|
On September 20, 201, SETMA’s provider training session focused on MACRA which is the acronym for the Medicare Access and CHIP Reauthorization Act of 2015 and MIPS, the acronym for the Merit-Based Incentive Payment System. MIPS is the new payment system which will be instituted in 2019 based on data reported in 2017, and it will be based on a healthcare provider “composite performance score” (CPS). This score will be made up of the following percentages in the first year:
- Quality (50%) - This is an extension of the Physician Quality Reporting System (PQRS0 which began as a required function in 2011, PQRS was an extension of the Physician Quality Reporting Initiative (PQRI) which began in 2006 and was voluntary. SETMA began participating in 2007 and has participated in PQRS since 2011. From 2009 through the present SETMA has publicly reported on over 250 quality metrics by provider name.
- Resource use (10%) - This is a cost measurement based on the total cost of a provider or a practice’s resources spent in taking care of fee-for-service Medicare. Later, I address SETMA’s resource utilization. Our only outliers are in Post Acute Care and Hospice. In all other areas our costs are significantly below the mean.,
- Advanced care information (25%), and - This is the new name for “meaningful use.”
- Clinical practice improvement activity (15%). - This is patient-centered medical home. A practice, like SETMA that has a Tier III recognition by NCQA is automatically awarded these points. SETMA recognition by NCQA began in 2010 and extends through 2019.
It is expected that when this program is fully phased in, that at some point currently undefined, each of the four categories will be valued at 25% of the whole. The penalty or bonus or no-change in payments will begin in 2019 based on data from 2017.
In our review, SETMA providers were pleased to know that the things we began twenty years ago are now providing benefits to our patients, practice and providers:
- Electronic Medical Records (EMR) and Electronic Patient Management (EPM),1998, which prepared us to qualify for Meaning Use I and II and now for the Advanced Care Information model of MIPS.
- Quality Reporting which we began in 1999 and which was changed to “public reporting by provider name” in 2009. A potential weakness of PQRS which SETMA recognized before the system was defined, was that it could also be used to encourage cookie-cutter treatment, a potential consequence that every healthcare facility must overcome. If the system is poorly used, it can make previously careful doctors put data extraction and expected protocols over patient well being. This doesn't happen because the system itself is defunct, but rather because PQRS is not used in a patient-centric way. To avoid this weakness, in 1999, SETMA developed a “Quality Metrics Philosophy” which included these assumptions:
- Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care. Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare “Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there.
- The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and patient-population data.
- There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- The collection of quality metrics should be incidental to the care patients are receiving and should not be the object of care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
- Clinical practice improvement activity - SETMA began the process of preparing for Patient-Centered Medical Home (PC-MH) in 1999. Ten years later, SETMA achieve its first PC-MH recognition from NCQA, followed by AAAHC, URAC and the Joint Commission. At times the time, energy and resource commitment to quality, meaningful use and medical home was questioned. Now, with MACRA and MIPS facing all of us, SETMA’s development appears prescient.
- The Use of Resources or cost is further evidence of the value of SETMA’s development. When it is seen that the only challenges to SETMA utilization are areas which benefit patients and not providers, it is seen that our model really works.
We were able to share celebration and self-congratulations for having made such excellent preparation for MACRA and MIPS. To understand the complexity and the anxiety of this new program review the following formula by which a providers CPS will be calculated by CMS with the following eight factors:
CPS = [(quality performance category score x quality performance category weight) + (resource use performance category score x resource use performance category weight) + (CPIA performance category score x CPIA performance category weight) + (advancing care information performance category score x advancing care information performance category weight)] x 100.
Quality - 50% MIPS which will evolve from PQRS
For the 2015 PQRS, SETMA was required to report on 9 PQRS measures. The 2015 data by provider with SETMA’s totals and the totals for all users of NextGen EMR is posted elsewhere on our website. Any result which is below 90% is posted in red meaning that it needs to be improved. Plans are in place for how to improve this performance in 2016 and 2017, in preparation for the MIPS Payments in 2019. When MIPS is instituted in 2017, we will be required to report on six measures.
Here is another element of quality which comes from hospital data:
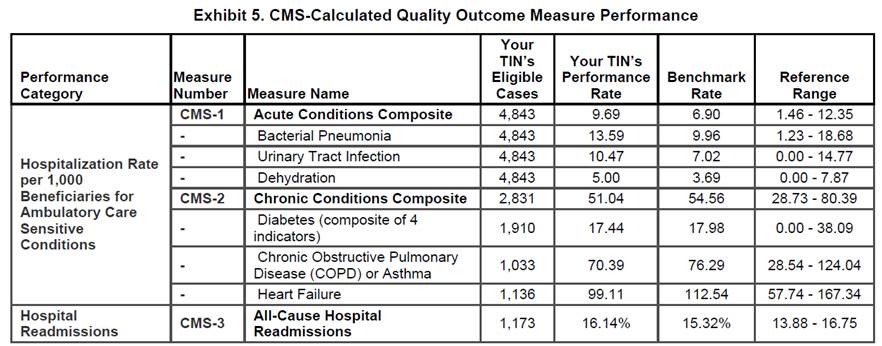
The three acute condition outcomes measures are related to patients who have pneumonia, UTI and dehydration. SETMA has a very high number of nursing home patients. While our numbers are still within one standard deviation, we have designed ways to improve these numbers. Our Chronic Conditions measures are very good (Diabetes, COPD and CHF).
Resources Utilization - Cost - 10%
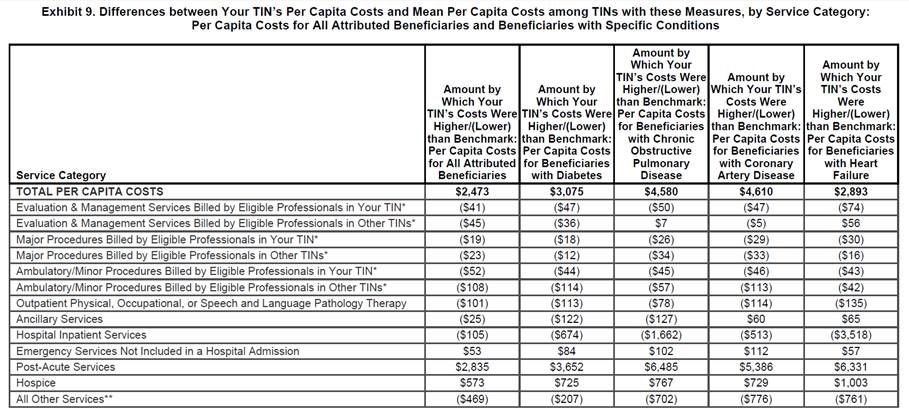
The services where SETMA’s costs are higher are “Post Acute Care,” which are:
- Home Health
- LTAC
- In-Patient Rehabilitation
- Skilled Nursing
The good news is that these are not areas where physicians are increasing costs for their own financial benefit but all are for the benefit of the patient. We are discussing ways in which we can decrease these costs without compromising patient safety and quality of care.
There are only two other areas in which SETMA’s cost are higher:
- Emergency Room Care -- SETMA has a plan for decreasing ER utilization in order to improve that metric in our cost mix.
- Hospice - Several SETMA providers have a passive financial interest in a hospice. All SETMA hospice candidates are given their choice such that almost 50% of our patients choose another hospice other than the one our providers work with. Second, CMS calculates a “Cap Rate” for each hospice. Hospices which are possibly “over utilizing” services will have a high “Cap Rate.” Hospices which are not “over utilizing” will have a low “Cap Rate.” The hospice in which any SETMA provider has a passive interest has a “Cap Rate” which is more than $1,000,000 below what is expected. This means that this hospice provides services at a lower cost than expected.
In all other areas, SETMA costs are below the benchmark. With some attention to Post Acute Care and to ER utilization, we believe that by 2017, we can move SETMA into a lower cost category.
The above data is for half of 2015. The following data is based on completed data from 2014:
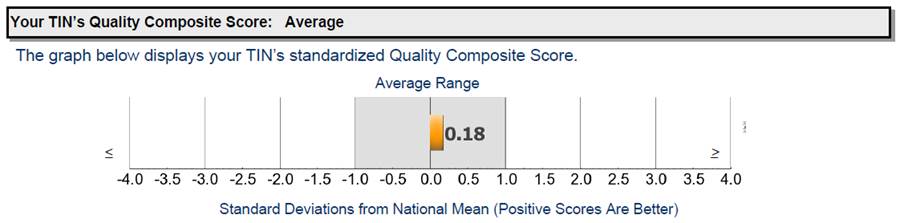
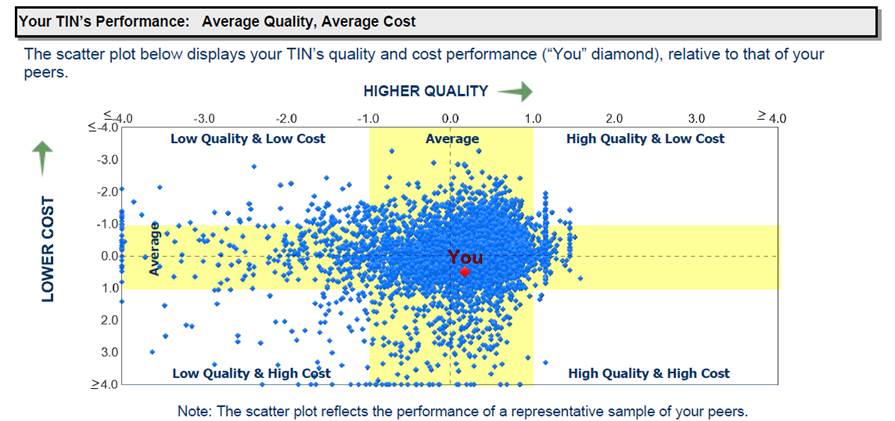
For Quality, a high score is good. SETMA is 0.18 standard deviations above the mean for quality. We think 2015, 2016 and 2017 will be significantly higher than this.
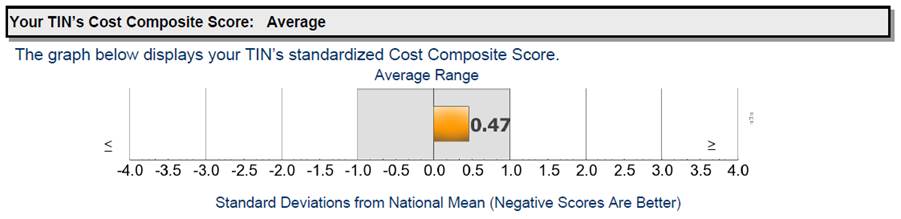
For Cost, SETMA is 0.48 standard deviation above the mean in which case lower is better. We believe that in 2015, 2016 and 2017 our costs will improve which means that they will go down.
The following “scatter plot” gives a visual of where SETMA is for 2014 data. No one wants to be in the left lower quadrant and everyone would like to be in the right upper quadrant. SETMA’s goal for the next three years will be to improve our quality and to decrease our cost.
With this data and with these considerations and others not included in this review, and with SETMA meeting Meaningful Use and PC-MH standards, and with our quality improvement effort over the next several years, we should be well positioned to continue providing excellent care to our patients and to benefit from the new payment model defined in MACRA and MIPS.
|