|
Overview and the Philosophical Underpinnings to
SETMA’s Website (www.jameslhollymd.com) which is SETMA’s “Offer”
to the Center for Medicare and Medicaid Services’ (CMS)
Transforming Clinic Practice Initiative (TCPI)
By James L. Holly, MD
Index
On May 21, 2015 Medical Home News submitted a series of questions to SETMA (see http://jameslhollymd.com/Letters/medical-home-news-questions-for-catching-up-with-dr-james-l-holly). The six questions asked were:
- You have an extraordinary passion for your practice, your patients, and you pursuit of excellence. Where does that passion come from?
- You built your own Electronic Health Record system at SETMA. Why did you feel the need to do that?
- Your Community Council gives your patients a very strong voice in SETMA governance and operations. Were any of your staff or doctors worried about that when you first set it up?
- You and your team have successfully earned recognition/accreditation already from AAAHC, NCQA, The Joint Commission, and URAC -- which is a lot of work -- and you’re now looking at Planetree. Anybody there getting “accreditation fatigue”?
- What advice do you have for practices that want to begin (and continue) the transformation journey to become a patient-centered medical home?
- Finally, tell us something about yourself that few people would know.
As you read the following, which is my answer to question one above, and as you recognize that this answer derives from my personal story, you should substitute your words and your story for mine. While this introduction to the intent and dynamic of the TCPI is based on my experience, its ultimate value will be as it provokes you to share your story within your own practice, community and within the TCPI community.
There is an old adage which states, “It’s my way or the highway,” TCPI modifies that to say, “This is our highway; it is an example from which you can build your personal highway.” The building of that highway requires that you be willing to face where you are and who you are, as you envision where and what you want to become. It is founded upon the implications of Abraham Lincoln’s 1858 declaration: “If we can first know where we are and whither we are tending; we can better judge what to do and how to do it.”
My father did not go to college but started work as a laborer with Louisiana Power & Light Company. In 1947, when I was four, we moved to a company house at Camp Livingston, a decommissioned, military base outside of Ball, Louisiana. Our family of four shared a two-bedroom house with another family. My father traveled to Monroe every Monday morning and returned Friday night. Within a year, he ran the power station at Camp Livingston and we moved to Natchitoches where he ran the power company’s interests over a large part of north Louisiana including Camp Polk which would become Fort Polk. Graduate engineers were sent to him for training. I watched his self-sustaining energy and drive, and his commitment to excellence without supervision and without guidance. I saw rich, educated and powerful men defer to my father because of his character and personal integrity. I learned.
Years later, while riding down an unpaved, country road, my father stopped and hailed a man plowing in the field. The man walked over and my father said, “I thought you were going to be by the house last Friday?” The man responded, “One of the kids got sick but I’ll be there this week.” As we drove on, I asked my father what that was about. He said, “He couldn’t pay his light bill and I paid it for him.” This was Louisiana, my father was Caucasian and his friend was African-American. I learned. He would never let children go without heat and power. Although he made less than $5,000 a year, he was never without money to help others.
As my social liberalism grew, my father expressed concern. He had lived a life of compassion and kindness to others, but had never opposed his culture. I started aggressively opposing that culture when I was 17. I responded to my father’s concern and said, “Daddy, everything I believe and everything I do, I learned from you.” As my personal faith grew, it only reinforced the lessons I had learned from my father until I would define myself as “a social liberal, a fiscal conservative and a theological fundamentalist. “ My father is deceased, but I still live with a desire to be like him, to be a man of integrity, honor, compassion, and fearlessness.
The other great influence on and driver of my life is the overwhelming gratitude which I feel for the honor of being a physician. (for more on this concept, see: http://jameslhollymd.com/Your-Life-Your-Health/pdfs/Memories-on-the-Auditorium-Dedication.pdf, http://jameslhollymd.com/In-The-News/pdfs/mission-magazine-a-call-to-heal-a-call-to-serve.pdf, http://jameslhollymd.com/Your-Life-Your-Health/pdfs/the-honor-of-being-a-physician.pdf. Forty-three years later, I still stand in awe of having the privilege of being a physician. As I watched and re-watch the movie Secretariat, I am moved almost to tears at the portrayal of his running of the Belmont Stakes in 1973, the same year I graduated from medical school. After the first half of the race, he was no longer running to win. He was running for the sheer joy of running.
Like Mikhail Baryshnikov, the great Russian ballet star, Secretariat is competing only with himself and his achievement was breathtaking. When he crossed the finish line and the race was over, he was still running as no one believed a horse could. Secretariat had done something which had never been done before and which has never been done since. I am drawn to this race as I have come to the point in my life when I am working for the sheer joy of my work. I have frequently said, “I have a passion for which I am owed no credit and over which I have no control as it is a gift from God.” Whatever your personal belief system, the principle can apply.
In the movie, Saving Private Ryan, Ryan, now in his seventies, approached the headstone of Captain John Miller who gave his life that Ryan could live. In the most poignant moment in a great film, tears stream down his face, as he crumpled before Miller’s tombstone, as Ryan plaintively said to his wife, "Tell me that I have lived a good life; tell me that I have been a good man." The sacrifice of others, imposed upon Private Ryan a debt only a noble and honorable life could repay. My debt and yours did not originate so dramatically, but it still exists.
There are few gifts as great as that of the opportunity to be a physician. The trust of caring for others has always been a sacred trust. It is a trust which should cause each person so honored to tremble with fear that he/she will not have lived worthily of that trust. It should cause us to examine our lives for evidence that we have been good stewards of the treasure of knowledge, skill, experience, and judgment which has been bequeathed to us by our university, our professors and the public which funded our education.
What nobler calling could one have than the opportunity to collaborate with others in their quest for health and hope? The honor of the trust and of the respect given by strangers, who share their deepest secrets, knowing they will be held sacrosanct, is a gift which exceeds any pecuniary advantage. The pursuit of excellence in the care of others is a passion which is self-motivating.
Passion is the fuel which energizes any noble endeavor. It is what makes a person get up early in the morning, work hard all day, and go to bed late at night looking forward to the next day. It is a cause of great sadness that today's society is so devoid of true purpose-driven passion. Many only vicariously experience passion through the eyes and lives of athletes, movie stars, or musicians. Ultimately, passion and purpose are what make life worth living. Those of us, who have been allowed the privilege of being physicians, can and should know the passion of a noble purpose every day of our lives.
Historically, governmental efforts to “change things” were associated with “rule making.” The desired change was mandated by regulations, and requirements, which were audited and enforced with penalties. While there is a place and even a need for standardization to promote and document change, and while there is a need to create accountability and to expose fraud and abuse, mandated change typically has been only modestly successful in producing excellence. Being motivated only by external pressure, which can reshape things over a short period of time, reform ultimately cannot sustain change and certainly has no generative power through which to create actively transformative change.
Inevitability, when pressure was decreased, or when the organization became indifferent to pressure, it resumed its original shape and structure. Through the elastic ability to mimic change, organizations have successfully resisted radical transformation judged by essential and inherent alterations in nature, dynamic and results. The organization’s inherent elasticity resists permanent and self-sustaining change. When pressure is decreased, the organization resumes its former shape and nature. Without increasingly greater pressure and/or reward, reform fails.
TCPI is building on a different foundation and with a different dynamic than external pressure. Unlike the past, the Centers for Medicare and Medicaid Services (CMS) rather than mandating change, wants to become your partner, your colleague, your consultant. Rather than “telling you what to do,” with support and facilitation from the Practice Transformation Networks (PTNs), the Support and Alignment Networks (SANs) and in collaboration with the existing State Quality Improvement Organizations (QIOs), CMS wishes to empower and encourage your personal passion, vision and generative energy to create a future of your design, which will be sustained by the internal drive of your ideal of the future you wish to create.
In this way, as CMS is working to encourage and to enable your transformation, CMS is itself transforming its interaction with healthcare providers. While CMS will continue to exercise its fiduciary responsibility to the public it serves, which requires auditing and enforcement activities, there will be a changing culture of collaboration with healthcare providers where CMS and healthcare providers recognize, acknowledge and cooperatively pursue their shared commitment to safety, quality and excellence in healthcare. It is almost as if CMS and healthcare providers have challenged themselves to adopt the principles of patient-centered medical home: activation, engagement and shared decisions making.
CMS is not the only organization which has and is facing the challenge of transforming itself as it promotes transformation in healthcare providers. Every accreditation agency which SETMA has invited to critique our performance has also been challenged to examine itself. In response to one accreditation experience, SETMA wrote the executives and said:
“SETMA has always taught that a test, a patient encounter, an accreditation visit, or any human interaction should be evaluation-al and educational for both parties. That means that both parties should be learning, and learning has only taken place when we make changes and sustain those changes.
“Peter Senge’s use of the term ‘learning organization’ in his book The Fifth Discipline, promotes organizational change that is a critical aspect of the dialectic of human interaction. Although we finished our accreditation site visit on a positive note - and successfully so as we had partial deficiencies in only 16 of over 1200 measures€¦- the hubris of the evaluators was obvious.
“Their attitude was that they had nothing to learn but were here only to critique and indeed to criticize as was demonstrated by their initial statement upon their arrival, in which they said, ‘If you are doing anything wrong, we will find it.’ This attitude was confirmed by their statement that it is a corporate policy never to say anything positive about an organization they are evaluating but only to point out the negative. The stated issue was that any positive response would diminish the imperative of making changes which were needed.
“SETMA’s philosophy is exactly the opposite. We believe that affirmation is the foundation of constructive observations and recommendations for change. And, affirmation actively empowers others to change.”
It is because of this philosophy that SETMA is willing to take the risk and to subject ourselves to the scrutiny of the highest standards. We are prepared to be transparent and to publish by provider name our performance on hundreds of quality metrics. This transparency drives our improvement. It allows SETMA to be the best we can be. It allows us to declare: Once you “open your books on performance” to public scrutiny; the only place you have in which to hide is excellence!
As you, among the 140,000 healthcare providers CMS hopes to engage in TCPI, experience the role of the PTNs, the SANs and CMS itself, you will begin to see that this is a new undertaking, a new day and a new CMS which wants you to succeed, which believes that you want to change and that you will succeed, and a CMS whose goal is to help you succeed in transforming your practice to achieve your vision and goals.
It is as the gratitude you feel toward those who have contributed to your success drives you, and as you begin to experience the sheer joy and delight of your work and efforts, like Secretariat, your current reality inextricably moves toward your vision, driven by your passion. Just as in a patient-centric environment, the patient is activated and engaged by shared-decision making, you are moved forward by your participation in transforming your practice to fulfill the future you envision. You work hard and you succeed because you are implementing YOUR ideals and you are experiencing the logical implications of YOUR personal story.
In The Fifth Discipline, Senge, addresses the importance of “creative tension.” He calls this the “spirit of the learning organization in which participants have ’personal mastery’ (which) goes beyond competence and skills, though it is grounded in (them). It goes beyond spiritual unfolding€¦although it requires spiritual growth. It means approaching one’s life as a creative work, living life from a creative as opposed to a reactive viewpoint.”
When personal master is integrated into our lives, it becomes a discipline and embodies two activities:
- “The first is continually clarifying what is important to us.
- “The second is continually learning how to see current reality more clearly.”
Senge concludes, “The juxtaposition of vision (what we want) and a clear picture of current reality (where we are relative to what we want) generates what we call ‘creative tension’: a force to bring reality and vision together, caused by the natural tendency of tension to seek resolution. The essence of personal mastery is learning how to generate and sustain creative tension in our lives.”
As the TCPI promotes clinical practice transformation, that transformation will be sustained by providers developing personal mastery in which they will share the following characteristics:
- “They have a special sense of purpose that lies behind their vision and goals. For such a person, a vision is a calling rather than simply a good idea.
- “They see current reality as an ally, not an enemy. They have learned how to perceive and work with forces of change rather than resist those forces.
- “They are deeply inquisitive, committed to continually seeing reality more and more accurately.
- “They feel connected to others and to life itself.
- “Yet, they sacrifice none of their uniqueness.
- “They feel as if they are part of a larger creative process, which they can influence but cannot unilaterally control.
- “Live in a continual learning mode.
- “They never ARRIVE!
- “(They) are acutely aware of their ignorance, their incompetence, their growth areas.
- “And they are deeply self-confident!”
“Personal Mastery is not something you possess, it is a process.” As we clarify our vision and as we face our current reality, we will be driven to transformation. While there will be objective standards and while there will be measurable outcomes which are promoted, the dynamic of TCPI will be internalized and will become a personally driven passion.
Part of the transformation hoped for in TCPI, is for practices to embrace and invest in team work. Before SETMA understood that Twenty-First Century medicine could not be practiced with “pencil and paper” (19th Century Medical Record Methodology), or even with “dictation and transcription” (20th Century Medical Record Methodology), both of which drove SETMA to Electronic Medical Records in 1998, SETMA understood that the demands of 21st Century medicine would require a team approach to healthcare delivery. Eventually, we would recognize that team work is not just an ideal of healthcare transformation; it is an imperative. And, that imperative grows out of the necessity of multiple people working in collaboration with patients and families in order to provide the quality and safety which 21st Century healthcare demands.
In the same way CMS and TCPI will be part of the team, promoting, driving and participating as a part of the healthcare team.
The principles of “team care” have been repeated and refined but they have been part of the organizational spirit of SETMA from the beginning. That team led us to a significant examination of the value of each member of the team and to their contribution to SETMA’s model of care. Without this team concept and reality, SETMA would not be where it is today. It also became apparent that a team approach to healthcare delivery, once embraced and executed, would inextricable require and lead to a Medical Home dynamic and structure of healthcare delivery.
In order to create great teams, the educational process has to change: see http://jameslhollymd.com/Your-Life-Your-Health/Medical-Home-Part-V-Healthcare-education-and-healthcare-Delivery-Changes-needed-in-both. The ideal setting in which to deliver and to receive healthcare is one in which all healthcare providers value the participation by all other members of the healthcare-delivery team. In fact, that is the imperative of PC-MH. Without an active team, with team consciousness and team collegiality, PC-MH is just a name which is imposed upon the current means of caring for the needs of others. And, as we have seen in the past, the lack of a team approach at every level and in every department of medicine creates inefficiency, increased cost, potential for errors and that it actually eviscerates the potential strength of the healthcare system.
Why is this? Typically, it is because healthcare providers in one discipline are trained in isolation from healthcare providers of a different discipline. Oh, they are in the same buildings and often are seeing the same patients, but they rarely interact. And, often they have little respect for one another and do not see themselves as collaborators but as isolated “collatoralists,” often working side-by-side but not interactively. Often, even their documentation is done in compartmentalized paper records, which are rarely reviewed by anyone but members of their own discipline. This is where the first benefit of technology can help resolve some of this dysfunction. Electronic health records (EHR), or electronic medical records (EMR) help because everyone uses a common data base which is being built by every other member of the team regardless of discipline. While the use of EMR is not universal in academic medical centers, the growth of its use will enable the design and function of records to be more interactive between the various schools of the academic center.
And, why is that important? Principally, because more and more healthcare professionals are discovering that while their training often isolates them from other healthcare professionals, the science of their disciplines is crying for integration and communication. For instance, there was a time when physicians rarely gave much attention to the dental care of their patients, unless they had the most egregious deterioration of teeth. Today, however, in a growing number of clinical situations, such as the care of diabetes, physicians are inquiring as to whether the patient is receiving routine dental care as evidence-based medicine is indicating that the control of disease and the well-being of patients with diabetes are improved by routine dental care. Also, as the science of medicine is proving that more and more heart disease may have an infectious component, or even causation, the avoidance of gingivitis and periodontal disease have become of concern to physicians as well as dentist.
In addition, Medical Home places major emphasis upon issues which historically have been the concern of nurses. Physicians who use EMRs are discovering that the contribution of nursing staff can make the difference in the excellent and efficient use of this documentation and healthcare-delivery method. No longer is the nurse a "medical-office assistant" ancillary to the care of patients, but the nurse is a healthcare colleague central and essential to the patient's healthcare experience. As evidence-based medicine expands the scope of what The Innovator's Prescription: A Disruptive Solution for Health Care By Clayton M. Christensen labels as "empirical medicine," which ultimately leads to "precise medicine," it is possible for physicians and nurses to be a true-healthcare delivery team, as opposed to the nurses only being an aide to the physician.
Christensen identifies the following "Levels of medicine" and makes the following judgments about the future of healthcare delivery:
- Intuitive Medicine -- "When precise diagnoses isn't possible...where highly trained and expensive professionals solve medical problems through intuitive experimentation and pattern recognition."
- Empirical Medicine -- "As patterns become clearer, care evolves into the realm of evidence-based medicine...where data are amassed to show that certain ways of treating patients are, on average, better than others."
- Precise medicine -- "When diseases are diagnosed precisely...therapy that is predictably effective ... (can) be developed and standardized."
- “... (When) we know what type of bacterium, virus, or parasite causes one of these disease..."
- “... (When) we know the mechanism by which the infection propagates..."
- "...Predictably effective therapies can be developed..."
- "...Therapies that address the cause, not just the symptoms..."
As a result, Christensen concludes:
- "...nurses can now provide care for many infectious diseases..."
- "...patients with these diseases only rarely require hospitalizations."
It is easily recognized in this emerging paradigm that all of the schools in the academic healthcare center are actively involved in patient care and in the training of those who will be healthcare providers. Yet, it seems that the farther and farther a person advances in biomedical education, the obvious union of their disciplines at their foundations is lost and the more isolated from the whole these "specialists" and “experts" become.
This even creates problems within the various disciplines as egocentrism isolates one provider from another. It is as a result of the need for the integration of healthcare disciplines at the delivery level, that we recognize the imperative for the restructuring of the training of the members of this healthcare team. And, the first change must come in the relationships between the leaders of the training programs who educate and mentor future healthcare scientist, teachers, caregivers and researchers. The educational leaders must model this integration for their disparate student bodies and that modeling will require the investment of the most precious and rare resource: time. This is not the law of the land but it will be in the future. (For more on this see the discussion at the following link: http://jameslhollymd.com/Letters/an-open-letter-to-the-medical-executive-committees-of-baptist-southeast-texas-hospital-and-christus-st-elizabeth-hospital; and at: http://jameslhollymd.com/Letters/comments-to-the-christus-medical-executive-committee-about-inpatient-healthcare-teams; and at http://jameslhollymd.com/Letters/value-and-power-of-the-healthcare-team-answering-dr-amy-townsends-imperative)
Again, it is not only you, the healthcare provider seeking transformation which must change, CMS will be required to re-examine its definitions of healthcare and its descriptions of the scope of practice of various members of the healthcare team.
What is the model for this restructuring of the relationships between schools in the academic healthcare centers? It has been suggested that there is "glue" which unites the members of the various schools which will ultimately create this team. I would argue with that. Glue is an adherent. In this context, "adherence" is described and simultaneously defined by the following: "Two dissimilar parts touching each other but not fused." "The union of separate parts; tending to adhere to or be connected by contact." If propinquity -- the state of being close to someone-- is the principle motivation for the forming of a team, it will not survive the stresses and pressures which tend to make the team fly apart.
On the other hand, "cohesion" is "the bonding together of members of an organization/unit in such a way as to sustain their will and commitment to each other, their unit, and the mission," and it has been further defined as a "union between similar plant parts or organs." Synonyms of "cohesion" are "harmony, agreement, rationality." Here is the source of the union of the various elements of the healthcare team in training. It is in the recognition of their commonness and in the acknowledgment of their being part of the same "organism."
The concept of "harmony" is valuable here also. Harmony is not the absence of discord; it is the presence of a common nature. The typical definition for a harmonic is "a sinusoidal component of a periodic wave or quantity having a frequency that is an integral multiple of the fundamental frequency." I smiled and chuckled aloud as I wrote this last sentence. It is a mouthful, but how is it related to our problem of healthcare delivery? If you have a room filled with tuning forks of different frequency and you strike one of the forks, all of the forks which are of the same frequency or a multiple of the same frequency, as the one struck, will begin to sound. Those which are intrinsically different will remain silent.
In a room of educators, some health science, some historians, some vocalists, some archeologists, etc., when the sounding is of excellence in healthcare delivery; when the sounding is of evidence-based medicine; when the sounding is of containing the cost of healthcare while maintaining the quality; when the sounding is of increasing the accessibility of healthcare by removing barriers of affordability, linguistics, literacy, etc; each member of the healthcare-education team, whether nurse, dentist, physician, scientist, physical therapist, laboratory technician or other, will begin to resonate, as they are all coherent, by their nature, to the process of sustained improvement in the delivery of healthcare. It is as if the healthcare-education team, as the healthcare-delivery team, has become a symphonic orchestra made up of instruments which are different in sounding method but which harmonize to produce an aesthetically satisfying result. Remember, the Greek word "symphonia" means "sounding together." So it is that the members of the healthcare-education and the healthcare-delivery team "resonate together" to produce the results we all desire.
My personal pilgrimage in this process began my first year in medical school, but it was not in the class room. One day, as I was leaving the medical school with a classmate, the Dean's secretary ran up to us and said, "Larry, you must go downstairs. There is a meeting for the new health careers program and the Dean is there by himself." Reluctantly, I went and began a two-year participation in the School of Medicine's Health Careers Program and a life-time of desire to help young people pursue health careers. Every Saturday, we brought high school students, principally Hispanics, to the school of medicine and introduced them to health careers. I realized then that the recruitment of a diverse student body to the various elements of the health science center was not going to be done en masse but it was going to be done one student at a time. As a result, one of the missions of the SETMA Foundation is to help underwrite the education costs for students who qualify but cannot afford health-career education.
The second element to my pilgrimage was in Clifton, Texas, after graduation from Medical School. With the birth of my second child days before graduation and with him in neonatal ICU, I had to work in order to provide for my family. Monday after graduating on Saturday, I left for Clifton. I lived in the hospital around the clock with two days off in a month to take the state medical boards. I learned the value of a healthcare team from an LVN when one night, as I was preparing to treat a patient in the ER, she said, "I have noticed that our doctors do that this way." She was so kind. She didn't say, "Hey, stupid, didn't you learn anything in medical school?" Yet, over the next four weeks, my wealth of knowledge of physiology, pathophysiology, biochemistry, heart failure, etc., was augmented by a wealth of practical medicine taught to me by an LVN. What doctor cannot remember the same kind of experience with a nurse, or other healthcare team member who helped him/her through a patient encounter which was new? Why have we forgotten?
The third element of my pilgrimage was SETMA's migration to EMR. When SETMA was formed there was no uniformity in how medical records were created, filed or stored. Some dictated records, others hand wrote records. Some organized records alphabetically, others used a numeric system. On August 1, 1995, SETMA's medical-record-keeping illustrated all of the problems facing the future of healthcare in America. With the new millennium approaching, with all of the potential of 21st-Century technological care, SETMA was hamstrung by the use of mixture of a 19th -Century documentation system, i.e., pencil and paper, and a 20th-Century system, i.e., dictation and transcription. Neither system was capable of supporting innovation in healthcare delivery. In March of 1998, we purchased an EMR system.
As TCPI progresses, your passion and your team’s work will be conducted electronically. In May, 1999, SETMA’s transformation process was radically changed as four seminal events took place. (For a full description of those events see: http://jameslhollymd.com/your-life-your-health/may-1999-four-seminal-events-in-setmas-history.)
The first event took place the first week of May, 1999, when SETMA’s CEO announced that the EHR was too hard and too expensive if all we gained was the ability to document a patient encounter electronically. When we began, it took a provider five minutes to create a chart note. Our CEO concluded EHR was only “worth it,” if we leveraged electronics to improve care for each patient; to eliminate errors which were dangerous to the health of our patients; and, if we could develop electronic functionalities for improving the health and the care of our patients and of population groups. This was our transition from EMR to electronic patient management (EPM).
We also recognized that healthcare costs were out of control and that EPM could help decrease that cost while improving care. Therefore, we began designing disease-management and population-health tools, which included “follow-up documents,” allowing SETMA providers to summarize patients’ healthcare goals with personalized steps of action through which to meet those goals. We transformed our vision from how many x-rays and lab tests were done and how many patients were seen, to measurable standards of excellence of care and to actions for the reducing of the cost of care. We learned that excellence and expensive are not synonyms. In ten years, these steps would lead us to begin public reporting by provider name on over three hundred quality metrics (http://jameslhollymd.com/public-reporting/public-reports-by-type).
The second event was that from Senge’s The Fifth Discipline, SETMA defined the principles which guided our development of an EHR and which defined the steps of SETMA’s transformation from an electronic medical records (EMR) to electronic patient management (EPM). (see: http://jameslhollymd.com/EPM-Tools/pdfs/designing-an-emr.pdf). These principles would also be the foundation of SETMA’s morphing into a patient-centered medical home (PC-MH) in 2009. The principles were to:
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to every patient encounter what is known, not what a particular provider knows
- Make it easier to do “it” right than not to do it at all
- Continually challenge providers to improve their performance
- Infuse new knowledge and decision-making tools throughout an organization instantly
- Promote continuity of care with patient education, information and plans of care
- Enlist patients as partners and collaborators in their own health improvement
- Evaluate the care of patients and populations of patients longitudinally
- Audit provider performance based on endorsed quality measurement sets
- Integrate electronic tools in an intuitive fashion giving patients the benefit of expert knowledge about specific conditions
In 2009, we would discover that these principles are essentially the principles of PC-MH and that the past ten years had prepared SETMA to formally become a PC-MH. Between 2009 and 2014, SETMA became accredited as a medical home by NCQA, AAAHC, URAC and The Joint Commission.
The third seminal event was the preparation of a philosophical base for our future; written in May, 1999 and published in booklet form in October, 1999, this blueprint was entitled, More Than a Transcription Service: Revolutionizing the Practice of Medicine With Electronic Health Records which Evolves into Electronic Patient Management”. This booklet was distributed to our practice and our community. It became our declaration that we were going to succeed at this process at any cost and at any effort. Like Cortez, who scuttled his ships on his expedition to Mexico so that there was no turning back, this booklet was SETMA’s public declaration that there was no going back. We were going to succeed. Our charge to ourselves was and our counsel to others is, “Don't give up!” The key to success is the willingness to fail successfully. Every story of success is filled with times of failure but every story is also characterized by the relentlessness of starting over again and again and again until you master the task. When we started our IT project, we told people about what we were doing. We called that our "Cortez Project". Like Cortez, we scuttled our ships; there was no going back. We had to succeed.
There were other “named” initiatives in SETMA’s history in addition to the Cortez declaration. There was the Fahrenheit 451 Initiative (the kindling point of paper) where we recognized and declared that paper was too expensive and too hard for record keeping and for transformation of healthcare. While we did not burn books, we set our sights on getting rid of paper in our practice.
There was also the Maginot Line Initiative. Like the fixed fortifications built by the French after World War I, as an obstacle to invasion by Germany and which fortifications were defeated by the ability of mechanized war-machines to “go around the line,” when confronted by a seemingly insurmountable obstacle to our successful transformation, SETMA went around the obstacles.
As we began defining and developing supports required for success in Performance Improvement, we found them to be:
- Care where the same data base is being used at ALL points of care.
- A robust EHR to accomplish the above.
- A robust business-intelligence analytics system, which allows for real-time data analysis at the point of care.
- A laser printer in every examination room so that personalized evaluational, educational and engagement materials could be provided to every patient at every encounter, with the patient’s personal health data displayed and analyzed for individual goal setting and decision making.
- Quality metric tracking, auditing and statistical analysis.
- Public Reporting of quality metric performance by provider name.
- Quality Improvement initiatives based on tracking, auditing and analysis of metrics.
- Shared vision among all providers, support staff and administrators - a personal passion for excellence -- which creates its own internalized, sustainable energy for the work of healthcare transformation.
- Celebratory culture which does not compete with others but continually improves the organization’s own performance, using others as motivation but not as a standard.
- Monthly peer-review sessions with all providers, to review provider performance and to provide education in the use of electronic tools.
- Adequate financial support for the infrastructure of transformation.
- Respect of the personal value of others and the caring for people as individuals.
- An active Department of Care Coordination and a hospital-care support team which is in the hospital twenty-four hours a day, seven days a week.
- Aggressive end-of-life counseling with all patients over fifty, and active employment of hospice in the care of patients when appropriate.
The fourth seminal event was that we determined to adopt a celebratory attitude toward our progress in EMR. In May, 1999, my cofounding partner was lamenting that we were not crawling yet with our use of the EMR. I agreed and asked him, “When your son first turned over in bed, did you lament that he could not walk, or did you celebrate this first milestone of muscular coordination of turning over in bed?” He smiled and I said, “We may not be crawling yet, but we have begun. If in a year, we are doing only what we are currently doing, I will join your lamentation, but today I am celebrating that we have begun.” SETMA’s celebratory spirit has allowed us to focus on the future through many lamentable circumstances and has allowed us to press forward through many disappointments. Focusing on our successes kept us moving forward and the cumulative effect was always success.
That celebratory attitude has given SETMA the energy and resolve to face hard times and the vision of electronic patient management has given us direction and substance to our goal. Today, we are not what we were, and we are not yet what we shall be, but we are on a pilgrimage to excellence which will never end. We started eight years ago at MGMA; where is the end? There isn't one and that is what helps us get up day after day, excited about the prospect of the future. Mostly what we celebrate today is the team which EMR has facilitated our forming.
In April, 2015, CMS and the Office of the National Coordinator held a joint conference to examine the IT Support for successful Accountable Care Organizations (ACOs). (for a complete report see: http://jameslhollymd.com/Letters/health-it-to-support-aco-and-group-reporting.)
It is not surprising that SETMA’s conclusion as a participant in this meeting was that the successful ACOs would depend upon a team dynamic and upon being a learning organization. This was summarized with a quote from Senge’s The Fifth Discipline:
“Most of us at one time or another have been part of a great ‘team,’ a group of people who functioned together in an extraordinary way - who trusted one another, who complemented each other others’ strengths and compensated for each others’ limitations, who had common goals that were larger than individual goals, and who produced extraordinary results. I have met many people who have experienced this sort of profound teamwork - in sports, or in the performing arts or in business. Many say that they have spent much of their life looking for that experience again. What they experienced was a learning organization. The team that became great didn’t start off great - it learned how to produce extraordinary results.”
Being part of such a team:
- Requires each of us to be better than we have ever been before
- Enables us to be better than we have ever been before
- Motivates us to be better than we have ever been before
- Allows us to take the risk of becoming better than we have ever been before
Furthermore the success of an ACO, like the success of TCPI will depend upon a solid philosophical foundation, i.e., knowing both what we are doing and why we are doing it. This was brought home to SETMA by the response of both the surveyors and one of the executives at The Joint Commission both of whom commented on the philosophical foundation of SETMA’s work. They said: “I was just talking to one of my colleagues and showing him SETMA’s notebook which was prepared in response to The Joint Commission’s Standards and Requirements Chapter Seven on leadership.” The executive said, “Look at this; everything they do is founded upon a philosophical foundation. They know ‘what they are doing,’ but more importantly, they know why they are doing it.’” SETMA is not the result of random efforts but of innovations and advances which are consistent with a structured set of ideals, principles and goals.
Part of SETMA’s culture is our willingness and ability to accept who we are. That can be expressed in the statement: Rarely can it be said that some one is THE best of ALL because we have strengths that place us at the head of the pack and we have weaknesses which make us one of the pack. Our progress and success is dependent upon our willingness to celebrate our strengths without arrogance and hubris and to acknowledge our weaknesses with humility and resolve to improve.
Whether in relationship to the ACOs success or the success of TCPI, communication and integration of the healthcare team through the power of IT will be critical. When the Robert Wood Johnson Foundation engaged the McColl Institute to conduct the Learning from Exemplary Practices (LEAP) study, 30 practices were selected from 400 nominees. SETMA was selected as one of the exemplar practices. After a four-day site visit, the survey team concluded the following comments.
The uniqueness of SETMA’s IT Department was a surprise to them. They felt that SETMA has approached healthcare transformation differently than anyone they have seen. They related that uniqueness to the decision we made in 1999 to morph from the pursuit of “electronic patient records” to the pursuit of “electronic patient management.” They were surprised to see how centrally and essentially electronics are positioned into SETMA and how all other things are driven by the power of electronics. They marveled at the wedding of the technology of IT with clinical excellence and knowledge. The communication and integration of the healthcare team through the power of IT is novel, they concluded.
The first four conclusions they reached are the following.
- The Care Coordination Department - they had never heard of such a department and had never seen one. They were impressed at how the department is integrated with the clinical personnel through electronic communication and how critical they are to our mission. Across the nation, transformative efforts in healthcare include what is referred to as “daily huddles” - meetings to discuss patient care and the day's activities. They were interested in SETMA’s concept of “electronic huddles” where there is continuous communications between departments and colleagues to strengthen, coordinate and improve care.
- The Care Transition and Hospital Care Team -- The complex solutions for this critical area of practice is very impressive to them. The integration of care with the admission hospital plan of care, the discharge Hospital Care Summary and Post Hospital Plan of Care and Treatment plan, the hospital follow-up care coaching call and other aspects of this care transition process, they identified as innovative improvements in the work force relationships among staff.
- The I-Care team - they are very impressed with the electronic tools we have with which to support the work of the full time staff and the professional support staff for I-Care. SETMA has worked in the long term residential care area for its entire existence and before. But, they were impressed with how a group of SETMA providers built upon that foundation and organized an excellent integration of work flow innovations to improve that care.
- Learning Team - they believe that the spontaneous and structured learning of SETMA allows us to continually and almost unintentionally learn and grow. They understand that learning, as Senge says, is only distantly related “to taking in more information.” They believe that we have incorporated “systems thinking” and “systems structures” into SETMA extremely well. They think this is one of the most value aspects of SETMA’s work force and work flow innovations. They were able to attend one of SETMA’s monthly training meetings and were intrigued by the enthusiastic and engaged participation by all of SETMA’s healthcare providers.
The CMS/ONC Conference was also focused on Group Reporting for success in the ACO model of care. (for details on SETMA’s tool for this see: http://jameslhollymd.com/EPM-Tools/Accountable-Care-Organization-Quality-Measures-Performance-Tool-Tutorial.)
SETMA has concluded that the tracking of quality metrics alone will not result in health care delivery transformation and/or improvement. Transformation and improvement will require the combining and tracking of quality metrics(access, outcome, patient experience, process, structure and costs of care, etc) with data analytics. This concept is addressed in depth in the presentation found at the following link:
http://jameslhollymd.com/Presentations/The-Importance-of-Data-Analytics-in-Physician-Practice.
The following are bullet point summations of this presentation:
- “The juxtaposition of vision (what we want) and a clear picture of current reality (where we are) generates ‘creative tension,’ (which is) a force to bring vision and reality together, through the natural tendency of tension to seek resolution.”
- Analytics transform knowledge into an agent for change. In reality, without analytics, we will neither know where we are, where we are going or how to sustain the effort to get there.
- For transformation to take place through knowledge, we must be prepared to ask the right questions, courageously accept the answers and to require ourselves to change.
- Healthcare transformation, which will produce continuous performance improvement, results from internalized ideals, which create vision and passion, both of which produce and sustain “creative tension” and “generative thinking.”
- Transformation is not the result of pressure and it is not frustrated by obstacles. In fact, the more difficult a problem is, the more power is created by the process of transformation in order to overcome the problem.
- The greatest frustration to transformation is the unwillingness or the inability to face current reality. Often, the first time healthcare provides see audits of their performance, they say, “That can’t be right!”
- Through analytics - tracking data, auditing performance, and statistical analysis of results - we learn the truth. For that truth to impact our performance, we must believe it.
- Through acknowledging truth, privately and publicly, we empower sustainable change, making analytics a critical aspect of healthcare transformation.
- While an Electronic Health Record (EHR) has tremendous capacity to capture data that is only part of the solution. The ultimate goal must be to improve patient care and patient health, and to decrease cost, not just to capture and store information!
- Electronic Patient Management employs the power of electronics to track, audit, analyze and display performance and outcomes, thus powering transformation.
- Public Reporting by Provider name is transformative but quality metrics are not an end in themselves.
- Optimal health at optimal cost is the goal of quality care. Quality metrics are simply “sign posts along the way.” They give directions to health.
- Metrics coupled with analytics are like a healthcare “Global Positioning System”: it tells you where you are, where you want to be, and how to get from here to there.
- Different elements of statistical analysis give different insight into population management, i.e. the mean may be at goal in a population but if the standard deviation is high, many are not to goal and efforts must be designed and made to maintain the mean while improving the standard deviation.
The identification of valuable quality metrics and the description and definition of them are a science. National Quality Forum, Physician Consortium for Performance Improvement (PC-PI), the National Committee for Quality Assurance (NCQA - HEDIS) and other organizations are equipped with the staff, experience and principles to identify and describe these metrics. Success with quality metrics will be built upon a sound philosophy and upon sound principles, some of which are:
- Quality metrics are not an end in themselves. Optimal health at optimal cost is the goal of quality care. Quality metrics are simply “sign posts along the way.” They give directions to health. And the metrics are like a healthcare “Global Positioning Service”: it tells you where you want to be; where you are, and how to get from here to there.
- The auditing of quality metrics gives providers a coordinate of where they are in the care of a patient or a population of patients.
- Statistical analytics are like coordinates along the way to the destination of optimal health at optimal cost. Ultimately, the goal will be measured by the well-being of patients, but the guide posts to that destination are given by the analysis of patient and patient-population data.
- There are different classes of quality metrics. No metric alone provides a granular portrait of the quality of care a patient receives, but all together, multiple sets of metrics can give an indication of whether the patient’s care is going in the right direction or not. Some of the categories of quality metrics are: access, outcome, patient experience, process, structure and costs of care.
- The collection of quality metrics should be incidental to the care patients are receiving and should not be the object of care. Consequently, the design of the data aggregation in the care process must be as non-intrusive as possible. Notwithstanding, the very act of collecting, aggregating and reporting data will tend to create a Hawthorne effect.
- The power of quality metrics, like the benefit of the GPS, is enhanced if the healthcare provider and the patient are able to know the coordinates while care is being received.
- Public reporting of quality metrics by provider name must not be a novelty in healthcare but must be the standard. Even with the acknowledgment of the Hawthorne effect, the improvement in healthcare outcomes achieved with public reporting is real.
- Quality metrics are not static. New research and improved models of care will require updating and modifying metrics.
The New York Times Magazine of May 2, 2010, published an article entitled, "The Data-Driven Life," which asked the question, "Technology has made it feasible not only to measure our most basic habits but also to evaluate them. Does measuring what we eat or how much we sleep or how often we do the dishes change how we think about ourselves?" Further, the article asked, "What happens when technology can calculate and analyze every quotidian thing that happened to you today?" Does this remind you of Einstein's admonition, "Not everything that can be counted counts, and not everything that counts can be counted?"
Technology must never blind us to the human. Bioethicist, Onora O'Neill, commented about our technological obsession with measuring things. In doing so, she echoes the Einstein dictum that not everything that is counted counts. She said, "In theory again the new culture of accountability and audit makes professionals and institutions more accountable for good performance. This is manifest in the rhetoric of improvement and rising standards, of efficiency gains and best practices, of respect for patients and pupils and employees. But beneath this admirable rhetoric the real focus is on performance indicators chosen for ease of measurement and control rather than because they measure accurately what the quality of performance is."
In our quest for excellence, we must not be seduced by technology with its numbers and tables. This is particularly the case in healthcare. In the future of medicine, the tension - not a conflict but a dynamic balance - must be properly maintained between humanity and technology. Technology can contribute to the solving of many of our disease problems but ultimately cannot solve the "health problems" we face. The entire focus and energy of "health home" is to rediscover the trusting bond between patient and provider.
In the "health home," technology becomes a tool to be used and not an end to be pursued. The outcomes of technology alone are not as satisfying as those where trust and technology are properly balanced in healthcare delivery. Our grandchildren's generation will experience healthcare methods and possibilities which seem like science fiction to us today. Yet, that technology risks decreasing the value of our lives, if we do not in the midst of technology retain our humanity.
As we celebrate science, we must not fail to embrace the minister, the ethicist, the humanist, the theologian, indeed the ones who remind us that being the bionic man or women will not make us more human, but it seriously risks causing us to being dehumanized. And in doing so, we may just find the right balance between technology and trust and thereby find the solution to the cost of healthcare.
It is in this context that SETMA whole-heartedly embraces technology and science, while retaining the sense of person in our daily responsibilities of caring for persons. Quality metrics have made us better healthcare providers. The public reporting of our performance of those metrics has made us better clinician/scientist. But what makes us better healthcare providers is our caring for people.
SETMA believes that the key to the future of healthcare is an internalized ideal and a personal passion for excellence rather than reform which comes from external pressure. Transformation is self-sustaining, generative and creative.
In this context, SETMA believes that efforts to transform healthcare may fail unless four strategies are employed, upon which SETMA depends in its transformative efforts:
- The methodology of healthcare must be electronic patient management.
- The content and standards of healthcare delivery must be evidenced-based medicine.
- The structure and organization of healthcare delivery must be patient-centered medical home.
- The payment methodology of healthcare delivery must be that of capitation with additional reimbursement for proved quality performance and cost savings.
At the core of these four principles is SETMA’s belief and practice that one or two quality metrics will have little impact upon the processes and outcomes of healthcare delivery and, they do little to reflect quality outcomes in healthcare delivery.
In the Centers for Medicare and Medicaid Services (CMS) Physician Quality Reporting System (PQRS), healthcare providers are required to report on at least three quality metrics. This is a minimalist approach to providers quality reporting and is unlikely to change healthcare outcomes or quality. PQRS allows for the reporting of additional metrics and SETMA reports on 28 PQRS measures. One of the greatest “missed opportunities” in healthcare transformation was in the design of PQRS. If, all primary physicians, had been required to report on a comprehensive measurement set for diabetes, we would today have a data base which could be used to transform the care of this condition and which would allow us to measure different approaches to healthcare delivery.
SETMA employs two definitions in our transformative approach to healthcare:
- A “cluster” is seven or more quality metrics for a single condition, i.e., diabetes, hypertension, etc.
- A “galaxy” is multiple clusters for the same patient, i.e., diabetes, hypertension, lipids, CHF, etc.
SETMA believes that fulfilling a single or a few quality metrics does not change outcomes, but fulfilling “clusters” and “galaxies” of metrics, which are measurable at the point-of-care, can and will change outcomes. The following illustrates the principle of a “cluster” of quality metrics. A single patient at a single visit, for a single condition, will have eight or more quality metrics fulfilled for a condition, which WILL change the outcome of that patient’s treatment.
The following illustrates a “galaxy” of quality metrics. A single patient, at a single visit, may have multiple “clusters” surrounding multiple chronic conditions thus having 60 or more quality metrics fulfilled in his/her care, which WILL change the quality of outcomes and will result in the improvement of the patient’s health. And, because of the improvement in care and health, the cost of that patient’s care will decrease as well.
SETMA"s model of care is based on these four principles and the concepts of “clusters” and “galaxies” of quality metrics. (For a full explanation of this “model of care:” see http://jameslhollymd.com/the-setma-way/setma-model-of-care-pc-mh-healthcare-innovation-the-future-of-healthcare) Foundational to this concept is that the fulfillment of quality metrics is incidental to excellent care rather than being the intention of that care.
- The tracking by each provider on each patient of the provider’s performance on preventive care, screening care and quality standards for acute and chronic care. SETMA"s design is such that tracking occurs simultaneously with the performing of these services by the entire healthcare team, including the personal provider, nurse, clerk, management, etc.
- The auditing of performance on the same standards either of the entire practice, of each individual clinic, and of each provider on a population, or of a panel of patients. SETMA believes that this is the piece missing from most healthcare programs.
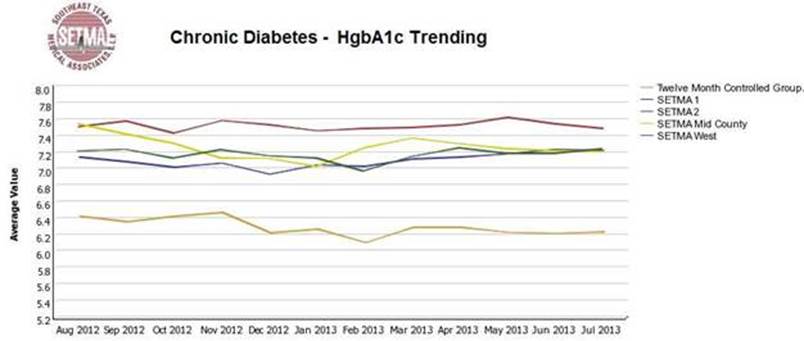
- The statistical analyzing of the above audit-performance in order to measure improvement by practice, by clinic or by provider. This includes analysis for ethnic disparities, and other discriminators such as age, gender, payer class, socio-economic groupings, education, frequency of visit, frequency of testing, etc. This allows SETMA to look for leverage points through which SETMA can improve the care we provide.
- The public reporting by provider of performance on hundreds of quality measures. This places pressure on all providers to improve, and it allows patients to know what is expected of them. The disease management tool “plans of care” and the medical-home-coordination document summarizes a patient’s state of care and encourages them to ask their provider for any preventive or screening care which has not been provided. Any such services which are not completed are clearly identified for the patient. We believe this is the best way to overcome provider and patient “treatment inertia.”
- The design of Quality Assessment and Performance Improvement (QAPI) Initiatives - this year SETMA"s initiatives involve the elimination of all ethnic diversities of care in diabetes, hypertension and dyslipidemia. Also, we have designed a program for reducing preventable readmissions to the hospital. We have completed a Business Intelligence (BI) report which allows us to analyze our hospital care carefully.
The Physician Consortium for Performance Improvement (PCPI) is an organization created by the AMA, CMS, Institute of Medicine and others to develop measurement sets for quality assessment. The intent is to allow healthcare providers to evaluate their own performance at the time they are seeing a patient.
SETMA is tracking a number of these measurement sets including: Chronic Stable Angina, Congestive Heart Failure, Diabetes, Hypertension, and Chronic Renal Disease Stages IV through ESRD, Adult Weight Management, and Care Transitions. Others will be added overtime. The details of these measurement sets and SETMA"s provider performance on each can be found under Public Reporting PCPI.
In addition to Provider Performance Tracking tools, such as those produced by PCPI, the National Quality Foundation (see Public Reporting NQF), and National Committee for Quality Assurance (see Public Reporting HEDIS and/or NCQA), SETMA has designed a pre-visit quality measures screening and preventive care tool. This allows a SETMA provider and a patient to quickly and easily assess whether or not the patient has received all of the appropriate preventive health care and the appropriate screening health care which national standards establish as being needed by this patient. The following is the Pre-visit Preventive Screening tool. All measures in black apply to the current patient and are fulfilled. All measures in red apply to the current patient and have not been fulfilled and all measures in grey do not apply to the current patient. If a point of care is missing, it can be fulfilled with the single click of a single button.
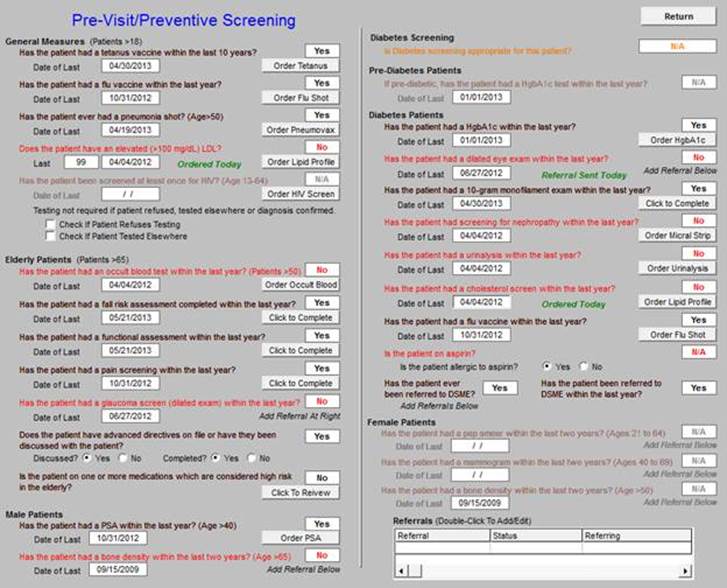
There are similar tracking tools for all of the quality metrics which SETMA providers track each day. The following is the tool for NQA measures:

The providers’ compliance with these measures is color coded for quick reference. The “view” button allows the provider to quickly review the content of the metric and to review the patient’s results.
While healthcare provider performance is important for excellent care of a patient’s health, there are 8,760 hours in a year. A patient who receives an enormous amount of care in a year is in a provider’s office or under the provider’s direct care less than 60 hours a year. This makes it clear that the patient is responsible for the overwhelming amount of their own care which includes compliance with formal healthcare initiatives and with lifestyle choices which support their health.
If responsibility for a patient’s healthcare is symbolized by a baton, the healthcare provider carries the baton for .68% of the time. That is less than 1% of the time. The patient carries the baton 99.32% of the time. The coordination of the patient’s care between healthcare providers is important but the coordination of the patient’s care between the healthcare providers and the patient is imperative.
Often, it is forgotten that the member of the healthcare delivery team who carries the “baton" for the majority of the time is the patient and/or the family member who is the principal caregiver. If the „baton" is not effectively transferred to the patient or caregiver, then the patient’s care will suffer.

Firmly in the providers hand
--The baton - the care and treatment plan
Must be confidently and securely grasped by the patient, If change is to make a difference
8,760 hours a year.
The poster illustrates:
- That the healthcare-team relationship, which exists between the patient and the healthcare provider, is key to the success of the outcome of quality healthcare.
- That the plan of care and treatment plan, the “baton,” is the engine through which the knowledge and power of the healthcare team is transmitted and sustained.
- That the means of transfer of the “baton” which has been developed by the healthcare team is a coordinated effort between the provider and the patient.
- That typically the healthcare provider knows and understands the patient’s healthcare plan of care and the treatment plan, but that without its transfer to the patient, the provider’s knowledge is useless to the patient.
- That the imperative for the plan - the “baton” - is that it be transferred from the provider to the patient, if change in the life of the patient is going to make a difference in the patient’s health.
- That this transfer requires that the patient “grasps” the “baton,” i.e., that the patient accepts, receives, understands and comprehends the plan, and that the patient is equipped and empowered to carry out the plan successfully.
- That the patient knows that of the 8,760 hours in the year, he/she will be responsible for “carrying the baton,” longer and better than any other member of the healthcare team.
The genius and the promise of the Patient-Centered Medical Home are symbolized by the “baton.” Its display will continually remind the provider and will inform the patient, that to be successful, the patient’s care must be coordinated, which must result in coordinated care. In 2011, as we expand the scope of SETMA"s Department of Care Coordination, we know that coordination begins at the points of “transitions of care,” and that the work of the healthcare team - patient and provider - is that together they evaluate,
The creating of quality measures is a complex process. That is why it is important for agencies such as the Ambulatory Care Quality Alliance (AQA), the NCQA, the NQF, the Physician Quality Reporting System (PQRS) and PCPI, among others, to identify, endorse and publish quality metrics. The provider’s ability to monitor their own performance and the making of those monitoring results available to the patient is important, but it only allows the provider to know how they have performed on one patient. However, the aggregation of provider performance over his/her entire panel of patients, through an auditing tool, carries the process of designing the future of healthcare delivery a further and a critical step. The problem with most auditing results, such as HEDIS, is that it is presented to the provider 12 to 18 months after the fact. SETMA believes that “real time” immediate auditing and giving of the audit results to providers can change provider behavior and can overcome “treatment inertia.”
Auditing of provider performance allows physicians and nurse practitioners to know how they are doing in the care of all of their patients. It allows them to know how they are doing in relationship to their colleagues in their clinic or organization, and also how they are performing in relationship to similar practices and providers around the country. As a result, SETMA has designed auditing tools through the adaptation to healthcare of a business intelligence software.
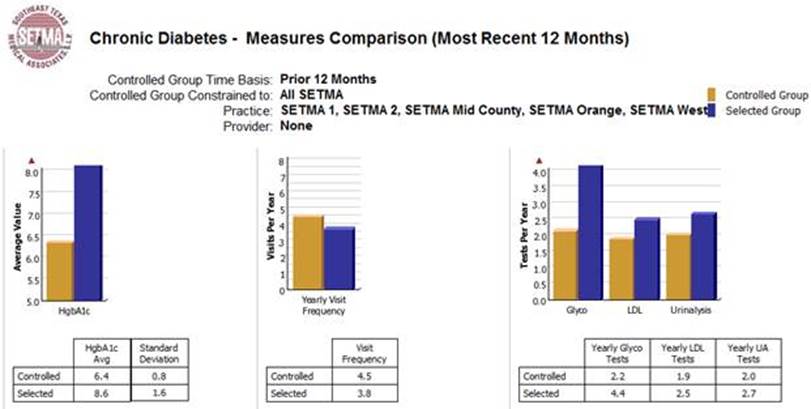
The following are a few examples of the auditing SETMA does of provider performance.
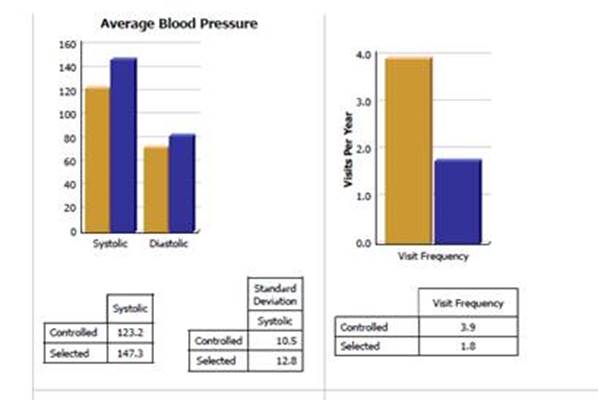
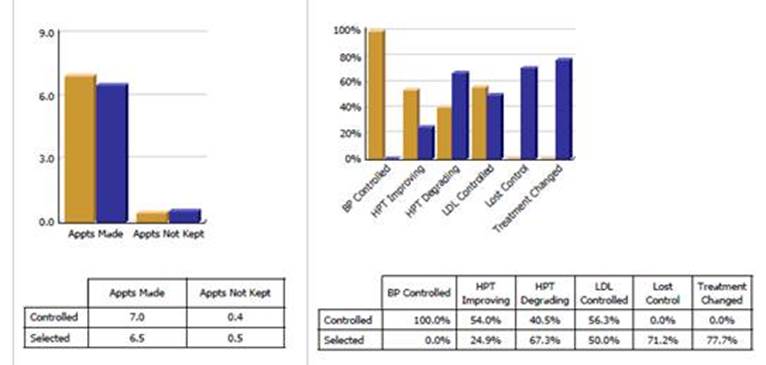
Through BI, SETMA is able to display outcomes trending which can show seasonal patterns of care and trending comparing one provider with another. It is also possible to look at differences between the care of patients who are treated to goal and those who are not. Patients can be compared as to socio-economic characteristics, ethnicity, frequency of evaluation by visits and by laboratory analysis, numbers of medication, payer class, cultural, financial and other barriers to care, gender and other differences. This analysis can suggest ways in which to modify care in order to get all patients to goal.
Using digital dashboard technology, SETMA analyzes provider and practice performance in order to find patterns which can result in improved outcomes practice wide for an entire population of patients. We analyze patient populations by:
- Provider Panel
- Practice Panel
- Financial Class - payer
- Ethic Group
- Socio-economic groups
We are able to analyze if there are patterns to explain why one population or one patient is not to goal and others are. We can look at:
- Frequency of visits
- Frequency of testing
- Number of medications
- Change in treatment
- Education or not
- Many other metrics
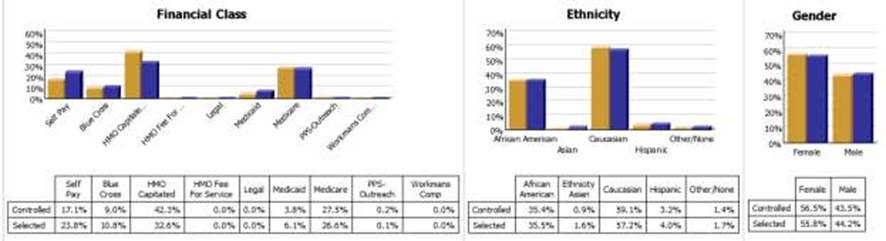
We are able to present over-time patient results comparing:
- Provider to practice
- Provider to provider
- Provider current to provider over time
- Trending of results to see seasonal changes, etc.
Raw data can be misleading. It can cause you to think you are doing a good job when in fact many of your patients are not receiving optimal care. For instance the tracking of your average performance in the treatment of diabetes may obscure the fact that a large percentage of your patients are not getting the care they need. Provider Performance at the point of service is important for the individual patient. Provider Performance over an entire population of patients is important also. However, until you analyze your performance data statistically, a provider will not know how well he or she is doing or how to change to improve the care they are providing.
Each of the statistical measurements which SETMA tracks, the mean, the median, the mode and the standard deviation, tells us something about our performance. And, each measurement helps us design quality improvement initiatives for the future. Of particular, and often, of little known importance is the standard deviation.
From 2000 to 2015, SETMA has shown annual improvement in the mean (the average) and the median results for the treatment of diabetes. There has never been a year when we did not improve. Yet, our standard deviations revealed that there were still significant numbers of our patients who are not being treated successfully. Even here, however, we have improved. From 2008 to 2013, SETMA experienced a 9.3% improvement in standard deviation. Some individual SETMA providers had an improvement of over 16% in their standard deviations. Our goal for 2010 is to have another annualized improvement in mean and in median, and also to improve our standard deviation. When our standard deviations are below 1 and as they approach .5, we can be increasingly confident that all of our patients with diabetes are being treated well.
An example of a statistical analysis of SETMA"s diabetes care in regard to the elimination of ethnic disparities of care is given in the article Eliminating Ethnic Disparities in Diabetes Care Your Life Your Life Your Health The Examiner May 13, 2010.
One of the most insidious problems in healthcare delivery is reported in the medical literature as “treatment inertia.” This is caused by the natural inclination of human beings to resist change. Often, when patients" care is not to goal, no change in treatment is made. As a result, one of the auditing elements in SETMA’s BI Project is the assessment of whether a treatment change was made when a patient was not treated to goal. Overcoming “treatment inertia” requires the creating of an increased level of discomfort in the healthcare provider and in the patient so that both are more inclined to change their performance. SETMA believes that one of the ways to do this is the public reporting of provider performance. That is why we are publishing provider performance by provider name under Public Reporting.
The following is a report which appears on our website for 2009-2015 through September 30, 2015 in the NCQA Diabetes Recognition audit. All SETMA providers have earned NCQA recognition.
A more complete explanation of SETMA"s philosophy and intent in “public reporting” of Provider’s performance can be found in the following articles:
Quality Improvement Initiatives based on tracking, auditing, statistical analysis and public reporting of provider performance are critical to the transformation of healthcare both as to quality of care and as to cost of care.
With the above described data in hand and with the analysis of that data, it is possible to design quality initiatives for future improvement in care. Currently SETMA is designing two major quality initiatives. One is for diabetes. It is an attempt to eliminate the last vestiges of ethnic disparity in the care of diabetes. This will require the use of additional internal resources and attention but it is our intent to do so and to permanently and totally eliminate ethnic disparities. The other is in regard to decreasing avoidable readmissions to the hospital.
The details of these two initiatives can be reviewed here:
Without a systems approach to healthcare, each of these steps are impossible; certainly, the analysis and transformation of healthcare is impossible. With a systems approach, this logical and sequential process is possible and rewarding for provider and patient. This process has also set SETMA on a course for successful and excellent healthcare delivery. Our tracking, auditing, analysis, reporting and design will keep us on that course.
SETMA’s Model of Care has and is transforming our delivery of healthcare, allowing us to provide cost-effective, excellent care with high patient satisfaction. This Model of Care is evolving and will certainly change over the years as will the quality metrics which are at its core.
Key to the success of TCPI will be your ability to examine complex tasks and through “process analysis” to design effective solutions. On March 30, 2012, I gave a presentation to the Massachusetts Medical Society, entitled, The Importance of Data Analytics in Physician Practice. (see: http://jameslhollymd.com/Presentations/The-Importance-of-Data-Analytics-in-Physician-Practice; a modification of this address was presented at Grand Rounds at the University of Texas Health Science Center, San Antonio, July 15, 2015 in a different format, see: http://jameslhollymd.com/Presentations/setmas-automated-team-function.)
In Boston, there were three speakers, each had an hour to speak and I was the last speaker. The first speaker asked, “How many tasks can you get a healthcare provider to perform at every patient encounter?” A vigorous discussion ensued at the end of which the speaker said, “I think you can get providers to do one thing.” As the last speaker, I began by saying, “I would like to answer the first speaker’s question, but to do so, you must first answer the following questions”:
- How important is the task you are asking providers to do?
- How much time does it take?
- How much energy does it take?
If you were to create a formula to represent this process, there would be a direct correlation between how many tasks a provider can or will do and how important the tasks are; the more important the tasks, the more tasks a provider will do. There would be an inverse relationship between how much time it takes and how many tasks will be done; the more time it takes, the fewer tasks will be done. There would also be an inverse relationship between how much energy it takes and how many tasks will be done; the more energy it takes, the fewer tasks will be done.
The key to getting more done is to determine what is important and only to do that, and then to make the completion of the important tasks require less energy and less time. Let me illustrate. The Texas State Health Department’s Reportable Conditions illustrates the standardization and the automation of parts of healthcare processes. Remember Peter Senge’s statement in The Fifth Discipline: “The more complex a problem is, the more systemic the solution must be.”
After the below discussion, which shows that with electronics, many complex and important tasks can be reduced to one second, or no seconds, with little energy expenditure, In he Boston discussion, I concluded: it is possible to get providers to do thirty or forty things every time they see a patient and at SETMA we do.
How can healthcare providers design a solution to a complex healthcare problem, particularly when the problem is not generated by a patient’s request but by a public-health need? In the former case, the provider simply determines if the request is appropriate or not. In the latter case, no one is in the provider’s office requesting a service; a requirement has been established and it is up to the provider, in the midst of many other demands, to remember and to fulfill the requirement. In the case of infectious diseases, requirements have been published for providers to report the occurrence of dozens of conditions.
The medical literature is filled with reports of a very low compliance of physicians with reporting infectious disease to State Health Departments. In Texas, there are 78 infectious diseases which require reporting. The window for reporting compliantly varies from immediate, to one working day, to one week, to ten days, to one month. It is improbable that many healthcare providers know the entire list or the requirement for reporting. The Department of Health wants the report to be triggered by a suspicion and not by a confirmed diagnosis. If the provider waits until the confirmation is made, the opportunity for a public health intervention is lost.
A systems solution would be best. The ideal solution would be an electronic medical record system in which the reporting action is triggered by the documentation of the diagnosis in the assessment in the EMR.
The following is the scenario which resulted in the systems solution being designed and deployed 48 hours later. On April 30, 2011, Dr. Holly made a presentation for a CME program at Texas A&M College of Medicine. The lecturer who followed him was Dr. Edward J. Sherwood, who lectured on “The Ethics of Infectious Disease.” Dr. Sherwood distributed a publication of the Texas State Health Department which detailed the 78 reportable conditions.
SETMA’s IT Department was charged with deploying a functionality which would:
- Display the reportable conditions for provider review
- Detail the time frame in which each infectious disease should be reported.
- Denote on the display of the reportable conditions the infectious disease which is identified by the provider. This would be done automatically when the diagnosis is documented on the assessment template in the EMR.
- Simultaneous with number three, a telephone message would be sent to SETMA’s Care Coordination which would then make the call or send the fax to report the infectious disease. The fact that this had been done will be stored in the EMR in a searchable fashion.
On SETMA’s AAA Home template, which is the place on all care begins, there is a new button entitled Reportable Conditions. It can be seen below outlined in Green.
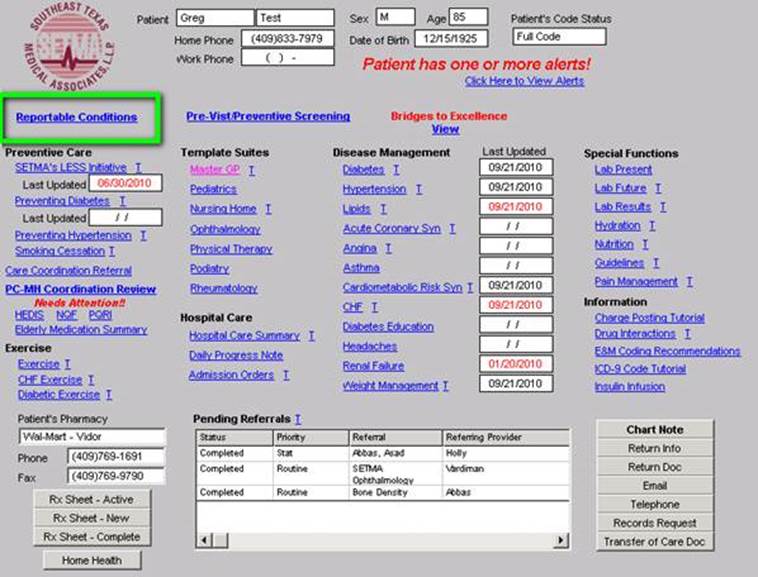
When this button is deployed the following template appears. The template can be used as a review for providers or nurses of what needs to be reported and/or to note that the diagnosed infectious condition, in this case “measles,” has been automatically checked as a result of the provider having selected this diagnoses on the assessment template.
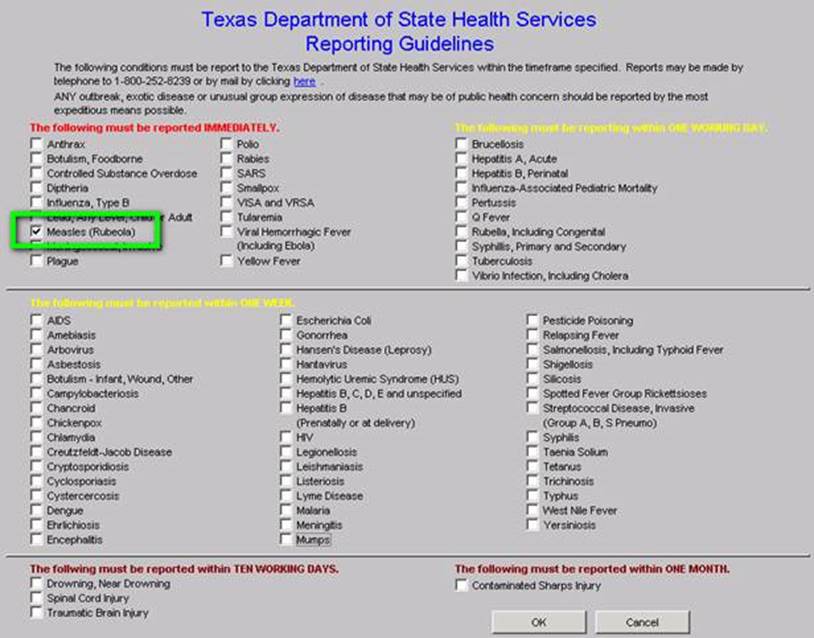
The above checking off of “measles” was noted automatically when the ICD-9 and soon to be ICD-10 code was selected by the provider as is seen below. (Clinicians will amuse themselves with the co-morbidities denoted in this selected “test” patient. It is generally not the case to find measles in patients with diagnoses which are probably from an elderly patient.)
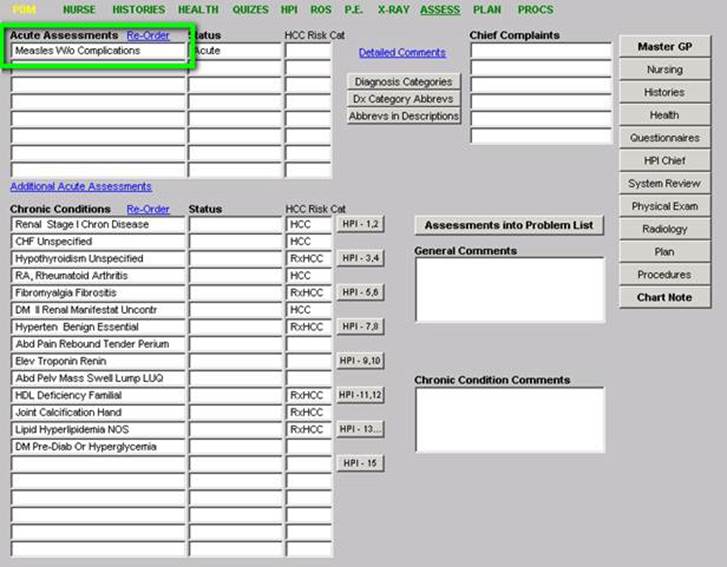
When the infectious disease diagnosis is selected, the system:
- Automatically checks the diagnosed infectious disease on the list of infectious disease
- A telephone message is sent to SETMA’s Care Coordination Department.
- The call notification appears in the workflow of the Care Coordination team.
- Once the report is made a note is added to the patient’s chart noting that Health Department notification has been done.
The following is the Care Coordination telephone alert:
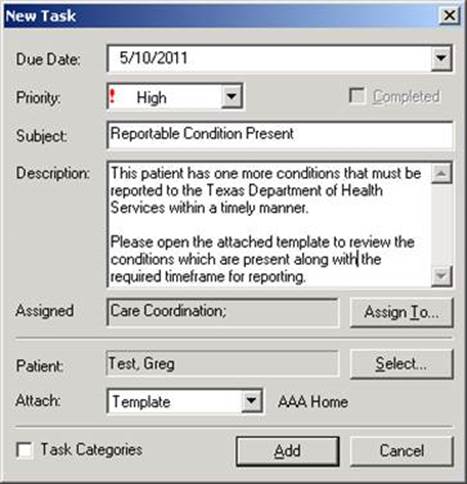
At this point, the process is complete. The entire responsibility of the provider is to make the presumed diagnosis. The remainder is done by a systems protocol which is automatic. We expect this to increase the reporting of infectious disease by SETMA to almost 100% thus improving individual patient care, community care and public health.
If you click the link circled below, it will automatically launch the form if you chose to do the report by mail.
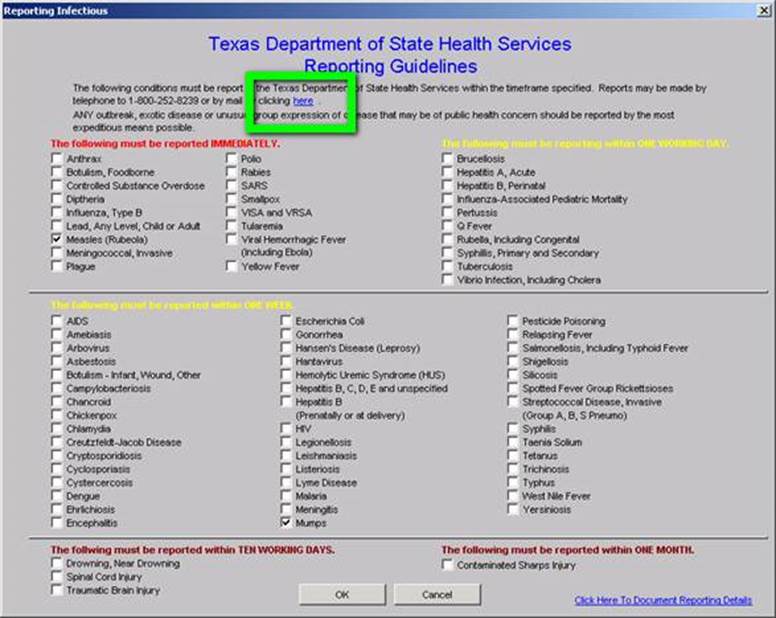
When the Care Coordination department reports the infection, the following allows for the documentation of that report.
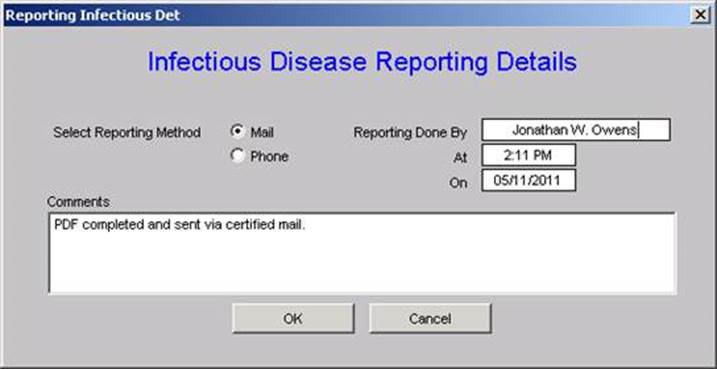
Quarterly and annually, SETMA will create the following audits:
- How many infectious diseases were documented as having been suspected by providers in the practice? These will be categorized by each of the 78 reportable conditions listed above.
- How many infectious diseases were reported to the appropriate health agency?
- How many of each infectious diseases were reported within the designated time frame?
- If a confirmatory test was performed, what percentage of the report conditions were proved to be present?
This material will be an ongoing quality improvement project by SETMA.
This is a simple but elegant electronic solution to a complex problem which has never been completely solved in healthcare provider workflow. It requires no time on the part of the provider. It is measurable and it is sustainable. Since SETMA designed this solution, several issues have arisen which were unanticipated.
- Does the Department of Health want previously reported incidences of chronic infectious diseases such as hepatitis and HIV to be re-reported?
- Does the Department of Health want infectious diseases previously reported in other states reported when the patient moves to Texas?
- Does the state have a way of determining that a chronic infectious disease has been previously reported or not?
- In regard to EMR solutions, the diagnosis of "Coumadin Toxicity" is reported as an "overdose." Obviously, this is not the intent of the desire for public health officials to know the incidence of narcotic or psychotropic drug overdoes. The power of electronics has to be guided so as not to report conditions not intended to be reported.
It is probable that as we proceed, other issues in reporting infectious diseases will arise. The good news is that the above issues have not been considered previously and decisions are being made as to what the answers are. We are all learning and with electronics, we are all participating in improving the care Texans and Americans are receiving.
If an important task is not being done either because the provider is resistant to doing it, or because the provider has “too much” to do, automate it. (Remember the Maginot Line)
- How much time does it take the provider to complete this reporting? None
- How much energy does it take the provider to complete this reporting? None
- How important for public health is this reporting requirement? Very important
- How effective is SETMA’s solution? Perfect reporting is continuously achieved
A second process analysis illustrates the power of electronic solutions to complex problems in healthcare. In August, 2010, the American Academy of Family Practice Journal recommended that every family physician calculate one Framingham Risk Score for each of their patients every five years.
The Framingham Study which began in 1949 is the longest running longitudinal health risk study ever undertaken. "Longitudinal" means that the same subjects are included at all stages of the study. There are weaknesses to the study. Often the Cardiovascular Risk calculators overestimate a person's health risk and because total cholesterol was the principle lipid element measured when the study was started, the data does not assess the risk of Low Density Lipoproteins (LDL, which is the "bad cholesterol)." We now know that controlling your LDL is the most important issue related to lipids and health risk.
Even though these risk calculators are not perfect, they are still the best we have. And, it is imperative that you know and that your provider knows what your risk is, because it is with the knowledge of your risk that a plan of care and a treatment plan can be designed to help you preserve your health. Remember, "risk" is an attempt to determine what the future might be like which means it is imprecise. Some people with a high risk will not experience poor health and some who have low risk will. Overall, however, those with high risk will have more heart attacks and strokes than those with low risk.
The problem with biological systems is that change, even change which results in deterioration of your health, does not occur quickly and it often occurs without any signs or symptoms until the illness, or disease process has already caused significant damage. There is no explanation of this principle more apt to our use of "risk calculators" than Peter Senge's explanation of "dynamic complexity" in The Fifth Discipline.
Senge defines "dynamic complexity" as a situation "where cause and effect are subtle, and where the effects over time of interventions are not obvious." This perfectly describes the development of many disease states and the benefit of their treatment. We know that obesity causes, or contributes to most diseases including type 2 diabetes, hypertension, heart disease, cancer, etc. In these conditions, "obesity" is the cause; "cancer" is the effect, but the change is slow and is not apparent. Also, the results of treatment are very slow. Consequently, it is hard to sustain the changes necessary to eliminate the "cause," which is obesity, in order to avoid the "effect" which is cancer.
There are structural problems which aggravate the obvious solutions to a business or a health problem; Senge addresses one of these and calls it "the shifting the burden." He defines "shifting the burden," as "an underlying problem generates symptoms that demand attention. But the underlying problem is difficult for people to address, either because it is obscure or costly to confront. So people 'shift the burden' of their problem to other solutions - well intentioned, easy fixes which seem extremely efficient. Unfortunately, the easier 'solutions' only ameliorate the symptoms; they leave the underlying problem unaltered. The underlying problem grows worse, unnoticed because the symptoms apparently clear up, and the system loses whatever ability it had to solve the underlying problem."
This happens in healthcare when a person looks to healthcare providers or medications to solve a problem which can only be solved by their own habits, choices, decisions and resolution. A pill, or a procedure, or a prescription is sought in order to overcome the "obesity." It will work for a short while but not long term. When it fails, more aggressive interventions are tried without addressing the fundamental problem.
Senge's business prescription is a good one for healthcare, also. He says, "Beware the symptomatic solution...that address only the symptoms...not fundamental causes, tend to have short-term benefits at best. In the long term, the problem resurfaces and there is increased pressure for symptomatic response. Meanwhile, the capability for fundamental solutions can atrophy." (p. 104) Senge adds, "The 'easy solution...the 'quick fix'...solves the problem temporarily....(but) a shifting of burden structure lurks behind many 'solutions (and) explains a wide range of behaviors where well-intentioned 'solutions' actually makes matters worse over the long term." (p. 107)
The longer a person delays addressing the "real" cause of their problem, the fewer options and the fewer resources they have for dealing with the "real" cause of the problem. For instance, the longer a person fails to exercise, often resulting in gaining weight and diminishing heart function, the more difficult effective solutions will be once a person determines to improve their health. If a person continues to "shift the burden" of their own irresponsibility to another, expecting an artificial solution to relieve the burden created by the rejection of the real solution, they will never achieve their goal. In this case, the harder the patient pushes for solutions from a healthcare system which cannot solve their problem, for which a natural and obvious solution exists, the less benefit the patient will achieve. It is possible to ignore the real solutions - i.e., activity such as walking - until the knees and other joints have deteriorated and it is not possible to become active. In that case, more and more pressure is placed on the artificial system with less and less satisfaction with the results.
These are the reasons for our using "risk calculators." Because in a biological system proving the benefit of fundamental solutions by waiting for the negative consequences of poor health choices is not acceptable, we use "risk calculators" to project what those poor choices will lead to. Hopefully, those risk calculators will help you make a decision to make a change. The American Academy of Family Practice (AAFP) recommends that a healthcare provider calculate these risk factors every five years for their patients. By accessing Cardiovascular Risk Calculators by Alan E Leifeste, you will be able to read Dr. Alan Leifeste's letter to the AAFP about SETMA's use of Framingham Risk Calculators.
More Information Found at www.jameslhollymd.com
The details of each of the risk calculators including the elements of your health used in calculating each score can be found on SETMA's website (www.jameslhollymd.com) under "Electronic Patient Management Tools" by clicking on "Framingham Cardiovascular Risk" and then accessing "Framingham Cardiovascular and Stroke Risk Assessment Tutorial." In addition, at our website under "Your Life Your Health", twenty-two articles can be found under "View Articles by Subject" and accessing "Cardiovascular Disease Risk Factors."
Because it takes SETMA only one second (really) to calculate all twelve risk calculators, we thought we were doing great. However, when we showed this function to Dr. Richard Jackson he commented that these scores overstate the risk and Dr. Kenneth Snow asked if we could show the patient how their risk would be affected if they make a change in their habits? Sadly, we had to admit that we could not. That was on Tuesday. November 30, 2010.
We realized that while the patient has to know their risk, to understand "dynamic complexity" and its dangers for their ignoring their health until it is too late, and to avoid "shifting the burden" of responsibility from themselves to another, their healthcare providers have a responsibility to show them that if "they make a change that it will make a difference."
Facts:
- There are 12 Framingham Risk Scores
- To turn these scores into a tool for challenging patients with the premise, “If you make a change, it will make a difference,” you can add “What If Scenarios” to each
- But now you have 72 computations
- Can you get a provider to do all of these scores at every visit?
Remember our three questions: How important is it; how much time does it take; how much energy does it take? With electronics, we can make it easier to do it right than not to do it at all. Depending on the method, it can take 10 to 200 minutes to make these 72 computations, but with electronics the time can be reduced to one second. With team work, the time and energy on the provider can be reduced to zero.
The General Cardiovascular Disease 10-Year risk
This score projects the probability of a person having a major cardiovascular event such as a heart attack or stroke in the next ten years. The above patient‘s real heart age is 54 years but the relative heart age is 76 years (his health is deteriorating more rapidly than he is aging), and the 10 year risk is high at 25.3%. These are very discouraging number for a 45-year-old man. But now that we have added the -What If? section, we can assure this man that if he will make a change, it will make a difference. In addition, the greatest opportunity for improvement in his risk is indicated by the change in risk with each of the scenarios below.
- If he changes all of the elements in this calculation which are changeable (systolic blood pressure, cholesterol, smoking, hypertension treatment), his risk will improve. The unchangeable features are age, gender and diabetes.
- If he changes all of the elements to evidenced-based goals, his risk will drop to 9.4% and his relative heart age will drop from 80 years to 54 years. These are dramatic improvements in his risk. We can categorically assure him that -if he makes a change, it will make a difference.
- If he changes all of the elements by a 20% improvement, his risk will drop to 15.6% and his -relative heart age will drop to 64. Obviously these are not as good as the result of treating him to goal, but they are significantly improved.
- The changes for treating his blood pressure to goal without affecting the other elements shows a drop in risk as does changing the cholesterol. There is no improvement for smoking cessation in that it is noted that this patient does not smoke.

The second risk score is the Global Cardiovascular Risk Score, which is technically not a Framingham Calculator, but which was derived from the Framingham Data. It was developed in order to eliminate the unchangeable features such as gender and age which are so heavily weighted in the Framingham Calculators so that many young people with significant risk are overlooked and many elderly people with lower risk are still rated at a very high risk. In addition, while others of the calculators take into consideration whether the patient has diabetes or not, as diabetes is an independent risk factor for heart disease, the Global Cardiovascular Risk Score takes into account whether patients with diabetes are well controlled, or not, as is indicated by the hemoglobin A1C (HbA1c).
The elements in this score are HDL, Systolic Blood Pressure, HbA1C, packs per day smoking and total cholesterol. As can be seen, if all of these elements are treated to goal, the risk goes from 13.9 points to 0.5 points. It is possible to get some indication of the contribution of each element to the risk by seeing how the risk changes when only one of the elements is changed such as blood pressure, lipids or HbA1C. As is suggested by this review, the most important thing to control is your blood pressure.
Stroke Risk - What IF?
The final calculator for which the -What If? scenarios have been calculated is -stroke risk, which is shown on the template below. The elements of this calculator are:
- Age 55-84
- Systolic blood pressure
- Diabetes mellitus
- Cigarette smoking,
- Prior cardiovascular disease (CHF, MI, Peripheral Vascular Disease, Angina)
- Atrial fibrillation
- Left ventricular hypertrophy
- Use of hypertensive medication
The current calculation of 16% risk is shown and the improvement with each scenario is displayed. Of interest is that simply controlling the blood pressure achieves almost all the possible improvement, i.e., from 16% to 5%. And, there is no difference between a -20% improvement and -a treatment to goal, demonstrating that it is not necessary to be perfect in order to achieve significant improvement; said another way, -If you make a change - even a small change -- it will make a difference.
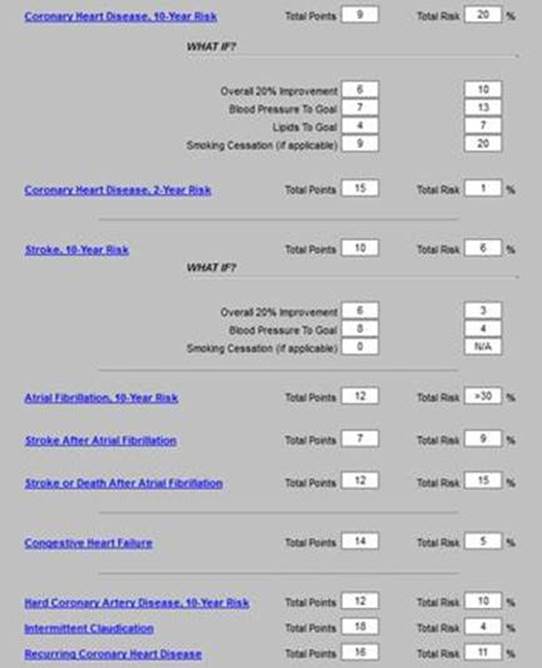
If a patient is going to make a change which will make a difference, there must be a basis on which change can be expected. We know that conversations at the time of an office visit are part of that decision to make a change. However, without a written, personalized plan of care and treatment plan, few patients will successfully make those changes and sustain them.
The -WHAT-IF? Scenarios described above will be added to patients‘ diabetes, hypertension and/or lipid plans of care and treatment plans. These documents are the -batons which are passed from one member of the healthcare team - your healthcare provider - to another member of the team - the patient. If the patient will study these documents, we believe it will encourage them to make changes and it is our confidence that those changes will make a difference. With the patient‘s name and personal data in each plan, the probability of their studying the material is greatly increased.
SETMA Tutorial For Use of Framingham Risk Calculators (the full 31-page tutorial can be found at http://jameslhollymd.com/EPM-Tools/pdfs/framingham-tutorial.pdf).
The SETMA Framingham Heart Risk Calculators can be found on the following Disease- Management Master Templates: Diabetes, Lipids, Hypertension, CHF, Acute Coronary Syndrome . and Chronic Stable Angina
This is an illustration taken from the Lipids Disease Management Tool:
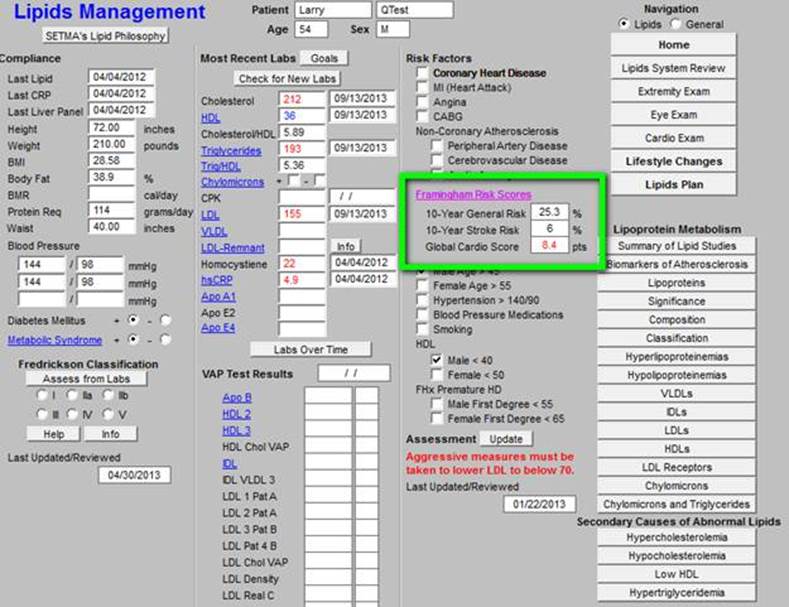
The three major Risk Score results - 10-Year General Cardiovascular Risk, 10-Year Stroke Risk and the Global Cardio Score -- are displayed on each master templates. When the button entitled Framingham Risk Scores is depressed on any of the above named master templates, the Framingham Heart Risk Calculator is launched. Without any other action on the provider‘s part, all twelve calculations are made. All data points are aggregated electronically for this purpose.
The following is the template which appears when the button entitled Framingham Risk Scores is depressed. It will be noted that the titles of each of the risk calculators is in blue. This means that each is a hyperlink and when depressed the elements on the basis of which the score is calculated is displayed.
This function is a useful teaching tool, as it is possible to review these elements with a patient when any score is being discussed. This will be a useful means of alerting patients to the changes they need to make in their lifestyles or treatment regimens in order to moderate their risk. The date that the Framingham Risk Scores were calculated and reviewed is noted at the top of the template.
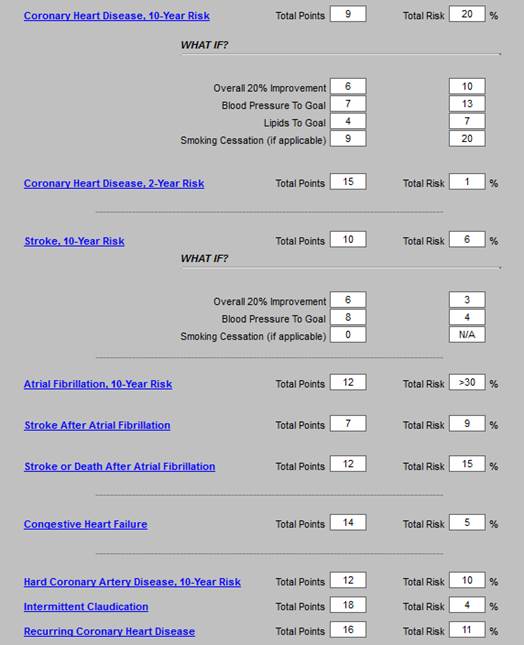
The remainder of this tutorial will be a review of the elements of each of the risk scores with an introductory statement for each, taken from the Framingham official website at www.framinghamheartstudy.org followed by SETMA‘s display of the risk elements when the hyperlinks above are launched.
In August, 2010, the American Family Physician (reference: Global Risk of Coronary Heart Disease: Assessment and Application, Anthony J. Viera, MD, MPH and Stacey L. Seridan, MD, MPH, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, North Carolina Am Fam Physician. 2010 Aug 1;82(3):265-274) made the following observations:
Coronary heart disease is the most common cause of death in the United States. The conventional risk factor approach to primary prevention excludes many patients who could benefit from preventive therapies. A global risk approach allows more accurate estimates of risk to guide clinical primary prevention efforts. Global risk of coronary heart disease is a calculation of the absolute risk of having a coronary heart disease event (e.g., death, myocardial infarction) over a specified period. It is based on an empiric equation that combines major risk factors, such as blood pressure and cholesterol levels. When physicians know a patient‘s global risk of coronary heart disease, they are more likely to prescribe risk-reducing therapies such as antihypertensives, statins, and aspirin. In addition, patients who know their risk level are more likely to initiate risk-reducing therapies. Many tools are available to estimate global risk, including several Web- based calculators. In the United States, tools based on the Framingham Heart Study are recommended.
(see: http://jameslhollymd.com/epm-tools/Automated-Team-Tutorial-for-the-EMR-Automated-Team-Function) - this link is to a tutorial for “The Automated Team”
These two illustrations are the foundation of what has come to be known as SETMA’s “automated team.” With automation, we can imitate Henry Ford, who automated the manufacturing of automobiles with assembly lines and in so doing made it possible for those who made cars to afford to drive them. There are many aspects of patient care which can be automated.
Classically, SETMA has used clinical decision support as reminders to providers, but now we are realizing that many of the tasks which were the object of CDS, actually could and should be automated, requiring no input from the provider. For instance, the value of the flu immunization is not enhanced by it being ordered by a healthcare provider, or by it being given by a registered nurse. And, the process of a flu immunization can be automated.
In June, 2013, the American Medical Newspublished an article entitled, “Serious work put into making primary care fun again.” With an anticipated serious shortage of primary care physicians over the next twenty years, the article addressed how to improve the lot of primary care providers, stating in part:
“Amid alarming rates of physician burnout, hundreds of clinics nationwide are redesigning their practices with a goal in mind beyond improving the quality of care. They are aiming to make life as a primary care doctor enjoyable once more. Twenty-three of these clinics...describe practice innovations that can ease the chaos, administrative overload, miscommunication and computerized busy work that too often characterize primary care.”
In 1993, John Patrick set IBM on another course and changed the company's future. Reading his story made me wonder, is it possible for SETMA to set medicine on another course and to change the future. John did not want people to work “collaterally,” side by side, maybe going in the same direction, maybe even having the same goal, but working independently and at best in a cooperative manner; he wanted people to work “collaboratively,” synergistically, leveraging the generative power of a team in creating a new future which they partially envision but which even they could not control.
What can we do today in healthcare which would mirror the changes IBM experienced? How can we change “collaterallists” into “collaborativists”? How can we use the power of electronics, analytics, and informatics principles to energize radical change to create a new future in healthcare? Testing and measurement is a science. In most industries, quality is determined by testing performance.
www.jameslhollymd.com
by James L. Holly, MD
You can find the website by clicking on the web address above and then clicking on the button entitled Transforming Your Practice (TCPI), outlined in green. The 21 following screen shots will navigate you through the materials available. All of this material can be used free of charge. The only limitations is that if you distribute and/or publish it with SETMA’s name attached, it cannot be change. However, any of this material can be adapted and/or integrated into your work without attribution.
This introductory document for TCPI is entitled:
Overview and the Philosophical Underpinnings to
SETMA’s Website (www.jameslhollymd.com) which is SETMA’s “Offer”
to the Center for Medicare and Medicaid Services’ (CMS)
Transforming Clinic Practice Initiative (TCPI)
This document can be found by clicking on Transforming Your Practice (TCPI) outlined in green above. The following screen shots show all of the categories available on SETMA’s website under Transforming Your Practice (TCPI). When each of the 21 buttons is clicked a list of tutorials, links, or descriptions and explanations of contents will appear. The following is a partial screen shot of this section and represents the Index which improves access to the material in this introductory section.

The first drop down after Transforming Your Practice (TCPI) is Summary Document of TCPI. With an extensive index, made up of hyperlinks to facilitate the accessing of all of the material, this document contains the materials on all of the 21 sections. These documents can be viewed individually by clicking on one of the buttons, or collectively by clicking on Summary Document of TCPI. This summary document and/or any of the sections can be printed for review or can be sent by an electronic link by e-mail to others.

This section contains materials produced during and/or in response to the CMS Quality Conference, December 1-3, 2015 in Baltimore, Maryland and during the TCPI potential faculty sessions held at that meeting. The material was distributed during the conference to many of those attending the potential faculty meetings.

The following is a screen shot of the beginning of the CMS Quality 12.2015 TCPI drop down.
This drop down menu contains material associated with SETMA’s Leadership and Governance principles. It was prepared for our successful completion of accreditation for Ambulatory Care and Patient-Centered Medical Home by the Joint Commission, URAC, Accreditation Association of Ambulatory Health Care (AAAHC) and National Committee for Quality Assurance (NCQA). It gives examples to other practices as to the importance of each of these issues in regard to practice organization and transformation. It can be accessed by clicking on the button outlined in green below.

The following is a screen shot of the Leadership and Governance section.
This section contains information about the organization, responsibilities and functions of a care coordination department. It can be found by clicking on the button outlined in green below. This department is critical to the transformation of traditional medical practices into a high function Patient-Centered Medical Home.

The following is a screen shot of this section of the TCPI materials.
To fulfill the responsibility of a transforming practice to patients and to Federal regulations and standards, HIPPA compliance and security measures are critical. This section introduces the importance and scope of this responsibility. A complete examination of this subject is beyond this presentation. The section can be found by clicking on the button outlined in green.

The following is a screen shot of the HIPPA and Security section of this material.
The power of analytics in the transformation of healthcare delivery and in the improvement of outcomes is critical. If you have a GPS service which tells you where you want to go but which does not tell you where you are, you can never get to your destination. Data Analytics helps you know where you are so that you can get to where you want to be. Remember Abraham Lincoln’s great quote: “If we can first know where we are and whither we are tending; we can better judge what to do and who to do it.” Data Analytics helps us face our “reality” which when measured against our “vision,” creates a self-sustaining “creative tension” which drives us to success. You can find the section on Data Analytics by clicking on the buttons shown below, outlined in green.
The following is a screen shot of the “Data Analytics” section.
The most important number in healthcare today is 8,760. It is the number of hours in a year. If a patients receives a great deal of healthcare, he/she may be in a provider’s presence for 30 hours a year; that leaves 8,730 hours in the year when the patient is in charge of his/her own care. Without care transitions, the patient will be lost. With patient activation, engagement, shared decision and with care coordination and transitions, the patient can sustain their healthcare initiative all year long.

The following is a screen shot of the Care Transitions section.
Less illness and more health was the goal which created the Less Initiative. It was one of the first major practice transformations which SETMA created. It can be found at the link outline in green below.

The following screen shot of the Less Initiative section of TCPI begin the introduction of this critical practice transformation initiative.
This section, found at the button outlined in green below, introduces practices to SETMA early medical record transformation in 1998-1999.

The title of the first link in this section shown in the screen shot below introduced an article which SETMA published as a booklet. It was distributed widely to our practice, patients, community and others and represented our Cortez Initiative – the declaration that there was not going back. We started with EMR, we changed to EPM and we were going to succeed not matter the cost or effort required.
Once SETMA morphed from EMR to EMP (electronic patient management), disease management tools and clinical decision support became the backbone of our work. This section can be found by clicking on the button outlined in green below.

The screen shot of Clinical Decision Support seen below introduces the ideal of EMR and EPM which requires that electronics make tasks easier to perform and to audit.
One of the most significant deficiencies of ambulatory, electronic health records is the isolation of ambulatory care from inpatient care. SETMA’s hospital care tools. Few things represent the power of a team as SETMA’s history in the hospital. Since January 1, 2007, SETMA has discharged 18,952 distinct patients from the hospital, which represents 39,340 distinct instances of discharges/encounters as of today. That is an average of 2,000 distinct patients a year and 4,371 annual admissions. The Hospital Care Summary and the Post Hospital Plan of Care and Treatment Plan (the discharge summary (this name was changed at an NQF, Transitions of Care conference in September, 2010) was completed at the time of discharge on 96.5 percent of the discharges/encounters at the time of the discharge. I would like the percentage to be higher but this is not a bad number. For the hospital, this means no “held charges,” and effective transitions of care with all follow-up care, medication reconciliations and readmission risks determined before the patients leave the hospital. This is not the work of solitary physicians working by themselves but it is the work of a team. This is the results of SETMA’s Hospital Care Tools and of SETMA’s Hospital Care Team.
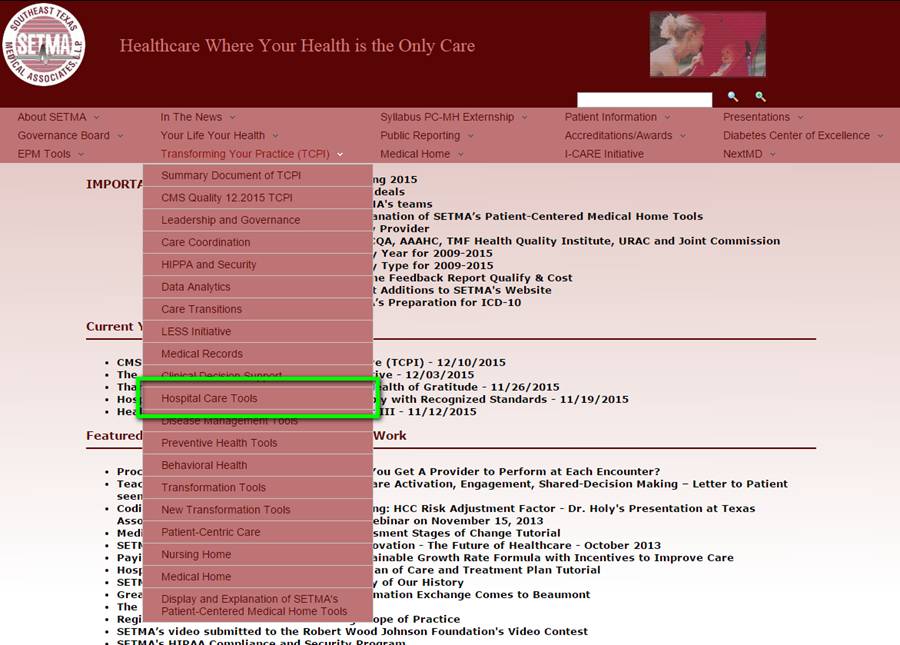
The following is a screen shot which introduces the Hospital Care Tools. The screen shot shows how SETMA addressed many issues in the hospital including “how nomenclature can obscure function.”
These tools are not just “how to” in using electronic functions but they are also lessons in disease natural history and in best practices in how to improve the overall health of patients while addressing specific illnesses. They provide the ability for providers to measure their quality performance at the point of care and they make it efficient to create treatment plans and plans of care.
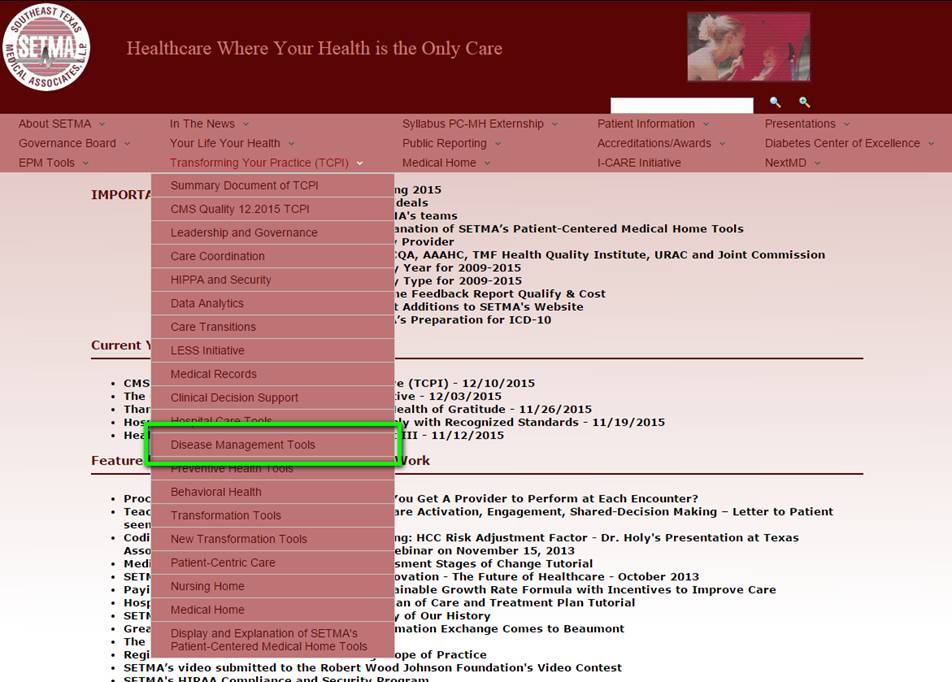
The following is a screen shot of the Disease Management section.
The foundation of effective preventive care is “hope.” The following link gives a more detailed explanation of this last statement: Value, Virtue, Trust and Hope - The Foundation of Health Improvement. Without a sense of person value and personal virtue from which comes the capacity to trust, the result of the coexistence of these three, hope, will not exist. And without “hope” individuals will not take the steps and make the changes for the power and potential of preventive medicine to improve health.
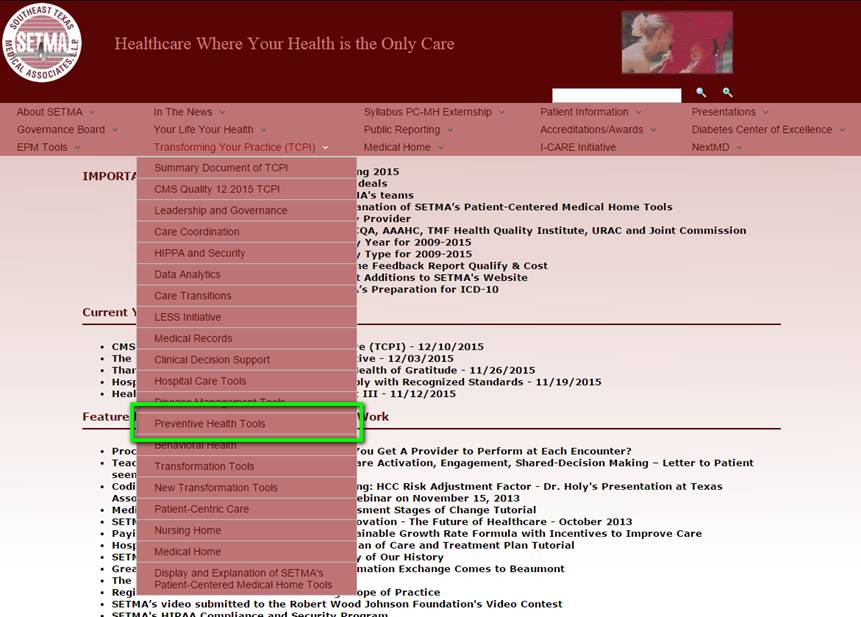
The following is a screen shot to the section on Preventive Health Tools.
This section is a discussion of SETMA’s efforts in Behavioral Health which are growing rapidly. According to the World Health Organization (WHO) mental health includes "subjective well-being, perceived self-efficacy, autonomy, competence, intergenerational dependence, and self-actualization of one's intellectual and emotional potential, among others.: WHO further states that the well-being of an individual is encompassed in the realization of their abilities, coping with normal stresses of life, productive work and contribution to their community. However, cultural differences, subjective assessments, and competing professional theories all affect how "mental health" is defined. A person struggling with his or her behavioral health may face stress, depression, anxiety, relationship problems, grief, addiction, ADHD or learning disabilities, mood disorders, or other psychological concerns. Counselors, therapists, life coaches, psychologists, nurse practitioners or physicians can help manage behavioral health concerns with treatments such as therapy, counseling, or medication. The new field of global mental health is "the area of study, research and practice that places a priority on improving mental health and achieving equity in mental health for all people worldwide."

The following is a screen shot of this section.
Does the distinction between reformation and transformation of the healthcare system really make a difference? In order to examine this question, we must define our terms. The definition of "reformation" is "improvement (or an intended improvement) in the existing form or condition of institutions or practices etc.; intended to make a striking change for the better in social or political or religious affairs." Synonyms for "reformation" are "melioration" and "improvement." Another definition states, "The act of reforming, or the state of being reformed; change from worse to better."
On the other hand, "transformation" is defined as, "a marked change in appearance or character, especially for the better." "Metamorphosis," a synonym for "transformation," is the transliteration of a Greek word which is formed by the combination of the word "morphe" which means "form," and "meta" which means "change." "Metamorphosis" conveys the idea of a "noticeable change in character, appearance, function or condition." Metamorphosis is what happens when a caterpillar morphs into a butterfly.
In function, the distinction between these two concepts as applied to healthcare is that "reformation" comes from pressure from the outside, while "transformation" comes from an essential change of motivation and dynamic from the inside." Anything can be reformed - reshaped, made to conform to an external dimension - if enough pressure is brought to bear. Unfortunately, reshaping under pressure can fracture the object being confined to a new space. And, it can do so in such a way as to permanently alter the structural integrity of that which is being reformed. Also, once the external pressure is eliminated, redirected or lessened, the object often returns to its previous shape as nothing has fundamentally changed in its nature.
Being from within, transformation results in change which is not simply reflected in shape, structure, dimension or appearance, but transformation results in a change which is part of the nature of the organization being transformed. The process itself creates a dynamic which is generative, i.e., it not only changes that which is being transformed but it creates within the object of transformation the energy, the will and the necessity of continued and constant change and improvement. Transformation is not dependent upon external pressure but is sustained by an internal drive which is energized by the evolving nature of the organization.

This section is placed here for new tools which we develop. The first tutorial which will be deployed here will be the Chronic Conditions Management Tutorial which is complete but will be posted to the website soon.

Many ideas are new to the “old” way of practicing medicine: coordination, transitions, activation, engagement, shared-decision making, but nothing is newer than the concept of “patient-centric care.” This section is designed to introduce concepts like patient-centric conversations and other equally novel concepts.

The following screen shot of this section alerts the provider to some of the challenges for practice transformation.
This section introduces special tools for this unique care delivery site. Five problems are identified as the most complex and difficult and solutions are identified and described.

The following screen shots introduces the Nursing Home tools designed by SETMA.
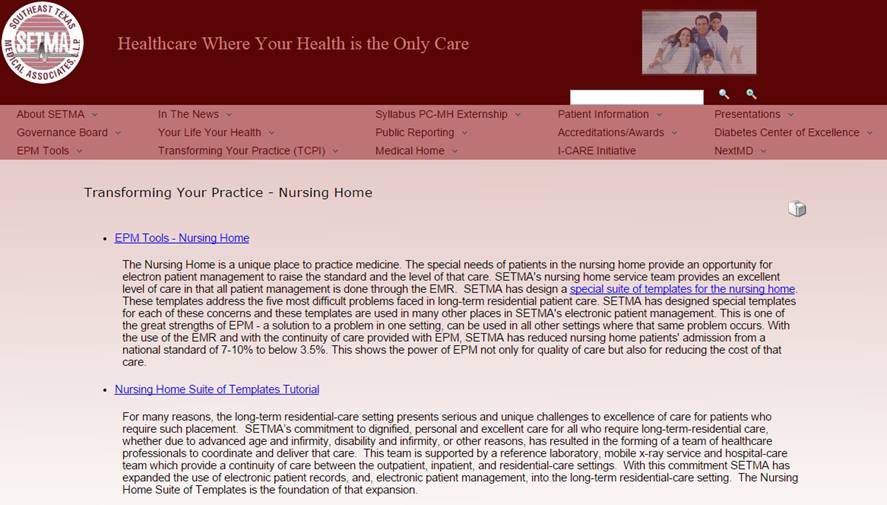
Stories, ideals, details and designs for Patient-Centered Medical Home are part of healthcare transformation and part of the TCPI.
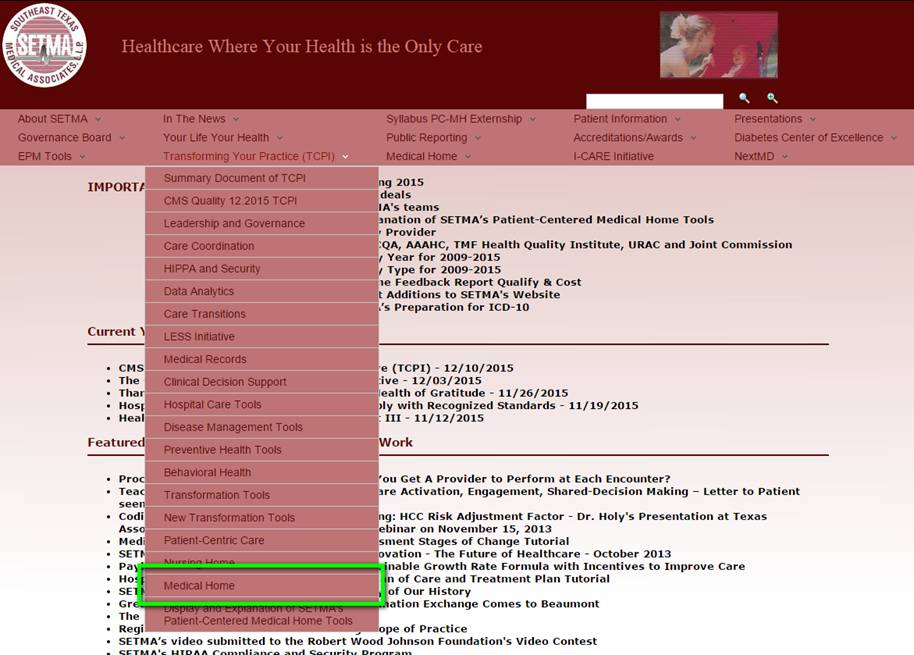
The following is a screen shot for the Medical Home section of this site.
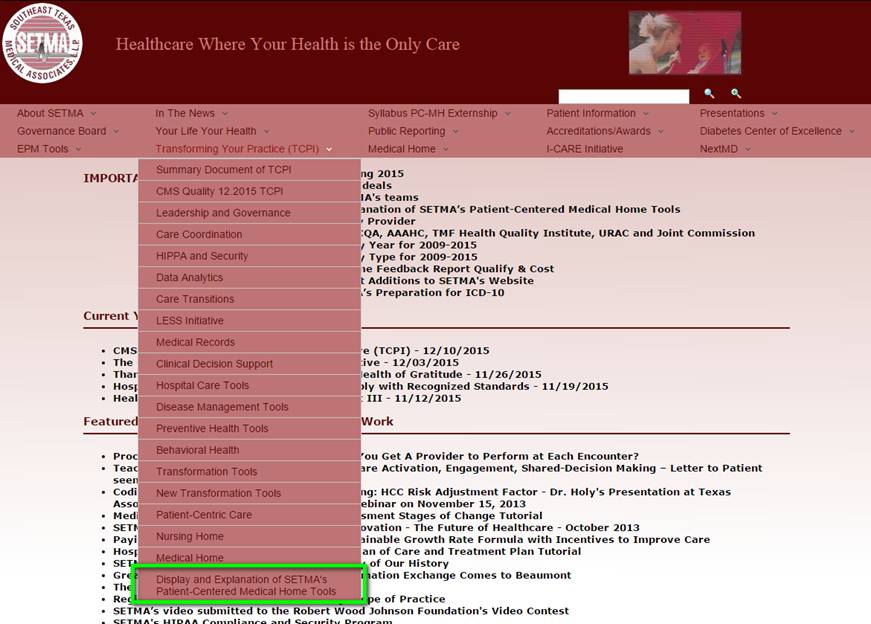
There is some redundancy here but a different organization makes access to these concepts easier. This is a screen shot for this section.
|