn more about the Nutrition template, visit the Nutrition tutor. To review the tests necessary to evaluate the patient’s nutritional status, see the Lab Charge Posting template
Intervention ---
This section addresses 6 skin-care options and 3 Mobility options for improving skin care. However, in the presence of the above mentioned Risk Factors and in the presence of clinically unavoidable malnutrition, maintaining the integrity of the skin is not possible.
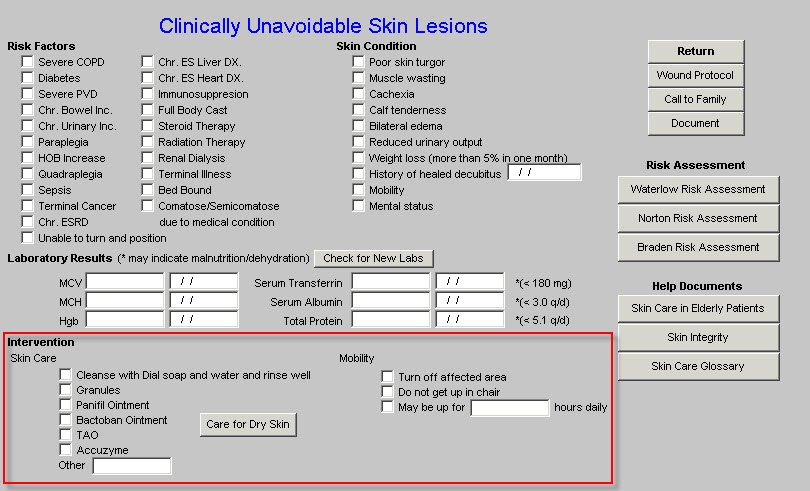
At the very bottom of this left-hand section is a button entitled Care for Dry Skin. When launched 8 options for caring for dry skin appear. There are boxes which allow the selecting of certain options which will then appear on the chart note.
Middle Section of Clinically Unavoidable Skin Lesions Template
Skin Condition – this provides the opportunity to document 10 skin conditions which contribute to Clinically Unavoidable Skin Lesions.
Right-hand section of Clinically Unavoidable Skin Lesions Template
NH Master – this is a navigation button back to NH Master Template
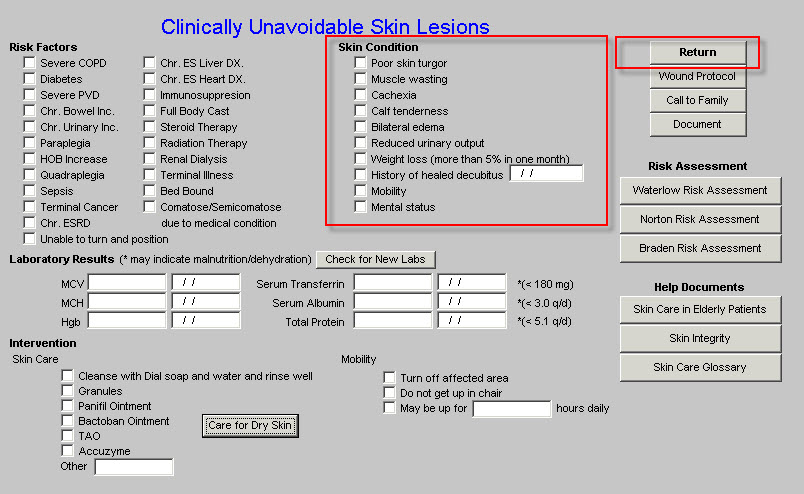
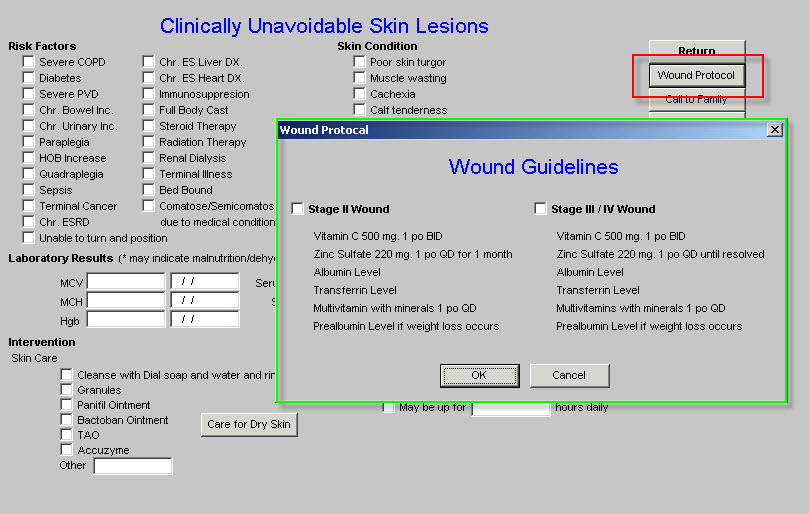
Wound Protocol – this launches the Wound Protocol pop-up which gives treatment guidelines for Stage II wounds and for Stage III/IV Wounds. This is a different guideline than that for the Skin Tear Guidelines
This is a test which assesses the presence of dementia. The scale allows for the assessment over time to evaluate the patient’s changing state of mental capacity. The questionnaire is self explanatory as to its use.
This is one of the greatest health threats to all elderly patients but particularly to those who are in long-term residential care. Through the review of seven categories, a score is developed which indicates whether the patient is at high risk or low risk of falls.
In addition to the seven categories for review with the elements of each, the template has three Instruction pop-ups.
Under the navigation button for NH Master at the right hand side of the template is a link to the Guidelines for Fall Prevention.
Depression is a serious and often life-threatening problem in the elderly and particularly in the elderly in long-term residential care facilities. In addition, the complexity of mediation treatment of the elderly is greater because they are often on multiple drugs which have serious interactions. While this template is mostly educational, it is key to the successful treatment of residents of long-term care facilities
This is link to the Hypertension and Depression Template in the Hypertension Suite of Templates. For information on how to use this function see the Hypertension and Depression tutor.
This is a standard function in SETMA’s EMR. When accessed this template causes the most recent laboratory values for the tests listed on the template to populate the template. A document can then be created. In addition, once the Lab Results template has been accessed, the lab results will appear on the chart note for that encounter.
This template allows for the documentation of a contact with the family. The template contains the ability to document:
This template allows the provider to document a contact with the Nursing home or Hospital about the patient’s care. The content is self-explanatory.