|
____ Events
June 3, 2013
Editor’s Note: During a healthcare conference in Washington, DC, a consultant made a presentation during which he disparaged several organizations, religious groups, and interests groups whose positions differed from his. The mockery was publicly challenged by me. The organization which sponsored the conference apologized for the speaker’s behavior (see page 11 below) On the day after the conference; I received an e-mail from the speaker “apologizing” (see page 3 below) for his comments. This discussion is because of the nature of the apology.
Response to ___ ____ _______ Conference
Washington, D. C. May __ - __, 2013
Later today, I will complete an analysis of the entire ___ Conference and recommend what I think would be improvements. I thought the conference was poorly organized and seemed to be perfunctorily conducted. It rarely covered the subject which we were promised. It was a waste of time and money for my organization.
This note is to address ____ _____’s “apology.” At the end of my response there is a copy of the previous dialogue between me and the conference leadership about _____ and the event.
Saturday, I received the following note from ____ ______. I, too, hoped that this would be end of this matter, but, alas, it is not. I had hoped that ____ would learn from this episode and deal with others with more respect. Apparently, as is evidence by the distortions in his “apology,” he has not learned anything, but this will be my last comment on this matter.
The very definition of a “sincere apology” is that you accurately describe what you did and you clearly indicate that you agree that what you did was wrong. ____ does the latter but as to the former, he said, as is high-lighted in red below, that “it was not (his) intention for (his) passions on-end-of-life care-coordination to enflamed Dr. Holly’s (passion.” In fact no one objected to his passion about end-of-life issue and I didn’t even address his use of vulgarity and profanity in his presentation which I think is inappropriate. I addressed his prejudicial and bigoted remarks about those with whom he disagrees.
If I had been “enflamed” over his “passions on-end-of-life care coordination”, I would have been contradicting my own professional stands as outlined below, and I would be the one who owed ____ an apology. But, as ____ knows and as all who attended the meeting know, no one objected to the discussion of end-of-life issues. I reacted to ____’s impugning of a news organization which ____ and his fellow-travelers hold in contempt and I further reacted when, in trying to extricate himself from his prior statement, he indicated that what he “really” intended to do was to object to Baptists and to pro-lifers and to those who disagreed with him about Terri Schiavo. (In my August 16, 2006, published letter (discussed below) I addressed a case not dissimilar to the Schiavo case; if ____ disagrees with my position, I accept that, but, “____, disagree with what I said, not your caricature of what I said.”)
A Straw man is easier to debunk than the truth
It is unfortunate that ____ wishes to further his distortion of the views of those with whom he disagrees. Those “inside the beltway” often seem so certain of their superiority that they refuse to deal honestly with the views of those who disagree with them. I do not and I did not object to ____’s passion for end-of-life matters. As is demonstrated below, I am at least as passionate about end-of-life matters as ____, and I may be more so.
I objected to ____’s bigoted and prejudicial attitude toward those whom he finds it easier to ridicule than honestly to address their ideas and ideals. As a deeply committed Christian, I celebrate the right of Jews, Muslims, Hindus, Buddhist and others to believe and to worship as they will. I respect their beliefs and when addressing the content of their beliefs and/or the social implications of their beliefs, I try to make certain that I accurately represent those beliefs. ____ does not, which is often characteristic of those who live and work “inside the beltway.”
As to his overall presentation, I would recommend that ____ read the June 2013 Harvard Business Review’s “How to give a killer presentation.” On page 122, the following is stated, “A successful talk is a little miracle – people see the world differently afterward.” At this conference, ____ seemed to be more interested in impressing us with his glib, clever speaking skills than with enlightening us with insightful and actionable content on the subject of the conference. I wonder what anyone changed in their organization, or what anyone was challenged to change by and after his presentation.
SETMA’s diligence in addressing advanced directives and end-of-life issues is documented our inpatient and ambulatory settings. These results are published for public review on our website at www.jameslhollymd.com. Here are published audits of SETMA’s success in addressing advance directives.
Inpatient addressing of advance directives and/or end-of-life issues
Clinic and/or ambulatory setting addressing of advanced directors and/or end-of-life issues
____’s Saturday, June 1, 2013 note to me and to the leadership of ____ which is so disappointing as an apology, follows.
-----Original Message-----
From: ____ _____ [mailto ______@_______________.com]
Sent: Saturday, June 01, 2013 11:07 AM
Subject: Re: SETMA.com | Public Reporting | Reporting by Type
_____. I am sincerely sorry for my remarks Thursday. As you know I try to shed light not heat and it was not my intention for my passions on end of life care coordination to enflame Dr. Holly's. (Emphasis added) And to Dr. Holly I will offer now my fifth sincere apology and good wishes that we may all move on. I hope you all enjoy the weekend. Regards, ____ ______ _____ Executive Chairman ______ ______Group
Passion for End-of-Life Planning – Declared; Demonstrated Some of SETMA’s articles published over the past eight years about end-of-life matters.
It is one thing to declare that you are “passionate for end-of-life coordination care”, as does ____ ______, which passion, I do not question; is another and more valuable thing to demonstrate that passion in clinic settings.
The following are only a few of SETMA’s publications and thoughts on end-of-life. The date of publication and the hyperlink to where the publication can be found appear first, followed by an excerpt from the article.
June 26, 2012 -- http://jameslhollymd.com/Presentations/SETMA-Provider-Trainning-June-26-2012-Summary-and-Action-Plan-IHI-Transitions
Monthly, SETMA closes all of its office and all providers congregate for training and quality improvement. In June, 2012 and the three following months, SETMA reviewed the Institute for Healthcare Improvement’s (IHI) four documents on transitions of Care. Following each four-hour training session, SETMA published a “Follow-up and Plan of Action” paper which represented what we intended to change due to what we had studied.
This follow-up tracked all of the recommendations from IHI and each recommendation was color coded. Those things we are doing well were coded in black; those we do not do, were in red and those things we do but need to improve upon were in “purple.” The following is in the section of “what should be included in each visit?” As a part of SETMA’s Patient-Centered Medical Home and because of our partnership with hospice, advanced directives are part of our quality management program.
May 14, 2009 http://jameslhollymd.com/Your-Life-Your-Health/Can-More-Care-Provide-Less-Health
This is an article which appeared in SETMA’s weekly newspaper column (This column has been published weekly for fourteen years). It addresses whether “less care can produce more health.” In part the article states:
“What Have We Learned? The last thing any of us wants is a healthcare system in which a patient is denied certain care based on age. In reality, there are some 80-year-old patients who should have a coronary by-pass and there are some 50-year-olds who should not. In addition, just because we can do something does not mean that it is appropriate to do it.
“Often the most loving thing which can do for a parent, a spouse, or for other loved ones is to say ‘no,’ to tests, procedures, or invasive care. The ONLY consideration in healthcare decisions should be the welfare of the patient and often that welfare is best defined by what you choose not to do, rather than by what you choose to do.
“What Should We Do?
- “Encourage primary care. Fewer medical-school graduates are going into primary care because they can make much more money as specialists, no small consideration when faced with paying off six-figure student loans. Medicare is currently studying paying primary-care doctors extra for functioning as a ‘medical home’ for patients, helping to manage their chronic ailments and coordinating care provided by specialists.
- “Find out what really works. The government should fund more research comparing different treatments for common conditions, and then scale reimbursements to encourage the use of the most effective care. That would help discourage the unnecessary treatments and tests found in high-spending regions.
- “Think twice about drastic measures. More aggressive hospitals more often use treatments such as feeding tubes and cardiopulmonary resuscitation in patients nearing death. But those measures might not extend life for long, if at all, and can be uncomfortable.
- “Every adult should have an ‘advance directive’ (available at www.caringinfo.org). It gives your preferences for care in the event you are ill with no prospect of recovery and unable to express your wishes.
- “Consider hospice care for a patient who, in the opinion of doctors, is likely to die within six months. Studies show that patients receiving hospice care on average live slightly longer than those with the same illnesses who are not in hospice. <
- “Don't be pressured into agreeing to invasive life-support treatments, such as feeding tubes, without a thorough discussion of the patient's prognosis, personal preferences (if known), and overall condition. (emphasis added)
“Healthcare reform is a complicated issue with many parties having their own agenda. As healthcare providers, we must continue to advocate for our patients, but that advocacy must not be just to keep doing more, when doing less may be the compassionate, human and right thing to do.”
June, 2009 -- NCQA: Physician Practice Connections – Patient-Centered Medical Home
“SETMA’s Medical Home Coordination Review – this is a 100-page review of SETMA’s Medical Home Coordination Review Template published in 2009 – central to this is Advanced Directive and Code Status. http://jameslhollymd.com/EPM-Tools/pdfs/tutorial-medical-home-coordination-review-tutorial.pdf
“This is the tutorial for SETMA’s Transition of Care Review published in June, 2009 when SETMA Deployed the Physician Consortium for Performance Improvement’s (PCPI) Review Transition of Care Quality Metric Set. http://jameslhollymd.com/EPM-Tools/tutorial-care-transition
“The tenth element of the PCPI quality metric set is ‘Have advanced directives been completed and a surrogate decision maker selected or a reason given for not completing an advanced care plan?’ We have reviewed SETMA’s performance on this measurement set above under ‘Care Transitions’ and ‘HEDIS.’.
“The following is a picture of SETMA’s Advance Directive template. On the Transitions of Care Quality Metric Set, if the box next to the Advance Directive element indicates that it has not been documented, in which case a red “No” appears next to the element, the provider by depressing the “update/review” button will display the Advanced Directive Detail template:
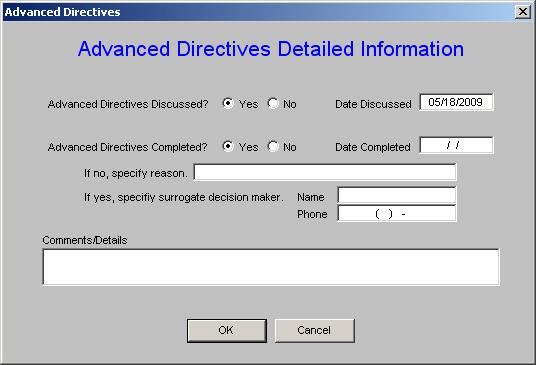
The Advanced Directive can then be addressed and the element completed.
April 4, 2008 -- http://jameslhollymd.com/Your-Life-Your-Health/Seeking-and-Finding-a-Good-Death
“Yet (seeking a good death) has not been the attitude of the past 50 years, and modern medicine may even have had the hubris to suggest implicitly, if not explicitly, that it could defeat death. If death is seen as a failure rather than as an important part of life then individuals are diverted from preparing for it. As a result, medicine does not give the attention it should to helping people die a good death.
“We need a new approach to death, and the debate of the age on older people has provided a clarion call: ‘We believe it is time to break the taboo and to take back control of an area [death] which has been medicalised, professionalised, and sanitised to such an extent that it is now alien to most people's daily lives.’
“To bring death back to the center of life would not, of course, be new. Ivan Illich traced the history of death in his critique of modern medicine, Limits to Medicine. The dance of the dead painted on a cemetery wall in Paris in 1424 showed each character dancing with his or her own death throughout life. One of the first books published by William Caxton, England's first printer, was a manual of how to die. It remained a bestseller for two centuries.
“It was not until after the Reformation that European death became macabre, and Francis Bacon was the first to suggest that doctors might hold death at bay. Earlier Arab and Jewish doctors had thought it blasphemous for doctors to attempt to interfere with death. Most people today die in the hospital, even though they say they would prefer to die at home, and a soulless death in intensive care is the most modern of deaths.
“For the American Indian, a good death addressed the nobility and the bravery associated with that death. For me, a good death would be one surrounded by loved ones and friends, celebrating the life we have shared. In the Movie, Exodus, the Jewish leader, David, stands over the crude grave of his Arab friend, Taha, and says, ‘He should have died surrounded by his people and his sons...And death should have come to him...as an old friend...offering the gift of sleep.’ The tragedy was not death, but untimely death which was intentionally caused by people filled with hatred.
“The authors of the final report on The Future of Health and Care of Older People have identified 12 principles of a good death; they are:
- To know when death is coming, and to understand what can be expected
- To be able to retain control of what happens
- To be afforded dignity and privacy
- To have control over pain relief and other symptom control
- To have choice and control over where death occurs (at home or elsewhere)
- To have access to information and expertise of whatever kind is necessary
- To have access to any spiritual or emotional support required
- To have access to hospice care in any location, not only in hospital
- To have control over who is present and who shares the end
- To be able to issue advance directives which ensure wishes are respected
- To have time to say goodbye, and control over other aspects of timing
- To be able to leave when it is time to go and not to have life prolonged pointlessly.
“Debate over whether people are dying badly or well obviously depends on a definition of a good death. It is clearly more than being free of pain, and three themes that emerged constantly in the debate of the age were control, autonomy, and independence. These are excellent principles and should be incorporated into the plans of individuals, professional codes, and the aims of institutions and whole health services.
“Dying is not the worst thing for you to do in this life. In fact, death can be a ‘healthy’ capstone to your life. As you make health care decisions for yourself or for another, make them such that you will live well for as long as you live and when it is time "to go," do so with dignity and grace, surrounding by something besides machines. And, if that is not possible, still celebrate life realizing that death is not a contradiction or a cancellation of life but an inevitable conclusion to life.”
August 16, 2006 http://jameslhollymd.com/Your-Life-Your-Health/Futile-care-law
In 2006, on a Friday afternoon, I was called by an attorney retained by a family who was protesting a hospital’s exercising a “futile care” intervention in order to end the care of their mother. I was asked if I would review the case. I was called because I am known in my community for being “pro-life.” Fifteen physicians had been involved in the patients care and the file was voluminous. I examined the patient and the next day spent eight hours reviewing the chart. I then dictated a 30-page summary of the care the patient had received. My judgment was that the patient had received excellent care but that communication had broken down between the family and physicians.
My summary stated there was one test which would be definitive in determining whether there was any possibility of the patient recovering. We did that test and I met with the family and explained the fact that their mother’s brain was dead and could not recover. They agreed to enact the Texas Natural Death Act the next day I met the family. After thanking God for their wonder mother, we turned the ventilator off. The above letter to the editor of the local newspaper was written with the consent of the family. This case had been broadly discussed in the press. The last paragraph of the letter stated:
“Whatever our position on these issues, they are serious enough that they require the careful choice of words and accurate representation of the views of those who differ with us. It is my prayer that the Conner’s family continues to find comfort in their tremendous love for their loved one. It is my prayer that none of us ever takes lightly the preciousness of life.”
I would ask ____ _____ carefully to choose his words and accurately to represent the view of those with whom he differs. Such a dialogue can bring understanding and sometimes resolution of problems. The response that I had to his presentation had nothing to do with his “passion for end-of-life” issues; it had everything to do with his mocking the position of others and amusing himself with his distortion of their views.
October 28, 2005 -- http://jameslhollymd.com/your-life-your-health/end-of-life-decisions-choices-which-make-a-difference
This article was written three weeks after I conducted the funeral service for my own father on October 9, 2005. It represents “my passion” for end-of-life mattes in the contest of my own overwhelming grief. This article states in part:
“There are three foundational principles which govern all considerations about the end-of-life decisions:
- Nothing should be done to or for a patient which would directly and intentional cause their death.
- Anything which is done to or for a patient must be legal.
- Just because there is something which can be done does not mean that it should be done.
“In my father's case, if we had chosen to put a feeding tube in his stomach and to give him artificial hydration and nutrition, he would have continued to function biologically. There is no doubt that he would be alive today. The question which we had to answer was, ‘Does this give him a quality of life which is valuable to him and is this what he would want?’ No doubt, he had established that he did not want artificial life support in the form of a ventilator, but what about hydration and nutrition?
“In my judgment, nothing must ever be done which actively results in the termination of life, i.e., no medications or other measures are to be given which results in a person's death. So called ‘assisted suicide,’ which is without doubt homicide, should remain prohibited. Yet, this prohibition of actively terminating a person's life does not mean that artificial steps and/or heroic and extraordinary measures must be taken to maintain the biological functions of a person's body.
“When The Quality of Life is Over
“I remember the moment when I realized that my father's life, as he knew and enjoyed it, was over. There was nothing I could do about that and it was no one's fault. It was a reality. For the eighteen months following that realization, my family and I walked a careful line between support of my father and not wishing to prolong his ordeal for our benefit.
“This addresses the most critical aspect of end-of-life decisions. They must be made solely and exclusively for the benefit of the person dying and not for the family. Often, in the emotional trauma of the potential loss of a loved one, decisions are made which are the result of the above mention emotions and experiences: guilt, unfinished issues, unresolved conflicts, sometimes financial reasons and a myriad of other concerns. None of these are valid foundations for good decision making about end-of-life measures.
“Cultural biases can complicate end-of-life decisions. Some cultures prepare people poorly for the death of anyone, particularly a loved one. As a result, irrational decisions are made based on maintaining the biological function of the human body no matter what the cost is to the one who is being treated. Those making the decisions about such matters must recognize that one of the mercies of life is death does not approach the elderly as a terror but as a release. As our body deteriorates, the fear of death loses its intensity and eventually the acceptance of one’s mortality allows the embracing of death to be a positive experience, particularly when surrounded by loving, supportive family and friends. To mechanically and/or heroically preserve life in the face of the inevitable is neither loving nor kind, but it can be selfish and self-centered.
“Guilt very often contributes to the complex end-of-life decisions we make for our loved ones. Whatever the basis of guilt, it is not absolved by interminably prolonging the bodily function of a loved one. Guilt is healed by forgiveness, either of others or of self. Rather than asking forgiveness or giving forgiveness, we destructively try to deal with guilt by bitterness or blame. This never works but only escalates into an emotional crisis which is self-destructive and destructive of any hope of resolution of the conflict which caused the guilt. End-of-life decisions made in the presence of guilt only perpetuate the problem.
“Unresolved conflicts can also result in making end-of-life decisions in which we try to meet our own needs rather than the needs of the one who is dying. Some how, it is often imagined that if we just keep someone alive a little longer; if we make demands upon science and medicine, that this substitutes for our having not protected and nurtured our relationship with the person who is dying. Love is sometimes interpreted as the one who shouts the loudest, or gets the angriest at those who are doing their best for our loved ones, but this never works for long.
“When my father first fell ill, I sat by his bedside and wrote about him. I thought he was going to die. I had said all that I needed to say. There were no unresolved conflicts; there was no unhealed guilt. Yet, I sat and wrote and wrote and wrote about my feelings about this wonderful man. Then I thought – and this was in a humorous moment – ‘Ah, my father’s illness must be someone’s fault. But whose?’ First, I thought, it must be his but when he became addicted to cigarettes in his youth, no one really knew of the destructiveness of tobacco. At least no one had told the public. Second, I thought, it must be my mother’s fault, but the reality is that no one could have taken better care of my father than she did all 64 years of their marriage. Third, I thought certainly my father’s terminal illness must be the doctor’s fault! Alas, my father never went to the doctor, but surely then it must have been that the doctor refused to see my father. Unfortunately, I could not blame the doctor because my father never tried to see him.
“In those quiet hours, I peacefully enjoyed the presence of my father realizing that he had lived a long, productive, honorable life. His illness was no one’s fault really. It was the natural summary of a life well spent with some mistakes, but nothing needed to rob me of the joy of having had this man as my father. My father had not consciously sought a ‘good death,’ but he had found one because of the honorable, honest, hard-working, manner in which he lived his life.
“We must all face end-of-life decisions. In reality, every day we live marches us to that moment. A man I greatly admired once said, ‘Make sure that when it comes time to die, all you have to do is die.’ That is a good death. All issues resolved; all relationships healed; all the words spoken. Idealistic? Yes! Possible? Absolutely.
“As you deal with end-of-life decisions for a loved one, do it for them, not for yourself. For more on end-of-life decision making, see the four-part series on a Living Will in the Your Life Your Health section of SETMA’s web site at www.jameslhollymd.com.”
April, 2005 -- In 2005, SETMA published a four part series on Advanced Directives. These are the links to those articles which include a sample advanced directive which patients can down load. The following are the links to those articles.
Advanced Directive Act of Texas Part IV 04/28/2005
Advanced Directive Act of Texas Part III 04/21/2005
Advanced Directive Act of Texas Part II 04/14/2005
Advanced Directive Act of Texas Part I 04/07/2005
Conclusion
SETMA has a proved passsion for end-of-life measures. In discharge over 20,000 from the hospital over the past five years, we have completed code status and advanced directives on over 93% of those pateitns. In completing over 300,000 ambulatory care viisit in the same time, we have addressed in of life issuses more than 90% of the time.
I will always object to distortions of other people’s views, as I do in this instance. While there are many things with which I disgree with President Obama, I have objected to the assertion that he has a “death squad” for he does not. If we are to have serious and helpful discussions about the serious matters we face in the transformation of healthcare, we have to have true dialogue, constructively interacting with one another’s ideas rather than having two simultaneous monoglogues without resolving anything.
James (Larry) Holly, M.D.
C.E.O. SETMA
Previous Notes
On May 31, 2013, at 1:27 PM, "_____ ______" <________> wrote:
Dr. Holly, I want to apologize to you on behalf of ____ Events. It is never our wish for any of our attendees to be made to feel alienated or uncomfortable either during the networking sessions or in the formal talks. I am very sorry to hear this was your experience at our ___ ____ Practices conference. ____ _____ is aware of your concerns both via your email and through talking to _______. I expect that he will reach out to you directly. In the meantime, please know that I take this very seriously. I appreciate you bringing the situation to our attention, as well as the other information you sent on SETMA as well as additional concerns regarding this specific event. I look forward to talking to you next week to hear more of your feedback and also to see if we can establish a working relationship for moving forward. Your feedback is very valuable to me and _____. Thank you again, and I hope you have a good rest of your day. Best, _____
_____ ______ | Director, Healthcare Products | ____ _______| ___.____ x ___
On 5/31/2013 8:53 AM, James L. Holly wrote:
On May 31, 2013, at 6:37 AM, "James L. Holly" <jholly@jameslhollymd.com> wrote:
One last issue. I wish to address the exchange ____ ______ and I had yesterday. SETMA, by provider, staff and patients is by design a muli-national, multi-ethic, multi-cultural, and multi-faith organization. We require excellence of care from all of our providers and staff. We require mutual respect and kindness from everyone as to faith, personal belief and political persuasion. We have a zero tolerance for sexual harassment, vulgarity and profanity. What a person does in their personal life is not our concern, but the cultural of SETMA is clear
We do not tolerate bigotry, prejudice or rudeness about any of these matters including sexual orientation. We are non judgmental about personal matters. I grew up in the South and have abhorred segregation and bigotry since I was a child. I am a social liberal, a theological conservative and a fiscal conservative
I and SETMA embrace and pursue the triple aim. Today I am making a 90-minute presentation to IHI by webinar. I embrace healthcare as a human right and approve the goals of the ACA although I have concerns about its fiscal impact.
Mr. _____ is talented and obviously very wealthy. His personal contempt for my Christian beliefs is irrelevant and should not be a part of a public address. His contempt for a conservative news source is irrelevant in a discussion of health policy. Even if given the chance I would not reticule his ideals. His comments added nothing to his points and were unnecessary to make them.
I probably speak and write as much as Mr. ______ and I am careful to show respect to people who hold different views. As an erudite and sophisticated person I am surprised and disappointed to hear Mr. _____ ______ use words like "shit" and "frichen" in the presence of ladies. If you don't know what this word derives from, look it up. It is one of the most offensive and vulgar words on the English language. If Mr. _____ _____'s company approves and encourages this language, that is his business, but I hope ____ does not.
I accepted Mr. _____s apology yesterday but did not appreciate the continued humor and ridicule at my expense. As an optimist, I am hopeful for a better day today.
James (Larry) Holly, M.D.
On May 31, 2013, at 5:57 AM, "James L. Holly" <jholly@jameslhollymd.com>wrote:
For your interest our public reporting by provider name. http://jameslhollymd.com/public-reporting/public-reports-by-type
James (Larry) Holly, M.D.
-----Original Message-----
From: James L. Holly Sent: Friday, May 31, 2013 4:27 AM
To: _____ ________; ____ Events; ______ _______; ________@__________.org; ____ _____ ______ ; _______ _____; ______.______@___________.com, _____ ______
Cc: Theresa Bailey; Jonathan W. Owens
Subject: Dr James Holly - SETMA and IMO on Vimeo
This video is a spontaneous, unrehearsed, unscripted discussion done on a cell phone on the exhibit floor at HIMSS 2013 in New Orleans. It addresses Chronic Problem List and HCC Risk. The first day of this ____ event gave details and often glib descriptions of the problems we face, but not information on solutions. In addition to the below short video, you will receive a link to SETMA's HCC Tutorial and a link to out tutorial for how to maintain a complete, up-to-date, accurate chronic problem list.
http://jameslhollymd.com/in-the-news/robert-wood-johnson-foundations-transitions-to-better-care-video-contest James (Larry) Holly, M.D.
-----Original Message-----
From: James L. Holly Sent: Friday, May 31, 2013 4:38 AM<
To: _____ ________; ____ Events; ______ _______; ________@__________.org; ____ _____ ______ ; _______ _____; ______.______@___________.com, _____ ______
Cc: Theresa Bailey; Jonathan W. Owens
Subject: SETMA.com | EPM Tools | Problem List Reconciliation
This work is the result of a question addressed to SETMA about the difficulty a Medical School faculty was having in maintaining an accurate, up-to-date, and complete Chronic Problem List. Along with an accurate and complete, Reconciled Medication List, these represent the two most difficult problems facing health care providers. In SETMA's Transitions of Care solution, our patients receive four medication reconciliations for each hospital admission and discharge. 6878 discharges in the past 48 months: http://jameslhollymd.com/epm-tools/problem-list-reconciliation-tutorial James (Larry) Holly, M.D.
-----Original Message-----
From: James L. Holly Sent: Friday, May 31, 2013 4:55 AM
To: _____ ________; ____ Events; ______ _______; ________@__________.org; ____ _____ ______ ; _______ _____; ______.______@___________.com, _____ ______
Cc: Theresa Bailey; Jonathan W. Owens
Subject: SETMA.com | EPM Tools | HCC/RxHCC Risk Tutorial
This HCC Tutorial describes SETMA solution to maximizing the clinical and economic benefit from the risk stratification of all patients seen at SETMA: http://jameslhollymd.com/epm-tools/Tutorial-HCC-RxHCC-Risk. In 207, our first major effort at HCC reporting, SETMA reported 29,689 HCC/RxHCC diagnoses. CMS rejected 51 of them. One of the most interesting things we do is contrasting E&M Code means with HCC coefficient aggregate scores for acute diagnoses on each patient encounter. We compare those results for Medicare Advantage, Fee-for Service Medicare and for all payers.
In 2011 CMS engaged RTI International to contrast 312 Medical Home Practices with 313 non coordinated practices. They compared total cost, quality performance and coordination. SETMA's total cost was 37.4% below the benchmarked practice. That study is posted on our website The Robert Wood Johnson Foundation is currently doing a three year study on SETMA. We have been involved in Medicare Advantage and its predecessors since 1996. We are participating in a federally qualified ACO and we are. Tier Three Medical Home and are currently submitting our application for re-recognition by N CAA and AAAHC.
James (Larry) Holly, M.D.
|