|
Beginning in 2019, all physician payments from the Centers for Medicare and Medicaid (CMS) will be made on the basis of a new system called MACRA (Medicare Access and CHIP Reauthorization Act of 2015) and MIPS (Merit-Based Incentive Payment System). Why should you care? An ongoing discussion is being had over how many healthcare providers with stop seeing Medicare and Medicaid patients and how many, out of frustration, will simply retire. The providers who will not care are those who have refused to care for our poor and elderly and who have built practices without caring for these groups.
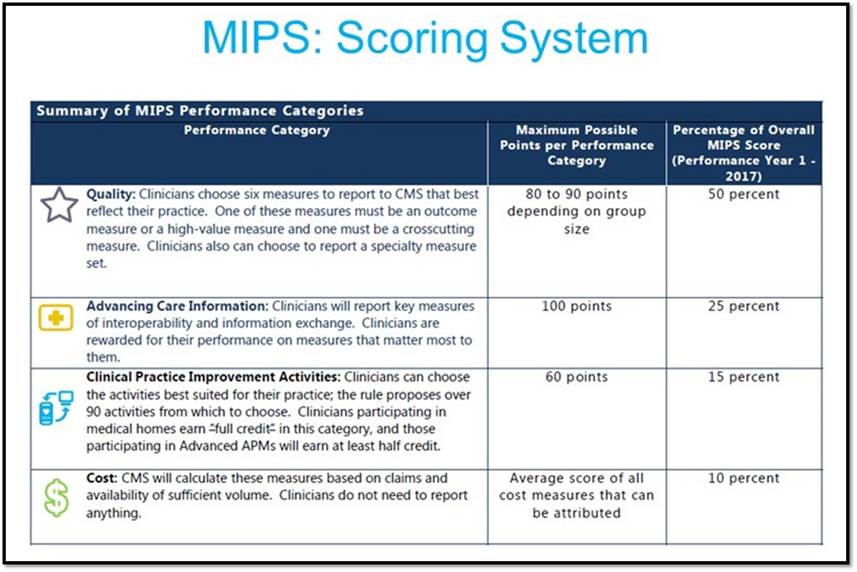
The new payment mode will be based on a healthcare provider “composite performance score” (CPS). This score will be made up of the following percentages in the first year: quality (50%), resource use (10%), advanced care information (25%), and clinical practice improvement activity (15%).
To understand the complexity and the anxiety of this new program review the following formula by which a providers CPS will be calculate by CMS with the following eight factors:
CPS = [(quality performance category score x quality performance category weight) + (resource use performance category score x resource use performance category weight) + (CPIA performance category score x CPIA performance category weight) + (advancing care information performance category score x advancing care information performance category weight)] x 100.
What SETMA Has Been Doing over Past 21 Years to Prepare for MACRA and MIPS
If the above formula doesn’t cross your eyes, you didn’t read it. The good news is that SETMA has been working for 21 years toward this time.
- We have participated in the Physician Quality Reporting System (PQRS) since its foundation.
- We have used a certified electronic medical records system (EMR) for seventeen years.
- We have been a certified patient-centered medical home (PC-MH) from 2010 through 2019.
- We have publicly reported on over 250 quality metrics (CQM0 by provider name for eight years and have been tracking quality for seventeen years.
- We have tracked ACO, HEDIS and MA Advantage quality metrics for over ten years.
- We have fulfilled the Meaningful Use standards, also.
But even with all of this, it is uncertain how we will fair due to the one issue of “resource utilization”. Quality, Screening and Preventive care are not inexpensive. It is unclear at this time whether quality, safety and cost of care will be at cross purposes, such that as quality goes up cost also increases. In addition, other than a study which CMS conducted on our practice in 2011 (see: Medical Home Feedback Report). In this study we did very well on “resource utilization,” we do not know and we actually cannot know how our “resource utilization” will be judged.
SETMA made a recent assessment of our preparedness for MACRA and MIPS
Payment adjustment made up of four parts shown below.
- Quality - This will be gleaned from the Clinical Quality Measures (CQMs) that SETMA reports to CMS. CQM is the new PQRS. Measures are physician selected and SETMA has many good ones to report.
- Advancing Care Information - This is the next phase of Meaningful Use. All of SETMA providers meet these measures and will continue to do so.
- Clinical Improvement Activities - “Clinicians recognized as a Tier III Medical Home by NCQA earn full credit in this category.” SETMA is accredited for Patient-Centered Medical Home by NCQA at their highest level (Tier III) and by three other agencies as well.
- Cost - The will be gleaned off of claims data. There is nothing to do on our part for this.
So, in summary, SETMA appears to have all of the pieces under control already according to the following description.
MACRA and MIPS
In order to understand the new payment system which is going into effect in 2019 but which will be based on provider performance in 2017, it is important to under the terminology. The following table gives definitions which are critical to this understanding.
| Old Acronym |
Term |
Description |
| MU |
Meaningful Use |
The Medicare EHR incentive program is now a component of MIPS and is called Advancing Care Information (ACI). |
|
Eligible Professional |
What we used to call an eligible professional under Meaningful Use is now called Eligible Clinician (EC) within MIPS. |
New Acronyms
| Acronym |
Term |
Description |
| MACRA |
Medicare Access and CHIP Reauthorization Act of 2015 |
A new business model focused on value based care. MACRA, replaces the Sustainable Growth Rate formula by paying clinicians for the value and quality of care they provide. MACRA created the Quality Payment Program. |
| QPP |
Quality Payment Program |
The single framework under which MIPS and APMs are administered. The goals of the QPP are described below. |
| MIPS |
Merit-Based Incentive Payment System |
Incentive program aligning old models into a single model made up of components. |
| CPS |
MIPS Composite Performance Score |
A clinician’s total MIPS score (a singular number) which is comprised of four scores from four weighted categories. |
| QP |
Qualifying APM Participant |
Someone that participates in an advanced APM model at a higher threshold. |
| APM |
Advanced Alternative Payment Models |
The QPP creates additional incentives for Qualifying Professional’s (QP’s) who participate in an Advanced Alternative Payment Models. It does not create the APM or alter the structure of APMs. |
The overarching goal
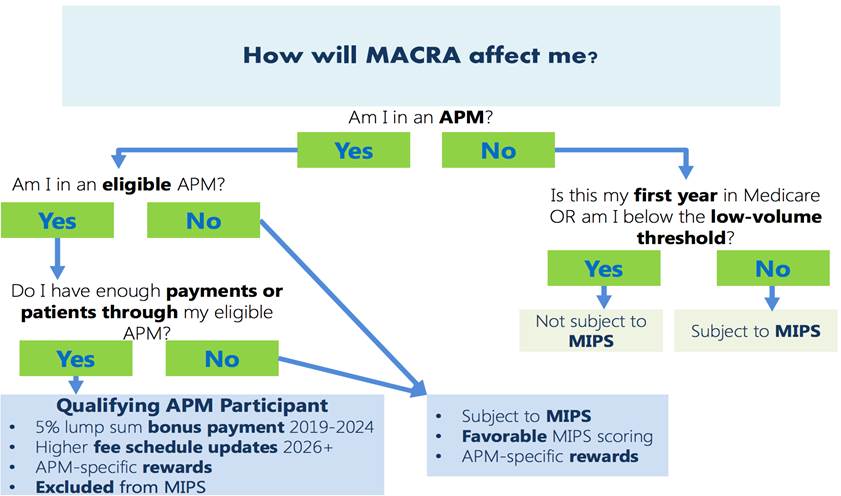
The goal of CMS is to increase the focus on quality and value-based care. By the end of 2016, CMS plans to tie 30% of Medicare payments to alternative payment models and to tie 85% of fee-for-service payments to quality. To do that, the Quality Payment Program has been created and has two branches. Clinicians will either participate in MIPS or an APM. Most clinicians will be subject to MIPS. Clinicians will be excluded from MIPS if they meet a low volume threshold, are in their first year of Medicare Part B Participation, or if they participate in the other branch of the quality payment program, an advanced alternative payment model (APM).
What is MIPS?
MIPS is a single incentive program that streamlines three current programs within it: the physician quality reporting system (PQRS), Value Based Payment, and the Medicare EHR incentive program for eligible professionals (Meaningful Use for EP). It is important to note that the EHR incentive program for hospitals will continue; MIPS does not apply to hospitals.
Also, the Medicaid EHR incentive program for eligible professionals will continue. MIPS will take effect in 2018 and MIPS begins adjusting payments in 2019. The fourth component of MIPS is new; Clinical Practice Improvement Activities.
The following chart explains how healthcare providers can be rewarded up to 9% of their total reimbursement from Medicare/Medicaid or penalized up to 9%.
MIPS is comprised of four Performance Categories which make up a composite performance score (CPS) of a possible 100 points. Clinicians can submit their individual score or a score for their entire group. The four performance categories are Quality, Resource Use, Clinical Practice Improvement Activity, Advancing Care Information. CMS will report the physician’s score publicly on Physician Compare.
In 2017, groups will report year’s worth of data to CMS so a national threshold can be calculated. This is the MIPS performance threshold and it will be used as comparison to a clinician's MIPS composite score (CPS) when determining the appropriate payment adjustment in year 2019. Clinicians with a CPS higher than the national performance threshold will receive an upward adjustment of MPFS payments (up to 4% in 2019, increasing to 9% by 2023), while a physician whose CPS is below that threshold will be subject to a corresponding downward adjustment.
What is an APM?
Advanced Alternative Payment Models (APMs) are defined by CMS as new approaches to paying for medical care through Medicare that incentivize quality and value. MACRA doesn’t create new Advanced Alternative Payment Models. Just as MACRA created MIPS, a program to change the reimbursement model, that’s the exact goal of MACRA under APMs as well; additional incentives for APM participation.
Although the majority of clinicians will be subject to MIPS, those that participate in Advanced Payment Models at a certain threshold, such as Accountable Care Organizations, will be excluded from the MIPS program. To be considered as an APM, at least 50% of the participating clinicians must use a certified EHR technology. This threshold increases to 75% after year one. The group must also base payment on quality measures comparable to those in the MIPS program.
Finally, APM entities are required to bear more than nominal financial risk. Eligible Clinicians can become Qualifying APM Participants if a certain percent of their patients or payments are through an APM. QP’s are eligible for a 5% lump sum bonus in years 2019 - 2024 and even higher in subsequent years. Only QP’s are excluded from MIPS.
|