|
Appendix H
What does it mean to you that SETMA is a Medical Home?
RI.01.04.03 The Organization Provides Patients with information about the functions and services of the Primary-care Medical Home.
What does it mean to you that Southeast Texas Medical Associates, LLP (SETMA, www.jameslhollymd.com) is a “medical home”? First, it means that SETMA has voluntarily been subjected to rigorous standards and examination by:
- The National Committee for Quality Assurance (NCQA -- http://www.ncqa.org/Programs/Recognition/PatientCenteredMedicalHomePCMH.aspx) and has received the highest designation, Tier III, for 2010-2013 and 2013-2016.
Medical Home News - Spreading Medical Home Concepts Beyond Primary
Care
- The Accreditation Association of Ambulatory Health Care ((AAAHC -- http://www.aaahc.org/accreditation/primary-care-medical-home/) and has received the highest designation by AAAHC for 2010-2011, 2011-2014.
Medical Home News - Keep Calm and Become a Medical Home
- URAC (Known only as URAC -- https://www.urac.org/accreditation-and-measurement/accreditation-programs/all-programs/patient-centered-medical-home-achievement/) and has received the highest designation as PCMH Certification with Electronic Health Records. Both AAAHC and URAC included multiple-day, on-site visits.
Medical Home News - The URAC PCMH Practice Achievement Program
- March 3-5, SETMA will be surveyed by the Joint Commission for ambulatory care and patient-centered medical home -- http://www.jointcommission.org/accreditation/pchi.aspx.
Medical Home News - The Joint Commission Primary Care Medical Home
Certification Program
SETMA was successful in the Joint Commission survey, making SETMA the only practice in the United States, and for that matter in the world, which simultaneously possesses recognition and/or accreditation by all four organizations which evaluate practices for medical home. Even with this remarkable achievement, we continue to learn about medical home and about how to serve our patients better with this remarkable method of healthcare delivery.
Second, it means that fifteen years ago, in May, 1999, SETMA began transforming the care SETMA’s patients receive by defining ten principles on the basis of which our use of electronic health records (EHR) would be built. That month, SETMA published a booklet entitled, More Than a Transcription Service: Revolutionizing the Practice of Medicine: And Meeting the Challenge of Managed Care With Electronic Medical Records (EMR) which Evolves into Electronic Patient Management. This booklet was SETMA’s declaration of our intent of transformation healthcare delivery with electronic health records (EHR). Before the federal concept of “meaningful use” of EHR was published, SETMA was about the process of “using the EHR meaningfully.”
Based on Peter Senge’s “systems thinking,” (see Designing an EMR on the Basis of Peter Senge's The Fifth Disciple by James L. Holly, M.D.), these principles stated that SETMA would:
- Pursue electronic patient management rather than electronic health records, leveraging the power of electronics to improve individual and population health.
- Bring to bear upon every patient encounter that which is known rather than what an individual provider knows.
- Make it easier to do it right than not do it at all.
- Continually challenge providers to improve their performance.
- Easily infuse new knowledge and decision-making tools throughout an organization.
- Promote continuity of care with patient education, information and plans of care.
- Enlist patients as partners and collaborators in their own health improvement.
- Evaluate the care of patients and populations longitudinally.
- Audit provider performance based on the Consortium for Physician Performance Improvement (PCPI) Data Sets. (Other measure sets have been added since then)
- Create multiple disease-management tools which are integrated in an intuitive and interchangeable fashion giving patients the benefit of expert knowledge about specific conditions while they get the benefit of a global approach to their total health.
Third, ten years later on February 16, 2009, with the tools which had been developed in the interim, SETMA began the formal process of transforming your care into a Medical Home model. In 2009, 2010, 2011, SETMA published three series of articles which described and defined medical home and which documented our progress toward being a medical home. (see 2011 Medical Home Series Two).
A Partial List of Services Available in your Medical Home
Being a patient in SETMA’s patient-centered medical home means you have access to a wide range of other clinical support services. These services include:
- Dietary Education through SETMA’s American Diabetes Association approved Diabetes Self Management Education program. SETMA’s education department also trains patients in dietary weight management, cholesterol control, the Dietary Approach to Stopping Hypertension (DASH), Renal Dietary management, and others.
- Cardiovascular Laboratory in which you can be tested for heart disease with stress test, dobutrex stress test, echocardiograms, arterial Doppler, carotid Doppler, holter monitors, etc.
- Pulmonary Function testing
- Bone Densitometry for osteoporosis
- Allergy Testing
- Cardiovascular Risk Stratification with Carotid Intima Thickening testing
- Ultrasonography for abdomen, pelvis, venous, oeripheral vasculature, etc.
- Laboratory services - SETMA’s reference laboratory provides an extensive array of testing, all of which are link with the electronic medical record.
- Radiologic services including Mobile x-ray
- Physical Therapy which provides state-of-the-art to all patients for cardiac rehab, conditioning and all other modalities of physical therapy.
- Infusion Center
- Specialty Diabetes care through the Diabetes Center of Excellence at Southeast Texas Medical Associates.
The Mission of Your Medical Home
The mission of SETMA and now of SETMA as a medical home was formalized into SETMA’s Mission Statement inn 1997. It states: “To build a multi-specialty clinic in Southeast Texas which is worthy of the trust of every patient who seeks our help with their health, and to promote excellence in healthcare delivery by example.” A framed copy of this statement is displayed in all public places within SETMA’s clinics. The statement is supported by SETMA’s:
Public Motto: Healthcare Where Your health is the only care
Private Motto: We want to do good while we do well
The Vision of Your Medical Home
SETMA’s medical home’s vision is to participate in the transformation of healthcare in the United States. This means that we understand that “transformation” comes from an internal, generative passion which drives us beyond the requirements of “reform” which is based upon regulations, rules and requirements. SETMA’s vision is defined by our wiliness to face our current reality and our willingness to honestly and straightforwardly face the gap between our reality and our vision.
In his book, The Fifth Discipline, Peter Senge addresses “creative tension” as that which is created by the difference between our reality and vision. Our ability to hold that creative tension between our reality and our vision is the force which will drive us to the successful achievement of our mission, the reaching of our goals and the fulfillment of our vision.
In reality because of transformation and generative passion which is internalized our vision will continually expand and change. Our vision is a society in which all have access to excellent healthcare, in which healthcare is seen as a human right. It includes our collaboration with our patients as team members on their healthcare team where the patient is activated, engaged and participating in shared-decision making. It is a healthcare delivery system which is coordinated and integrated, and which is sustainable financially.
The Goal of SETMA’s and of Your Medical Home
The Goal of SETMA’s medical home – of YOUR medical home – is to fulfill both the Triple Aim as defined by the Institute for Healthcare Improvement (IHI) and the Moral Test of Healthcare delivery as defined by Vice-President Hubert Humphrey in September, 1977. The “Moral Test” of government is: “How that government treats those who are in the dawn of life, the children; those who are in the twilight of life, the elderly; and those who are in the shadows of life, the sick, the needy and the handicapped.” While this was defined as the “moral test of a government,” SETMA has adopted this as the test by which we measure our standards of care and of conduct.
In 2007, the IHI launched the Triple Aim Initiative which includes the “simultaneous pursuit of three aims”:
- Improving the experience of care
- Improving the health of populations
- Reducing per capita costs of health care”
IHI defined a set of components of a system that would fulfill the Triple Aim. Five of the components are:
- Focus on individuals and families
- Redesign of primary care services and structures
- Population health management
- Cost control platform
- System integration and execution”
It is in pursuit of the Triple Aim before and after we learned of it, that SETMA has been redesigning primary care’s service and structures. In reviewing the ten principles of EHR design and of practice design in 1999, it can be seen by while we did not know the principles of the Triple Aim, we intuitively were pursuing those goals since our origins.
What Does the Medical Home Mean to You?
Essentially, the medical home model means that you are no longer a passive recipient of healthcare instructions from a healthcare provider, but you are now an active participant in your own care. Viewed as a “race,” your health-care is yours to run. Viewed as a “baton” in a relay race, you will carry your baton for the majority of your life. With 8760 hours in a year, and with your formal healthcare received from a healthcare provider occupying fewer than twenty hours a week, you are in charge of your care for over 8740 hours a year.
SETMA being a medical home means that your care will be “coordinated”, i.e., you will know where, when and how to obtain the care you and your provider have determined that you require. It means that you will receive a plan of care which is more than a prescription and a follow-up visit. It means that in a process called “shared-decision making,” you and your SETMA provider agree upon comprehensive steps to retain or regain your health. It means that because active learning is the only effective way for you to participate in your own healthcare decision making, your “activation” occurs when you gain the knowledge and skills needed. This is called “activation,” after which you become “engaged” in your care.
The foundation of this new dynamic is the patient-centric conversation in which you and your provider discuss your healthcare concerns and needs in a dialogue which is an active process rather than the traditional monologue where you passively received information and instructions. Under the old model of care, which might be referred to as a “paternalistic” healthcare system, you were very often told what to do and it was expected that you would follow the healthcare providers’ instructions without modification.
“Paternalism” meant “treating you in a fatherly manner, especially by providing for your needs without giving you rights or responsibilities.” The medical home redefines your relationship with your provider and changes how you relate! Rather than healthcare encounters being didactic (to lecture or teach, as one with knowledge instructions or informs), where the healthcare provider tells you what to do, how to do it and when to do it, the patient-centric encounter becomes a dialogue (an exchange of ideas or opinions) - where you and your provider discuss mutual concerns and together come to a conclusion with a mutually agreed upon plan. This new relationship is somewhat like a partnership.
The concept of a patient encounter being a dialogue where your interests and desires are respected is alien to the old paternalistic model of care. The only way in which the patient-centric conversation in a healthcare encounter can be a dialogue is where you and your provider become collegial and where you both enter into a collaborative relationship.
As we transformed our ambulatory practice into a PC-MH, we began to understand that your convenience and satisfaction were important aspects of healthcare transformation. In August of 2010, SETMA struggled with whether “patient convenience” was a worthy goal. As we formed our Department of Care Coordination, we began to realize that “coordination” meant scheduling which translates into:
- “Convenience for the patient which
- “Results in increased patient satisfaction which contributes to
- “The patient having confidence that the healthcare provider cares personally which
- “Increases the trust the patient has in the provider, all of which,
- “Increases compliance (adherence) in obtaining healthcare services recommended which,
- “Promotes cost savings in travel, time and expense of care which
- “Results in increased patient safety and quality of care.”
It is your right to have your care coordinated for your convenience and as a result, it is your responsibility to be engaged in your care. That not only means that you adhere to the plan you have developed in collaboration with your healthcare provider but that you are involved in developing your healthcare plan of care and treatment plan.
Part of that plan is seeking the counsel and collaboration with other healthcare provider when needed through a “referral process.” The “referral process” does not just mean choosing a provider from who a referral will be obtained, but also it means you keeping the appointment for the consultation requested by the referral and it means that your medical home will track that process to make sure that:
- The referral request is completed according to standards of excellence
- The consultant receives your healthcare information which supports his/her ability to give you the maximum benefit from the consultation.
- The consultants notes and conclusions are included in your primary care providers’ electronic health record.
- The recommendations of the consultant are incorporated into your plan of care and treatment plan after discussion with you.
Welcome to your medical home. This is what you can and should expect. It is new and it is hard work for you and for us. We believe that in the medical home your care will improve, your satisfaction with your care will improve and the effectiveness and safety of your care will improve. We still have a great deal to learn, but together we will learn and we will transform healthcare.
Your rights in your medical home
In your medical home, you have the right to choose your primary-care provider and/or to change that provider if you so choose. SETMA, as a medical home, will help you with the decision making about whom you will select as your primary-care provider including discussions about your preference as to gender, age, degree or training and scope of practice.
In fact, you both have the right and the responsibility to participate in decision making about your health and your health care, which in the medical home is referred to as “shared-decision making.” You have the right and the responsibility to select the specialists whom you need to see so that your desire is followed as to whom you do see.
The following lists your right:
- to be treated with respect, consideration and dignity, free from any abuse or harassment
- to be provided appropriate privacy
- to have records and disclosures treated confidentially and, except when required by law, to have the opportunity to approve or refuse the release of your records
- to be provided, to the degree known, complete information concerning your diagnosis, treatment and prognosis. When it is medically inadvisable to give such information to a patient, the information is provided to a person designated by the patient or to a legally authorized person
- to have the opportunity to participate in decisions regarding your health care
- to be informed about procedures for expression complaints and grievances, including those required by state and federal regulations
- to see a specialist if you request to see one and/or if your primary care provider determines that the seriousness of your care requires such.
- to ask for and receive a second-opinion about your diagnosis and/or plan of care
- to receive treatment for pain management. The prescription of pain management narcotics will be done in compliance with Texas Medical Board Rule 170. You have a right to review of copy of this Rule which may be obtained from the Board’s website or from your SETMA provider.
- to receive a written response to a written complaint which you lodge against a practice or a provider.
- to have information available to patients and staff concerning
- patient rights
- patient conduct and responsibilities
- services available at the organization
- provisions for after-hours and emergency care
- fees for service
- payment policies
- the right to refuse participation in experimental research
- advanced directives
- credentials of health care professionals
Just as your medical home has the responsibility to be guided by your rights and to fulfill the goals of your rights, you have responsibilities to your medical home and to your healthcare provider. As a patient you have the responsibility:
- To actively participate in the formulation of your plan of care and treatment plan, including sharing in the decision making about your care. This responsibility is key to your healthcare being delivered in a medical home.
- To become an “activated” patient by learning what is necessary for you to know in caring for your health.
- To become an “engaged” patient by assuming responsibility for your care.
- To engage in a conversation with your healthcare provider where you address all of your concerns.
- To notify other treating clinician (s) of your participation in the Medical Home and of your desire for the other clinicians to communicate with your Medical Home of your health needs as assessed by you and the other clinician (s).
- To adhere to the plan of care and/or treatment plan which you participated in establishing and with which you agreed to participate.
- To recognize that your failure to adhere to your treatment plan and/or plan of care may result in treatment failure and/or with the worsening of your health.
- To notify your provider, preferably in writing, if you determinate that you are unable or unwilling to adhere to your plan of care or treatment plan.
- To notify your provider, preferably in writing, if a barrier to your adherence to your plan of care or treatment plan exists and/or if you have determined that you cannot or will not follow your plan.
- to make full and complete disclosure of your medical history, medications including over the counter and dietary supplements, allergies and symptoms before and during the course of treatment
- to accept personal financial responsibility for charges not covered by his/her insurance
- to respect the rights of other patients, the health care providers and staff
- to understand your health problems to your satisfaction
- to notify your doctor about any unexpected changes in your health
- to follow the treatment plan prescribed by his/her provider
- to inform his/her provider about any living will, medical power of attorney or other directives that could affect care
How to contact your medical home
In a patient-centered medical home, there are multiple ways in which to contact your healthcare provider:
- You can make an appointment
- You can text your provider. (See part IV of this series as to how to send an encrypted text which is HIPAA compliant.)
- You can access SETMA’s web portal in order to send a secure e-mail to your provider.
- You can call your provider at the office or through the answering service. Remember, there are multiple people available for your healthcare needs 24 hours, seven-days a week.
Some providers will give you their personal cell phone number which allows you to contact them directly. As the CEO of SETMA, I have found that patients do not abuse the privilege of having this direct contact.
The new phenomenon, with which SETMA disagrees called “concierge medicine,” has the patient paying a premium to the doctor, sometimes as much as $2,000 a year for this privilege. In your medical home, if you would feel more secure, ask your provider if he/she will give you their cell phone number. Reward this privilege with the courtesy of not abusing it.
You can also contact your medical home by:
- Dropping by the office. You are always welcome at your medical home.
- Other providers can contact your medical home through SETMA’s Health Information Exchange which will also give you a means of proving your healthcare information to providers other than your primary care provider.
If you choose to contact your provider by texting, the below is a statement from Apple about its inability to comply with government request for data due to iMessage traffic being encrypted:
“….conversations which take place over iMessage and FaceTime are protected by end-to-end encryption so no one but the sender and receiver can see or read them. Apple cannot decrypt that data.”
Wikipedia’s article about iMessage states:
“Every connection has its own unique code, which acts as an identifier for the route that should be used to send a message to a specific device. The connection is encrypted with TLS using a client side certificate, which is requested by the device on the activation of iMessage.”
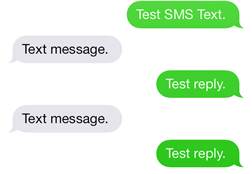
IMessage traffic is encrypted, only readable for the two end users and is therefore HIPAA compliant. You can tell when a message is being sent using iMessage because it will show in blue and not green.
Blue = iMessage = encrypted, is HIPAA compliant and is Ok to use for healthcare information
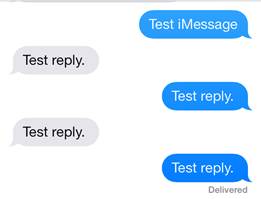
Green = SMS = is not encrypted, is not HIPAA compliant and is not OK for healthcare information.
Group Texting
If you send a group message to 10 people and 9 of them have iPhones setup with iMessage and one has SMS. The texting will send it to all of them as SMS. Don’t do this. Encryption only works from iPhone to iPhone, and your iPhone needs to be setup to use iMessage.
- Go to Settings > Messages > and
- Make sure iMessage is turned on.
It is up to you but you can also turn “Send as SMS” off. This would act as a safety net in case you sent a text to someone that did not have iMessage it would not send it as text. There are instances when due to poor signal your phone could choose to send something as SMS as opposed to iMessage. Messages are only HIPAA compliant if it is sent using iMessage.
Remember:
- This only works from iPhone to iPhone. If one person does not have a iPhone it will not be encrypted.
- You will not have a saved copy of this texting – so for orders from a physician or NP to an RN or LVN, it should always be e-mail so that we have a permanent copy. It texting is used, the text should be copied and with a time and date stamp placed in the patient’s chart.
- If you must text and if it is important that you keep a copy – you can copy the text put it into an e-mail and send it to yourself. Just make sure you put a Subject line which will allow you to search for the e-mail.
- Text will not have a subject or a source unless you type your name, no one will know who sent the text.
Your Satisfaction with care in SETMA’s medical home
In order to make our service better, we want to know when you have a problem. When you contact SETMA for any reason and by any means -- appointment, refill, referral request, question or another issue -- always get the name of the person with whom you spoke.
In the event that you have a problem, this will help us identify any issues on our end and improve our service. If you do have a problem of discourteous, rude or improper behavior with or from someone, you can ask to speak to their supervisor. Once again, you should have your contacts name so you can reference this with their supervisor.
SETMA works hard to response in a timely and appropriate way to all telephone calls. Many days SETMA receives more than 3,000 phone calls from our patients. Please be patient with us, as we try to keep wait times to at a minimum while still giving care to each person. If you get a voice mail, you will be instructed to leave your number and information. You will also be given a number to call if you do not receive a return call within two hours. This number will connect you with one of SETMA's management staff who will make sure your needs are met.
Patient Satisfaction – Consumer Assessment of Healthcare Providers and Systems (CAHPS)
SETMA measures patient satisfaction in three ways:
- SETMA’s internal patient satisfaction survey
- The Patient-Centered CAHPS survey which is done by an independent vendor
- The HCAHPS Survey which is done through the hospital by an independent vendor
For over ten years, SETMA has ask you to complete “patient satisfaction surveys . We have taken your responses seriously. SETMA’s Executive Management reviews these surveys and distributes them to providers. We compare results over time to see if we are learning from what you are telling us.
In April, 2014, SETMA will formally receive the NCQA Distinction in Patient Experience Reporting. The National Committee for Quality Assurance (NCQA developed the optional Distinction in Patient Experience Reporting to help practices capture patient and family feedback through the newly developed Consumer Assessment of Healthcare Providers and Systems (CAHPS) Patient-Centered Medical Home (PCMH) Survey. Because consumer experience is a critical component of quality of care, giving more prominence to patient engagement is a crucial change to the PCMH program.
The CAHPS PCMH Survey assesses several domains of care:
- Access
- Information
- Communication
- Coordination of care
- Comprehensiveness
- Self-management support and shared decision making.
Sine 2010, SETMA has been an NCQA PCMH-Recognized practice and in September, 2013 began using the CAHPS PCMH survey tool to obtain the new NCQA Distinction in Patient Experience Reporting. The survey is completed by an NCQA recognized vendor who sends out letters to a statistically significant sample of SETMA patients. The letters are then followed up with telephone calls. The completion of this survey involves more than 100 questions. This represents a significant commitment of time by SETMA’s patients and we are grateful to those who take the time to participate in this process. It gives SETMA providers critically important information on how they can improve the care patients receive.
At the next reporting period, April, 2014, SETMA will receive the NCQA’s Distinction in Patient Experience Reporting. This will help the healthcare community as submitted data will be used to develop a benchmarking database that will allow comparison across practices. As SETMA and other healthcare providers work to improve the quality of care everyone receives, these benchmarks are critical.
HCAHPS – Hospital Consumer Assessment of Healthcare Providers and Systems
In July, 2013, SETMA devised a plan for improving our results on the patient satisfaction of the care they receive in the hospital. Hospitals are required to employ an independent contractor to complete the HCAPHS survey oh patient satisfaction of that care. Historically, physicians did not know what the standards were for the HCAHPS survey. Starting in 2014, hospitals reimbursement is dependent a number of factors, one of them is providers HCAHPS scores.
There has been on the part of providers a sense of futility as the standard required on the HCAPHS survey is extraordinarily high and the judgment of whether or not a provider meets that standard is totally subjective on the part of the patient and/or patient’s family.
SETMA’s determined to improve our patient’s hospital experience and to do that in a systemic and sustainable fashion. SETMA is determined to solve this problem in a manner which will contribute to the quality of care all of our patients receive. As a result, SETMA learned the elements of the HCAHPS survey and added those to the Care Coaching Call SETMA’s Care Coordination Department makes to the patient the day following discharge from the hospital.
This is SETMA’s medical home; this is your medical home. Use your medical home; learn from it. Get involved in your own care; you and your heath will benefit.
The following documents which explain medical home are available on SETMA’s website at ”http://jameslhollymd.com/your-life-your-health/medical-home
NCQA’s New Distinction in Patient Experience Reporting
SETMA’s Meaningful Use Two Dilemma Part II
SETMA’s Meaningful Use Two Dilemma Part I
Lessons from a Tree: Excellence Medicine as a Provider or Patient
How Our Healthcare System Evolved and How It Must Change: Patient-Centered Medical Home
The Conversation Project
The Familiar Physician Contrasted with SETMA’s Experience Part II
The Familiar Physician Contrasted with SETMA’s Experience Part I
Citadel - A 1937 Introduction to the Spirit of Patient-Centered Medical Home
Paternalism or Partnership: The Dynamic of the Patient-Centered Transformation
Healthcare Transformation: Dynamic and Documents
Evidence-Based Medicine versus Alternative Medicine
Is Unlimited Primary Care the Goal or Even Possible?
Lessons from the African Ship of Hope
SETMA's 18th Anniversary: August 1, 1995 - August 1, 2013
Improving the quality of healthcare; why not cheat?
The Convergence of Public Health: Ethics, Primary Care and Routine HIV Testing in Healthcare
Transitions of Care: Handing Off Care to an Activated Patient
Improving Patient Care by Automating Care, Improving Patient Satisfaction and Care and Reducing Healthcare Provider Stress
Improving the quality of healthcare; why not cheat?
Being Accountable For Good Preventive Care
Provider Payment Reform: Incentives to Improve Care
The Future of Collaboration Between Physicians and Nurses
Medicare Preventive Services: Initial Preventive Physical Exam & Annual Wellness Visit
Transitions of Care Management Coding: SETMA’s Preparation and Solutions
Continuous Professional Development: Learning from a Convergence of Events
Patient and Family Engagement: Part I
The Paradoxical Commandments of Leadership and Healthcare
A Developmental History of SETMA Chapter 1 Part 2 Team Building
Problem List Reconciliation: The Tools Required to Facilitate the Maintenance of a Current Valid and Complete Chronic Problem List in an EMR-Part I
Robert Wood Johnson Foundation Site Visit Team
Southeast Texas Medical Associates, LLP: August 1, 1995 - July 31, 2012
HIMSS Innovation Committee and Introduction
SETMA’s Response to the Robert Wood Johnson Foundation: Part VI The Primary Care Team Learning from Effective Ambulatory Practices
SETMA’s Response to the Robert Wood Johnson Foundation: Part V The Primary Care Team Learning from Effective Ambulatory Practices
SETMA’s Response to the Robert Wood Johnson Foundation: Part IV The Primary Care Team Learning from Effective Ambulatory Practices
SETMA’s Response to the Robert Wood Johnson Foundation: Part II - The Primary Care Team Learning from Effective Ambulatory Practices
SETMA’s Response to the Robert Wood Johnson Foundation: Part I - The Primary Care Team: Learning from Effective Ambulatory Practices
Hospice Palliative Scales Part II
Hospice Palliative Scales Part I
STARs Program and SETMA’s Solution Part II
STARs Program and SETMA's Solution
Patient-Centered Medical Home Annual Questionnaires
Core Measures: Baptist Hospital of Southeast Texas
Preventable Readmissions: Predictive Modeling, Nurse Practitioners and Changes in Models of Healthcare Delivery
SETMA Featured in National Publication - "A Portrait of Health"
Can America’s Healthcare Problems be Solved?: Part I - How?
Healthcare Quality Award 2012 - Part VI: Demonstrated Results on Publicly Reported Performance Measures
Healthcare Quality Award 2012 - Part V: Data-Driven Improvement in the National Quality Strategy Priority Goal Areas
Healthcare Quality Award 2012 Part IV - Data-Driven Improvement in the National Quality Strategy Priority Goal Areas
Healthcare Quality Award 2012 Part I - Priorities for Performance Improvement
Medical Home Series Two: Part XVIII - Introduction to SETMA’s 2009, 2010 and 2011 Series of Articles on Medical Home
Medical Home Series Two: Part XVII - SETMA’s Model of Care & Patient-Centered Medical Home
Medical Home Series Two: Part XVI - Quality Metrics in the Medical Home
Medical Home Series Two: Part XV - The SETMA Foundation
Medical Home Series Two: Part XIV - Medication Reconciliation: AMA, NQF, ISMP
Medical Home Series Two: Part XI - Continuation of Quality, Coordination and Cost of Care
Medical Home Series Two: Part X - Quality, Coordination and Cost of Care
Medical Home Series Two: Part IX Telling The Truth and Collaboration
Medical Home Series Two: Part VII Care Coordination
Medical Home Series Two: Part VI Care Transitions
Medical Home Series Two: Part V Continuity of Care
Medical Home Series Two: Part IV A Metaphor for Medical Practice
Medical Home Series Two: Part III The Baton
Medical Home Series Two: Part II The Caution Lights
Medical Home Series Two: Part I The Movie
Texas State Reportable Infectious Diseases: A Systems Solution to the Problem of Reporting
Care Transitions: The Heart of Patient-Centered Medical Home - The Article
Over-diagnosis - THE Problem?
Business Analytics and Your AQ
Patient-Centered Medical Home and Care Transitions: Part II
Patient-Centered Medical Home and Care Transitions: Part I
2011 Gartner Business Intelligence Excellence Awards:SETMA A Semi-Finalist
SETMA: Practices in the Spotlight Medical Home and Diabetes Care
Reducing Preventable Readmissions to the Hospital
Accountable Care Organizations: What Is Required to Make Them Work?
SETMA HIMSS Stories of Success: Part II -- Improving Population Healthcare and Safety Through Real-time Data access, Auditing and Reporting
SETMA -- HIMSS Stories of Success:Part I -- Improving Population Healthcare and Safety Through Real-time Data access, Auditing and Reporting
Concierge Medicine and the Future of Healthcare
Patient-Centered Medical Home - Care Coordination and Coordinated Care
Address to the Beaumont Chamber of Commerce August 2000 Part II
Address to the Beaumont Chamber of Commerce August 2000 Part I
A Review of 2010 and a Projection for 2011
SETMA and the National Quality Forum
Re-Evaluating the Value of Members of the Healthcare Team
A New Day in Healthcare for You and for Us - Part V - Certified Electronic Health Records (EHRs)
A New Day in Health Care for You and for Us - Part IV - Are Quality Metrics a Good Part of the Future of Healthcare?
A New Day in Healthcare for You and for Us - Part III - Medical Home
Medical Home: Questions About Our Journey
Reporting of Health Care Provider Performance
The Place of Patient-Centered Medical Home in the Future of Healthcare Delivery
Medical Home Part X: A Summation of the Beginning of a Journey
Medical Home Part IX: Radical Changes in Healthcare Delivery
Medical Home Part VIII: Why is Medical Home Called Patient-Centered Medical Home?
Can More Care Provide Less Health?
Medical Home Part VII: Reporting of Quality Measures Performance
Medical Home Part VI: Evidenced Based Medicine Defines the Standard and the Structure of Care
Medical Home Part V: Healthcare Education and Delivery: Essential Changes Needed in Both
Medical Home Part IV: Help and Hope in Healthcare
Medical Home Part III: Requirement Number 1 of 28
Medical Home Part II: What is it?
Medical Home Part I: Is it the future of healthcare?
|